Back to Journals » Research Reports in Clinical Cardiology » Volume 14
The Magnitude of 30-Day Readmission and Factors Associated with Patients Underwent Cardiac Surgery in Tikur Anbessa Specialized Hospital Cardiac Center, Ethiopia
Authors Demissie DB , Doge G, Werba TB
Received 4 February 2023
Accepted for publication 29 April 2023
Published 17 May 2023 Volume 2023:14 Pages 35—48
DOI https://doi.org/10.2147/RRCC.S407183
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Kones
Dereje Bayissa Demissie,1 Gijo Doge,2 Teshale Biku Werba2
1Department of Neonatal Nursing, School of Nursing, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 2Department of Operating Theater Nursing, Schools of Nursing, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
Correspondence: Dereje Bayissa Demissie, Tel +251912189560, Email [email protected]; [email protected]
Introduction: Early hospital readmissions after cardiac operations are common, can vary from 7% to 21%, and are likely related to patient co-morbidity and perioperative care. Hospital readmissions are costly and potentially avoidable. Reducing hospital readmissions after cardiac surgery is necessary as part of the solution to improving efficiency in health care.
Methods: An institution-based retrospective chart review was conducted among 324 patients’ charts with the complete document from October 2013 to October 2020. The data were analyzed using SPSS. Both binary and multiple logistic regressions were run to identify associated factors at. PV< 0.05 with a 95% confidence interval (CI), which was considered statistically significant.
Results: The overall readmission rate was 8.0%. Fifty-one (15.7%) patients had mitral regurgitation history before surgery. About 207 (63.9%) patients were admitted with the preoperative diagnosis of chronic rheumatic valvular heart disease. Mitral valve (MV) replacement was done in 110 (34%), MV repair in 64 (19.8%), and atrial septal defect closure in 36 (11.1%). This study revealed that pericardial effusion was most common, accounting for 2.4%. Patients who were currently or ever smokers [adjusted odds ratio (AOR) 11.57, 95% CI (1.87– 75.16.6)], obese patients [AOR 14.0, 95% CI (1.11– 176.3)], and patients whose length of hospital stay (LOS) was 10– 14 days post-operatively [AOR 4.89, 95% CI (1.83– 13.06)] were identified as factors that increase the likelihood of 30-day readmission among patients who underwent cardiac surgery.
Conclusion: The magnitude of 30-day readmission after cardiac surgery in Tikur Anbessa Specialized Hospital Cardiac Centre, Ethiopia, was moderate, with identified factors of left ventricular ejection fraction, obese patients, history of smoking, history of dyslipidemia, postoperative LOS, and postoperative inotropic drug need all increasing the likelihood of readmission within 30 days after cardiac surgery. Therefore, policymakers and health planners would develop strategies and protocol guidelines to improve the quality of cardiac surgery and prevent readmission after cardiac surgery.
Keywords: magnitude, cardiac surgery, readmission, 30 days after cardiac surgery
Plain Language Summary
Reducing hospital readmissions after cardiac surgery is necessary as part of the solution to improving efficiency in health care. An institution-based retrospective chart review was conducted among 324 patients’ charts with the complete document from October 2013 to October 2020. The magnitude of 30-day readmission after cardiac surgery in Tikur Anbessa Specialized Hospital Cardiac Centre, Ethiopia, was moderate, with identified factors of left ventricular ejection fraction, obese patients, history of smoking, history of dyslipidemia, postoperative length of hospital stay, and postoperative inotropic drug need all increasing the likelihood of readmission within 30 days after cardiac surgery. Therefore, policymakers and health planners would develop strategies and protocol guidelines to improve the quality of cardiac surgery and prevent readmission after cardiac surgery.
Introduction
Cardiac surgery remains a significant function in treatment of different types of cardiovascular diseases, including the care of acutely and critically ill patients. Globally, around one million cardiac operations are performed yearly, including coronary artery bypass graft (CABG) and valvular surgery, accounting for the most frequently performed procedures.1 Although cardiac surgery has improved significantly over the past several years, postoperative hospital readmissions remain significant challenges after cardiac operations.2
A hospital readmission is a return to a hospital after an initial admission and release within a specific time limit.3
Readmission can happen in the same or a different hospital, and it might happen on purpose or by accident. Although no consensus has been achieved on what period to define readmission, policy analysts commonly refer to readmissions as hospital admissions occurring within 7, 15, or 30 days of release from the index hospitalization. In rare cases, the period following discharge might be as long as 60, 90, or even a year.3,4 The Centers for Medicare and Medicaid Services (CMS), on the other hand, has set 30-day readmission rates as a quality indicator. Hospitals with higher-than-expected readmissions are subject to financial fines under the Affordable Care Act.5 Readmission rates globally are high and could be reduced through targeted intervention, but not all hospital readmissions are preventable.4 According to a study done in the United States (USA) and the United Kingdom (UK), different rates of potentially preventable readmissions within 30 days of hospital admission were revealed. In the UK, the emergency 30-day readmission rate between 2004 to 2010 was 7% compared to 2% in the USA.6 Readmissions are a significant problem after both surgical and medical admissions, and recent policy changes that include substantial financial penalties have made readmissions pay for performance programs for health care in developed countries.7 Global readmission rates vary from 10% to 25%.4
Readmission rates for patients hospitalized after CABG surgery is 16.5%, and 1 in every 5 patients are readmitted within 30 days. In the study of Medicare fee-free service beneficiaries discharged from the Hospital in 2003 and 2004, only 10% of the patients were readmitted.5,6 About 7.8 million (20%) of patients discharged from hospitals in the USA alone were readmitted, accounting for $17.4 billion of hospital payment.8
Hospital readmissions within a short period after the initial admission contribute significantly to the overall cost of health care in the USA; early readmission to the hospital after cardiac surgery is a significant concern for patients and their families and health-care providers. Readmissions within a short period contribute significantly to the overall cost of health care in the USA.9,10
Unplanned 30-day hospital readmissions account for significant health-care costs, especially among postoperative cardiac patients. Preventing readmissions is now a priority for hospitals and health systems because of the Hospital Readmissions Reduction Program (HRRP). A study found that hospitals with low readmission rates also had low mortality rates.1,4,7,11–14
Readmission within 30 days of hospital admission can be costly for patients and their families, and according to Polites et al, risk markers of 30-day readmission are more common in patients with stress and high stress was associated with a threefold increased risk of re-admittance.7,15 Formulation of policies such as substantial penalties makes readmission a more significant concern for health care in developed countries. Preventing readmissions is now the priority for hospitals and health-care systems because of HRRP implementation by the CMS and hospitals whose readmissions exceed the national 30-day risk-adjusted all-cause readmission rates will impose some penalties on those hospitals.16 In developing countries with low income, access to cardiac surgery is very expensive and not easily available. Data on the magnitude and associated factors of 30-day hospital readmission in patients who underwent cardiac surgery are minimal.16,17 In Egypt, early hospital readmission after cardiac surgery is common and accounts for 8–24%, whereas in Ghana overall readmission rate was 3.1%.2 In Ethiopia, patients who underwent cardiac surgery are currently discharged to home with a follow-up phone call on discharge after cardiac surgery. However, there is no information or study conducted on the 30-day readmission after discharge among patients who underwent cardiac surgery in Cardiac Centre – Ethiopia. Therefore, this study seeks to determine the magnitude and associated factors of 30-day readmission among patients who underwent cardiac surgery.
Methods
Study Area and Period
The study was conducted among patients who had undergone cardiac surgery in Tikur Anbessa Specialized Hospital Cardiac Centre, Addis Ababa, Ethiopia, from April to June 2021.
Inclusion and Exclusion Criteria
All patients who had undergone open-heart surgery between October 2013 and October 2020 in a teaching hospital in Tikur Anbessa Hospital Cardiac Center, Ethiopia, and readmitted to the Hospital during the first 30 days after surgery whose charts were available or complete were included in the study, while all patients who had undergone cardiac surgery’s charts not containing full information or incomplete in major variables such as diagnosis cardiac surgery’s, 30-day readmission history according to the checklist, and percutaneous coronary intervention were excluded.
Study Design
A retrospective chart review was conducted in Tikur Anbessa Special Hospital Cardiac Center, Ethiopia.
Sample Size Determination and Sampling Technique
The sample size for the study was calculated using the single-population proportion formula, and the 50% prevalence was used to calculate the sample size. The total number of patients operated on from October 2013 to October 2020 was 996. Using the correction formula as considering refusal rate as 15% the final sample size was 324. Each year, patients were counted, and the total sample size (n = 324) was allocated proportionally.
Data Collection Methods and Techniques
The study was conducted based on patients’ records from Black Lion Specialized Hospital Cardiac Center, Ethiopia. Four trained clinical nurses collected the data by using a structured checklist. The checklists included basic demographic data including age, sex, residence, clinical, diagnostic, and laboratory findings prepared based on Black Lion Hospital Cardiac Center, Ethiopia, chart registration. The research assistans or data collectors were qualified nurses involved in daily patient care management. The training was given to them on checklists and documentary reviews. The pre-testing of the checklist was done in Addis Cardiac Center in April 2021 using the 5% of the sample size. The checklist was examined for clarity and ambiguity, and time is taken to fill them. The checklist was adapted from similar studies based on the objects of study. The required data was collected by getting permission from the institution. First, the principal investigator has described the purpose of the study.
Quality Control for the Research
Data quality was assessed using a number of measures, including pre-testing and training of data collectors, supervision by the principal investigator and checking the completeness and internal consistency of data during and after data collection and entry. Data cleaning was done by running the frequencies of each variable.
Statistical Analysis
The returned checklist was checked for completeness, cleaned manually, coded and entered into EPI INFO 7.1.6 version, and then transferred to SPSS version 23 for further analysis. Frequencies, percentages, mean and standard deviation were used to summarize the descriptive statistics of the data, and the chi-square test was used for categorical variables.
Both binary and multiple logistic regressions were run to identify associated factors at P < 0.05 with 95% confidence interval (CI) tested between 30-day readmission and its predictors. Then the results were presented with text narration, graphs, figures, and tables.
Operational Definitions
Cardiac surgery, also known as cardiovascular surgery or heart surgery, treats many problems related to the heart and the blood vessels connected to it. Common types of heart surgery include CABG, valve repair or replacement, inserting a pacemaker or ICD, maze surgery, aneurysm repair, and a heart transplant.
Hospital readmission is an episode when a patient discharged from a hospital is admitted again within a specified time interval.
Thirty-day readmission is defined as readmission to the hospital for any reason within 30 days of discharge from the index hospitalization after cardiac surgery.
Discharge from hospital is when a patient leaves hospital and either returns to home or is transferred to another facility such as one for rehabilitation or a nursing home.
Body mass index (BMI) is a measure of where BMI falls within the underweight range (<18.5 kg/m2), middle range (18.5–25 kg/m2), overweight range (25.0–30 kg/m2), and obesity range (≥30.0 kg/m2).
Result
The complete response rate was 324/324/100%. Of the total study participants, 212 (65.4%) were women. The majority of the study participants (190 [58.6%]) were less than 18 years old, and 185 (57.1%) were from rural residents as shown in Table 1.
 |
Table 1 Socio-Demographic Information of Patients Who Underwent Cardiac Surgery at Tikur Anbessa Specialized Hospital Cardiac Center, Ethiopia (n = 324) |
History of Comorbidity
The client’s medical evaluation indicated the key co-morbidities that existed before surgery were documented, and the proportion of co-existing co-morbidities were as follows: 20 (6.2%) had a history of hypertension (HTN), 24 (7.4%) had a history of obesity as measured by a BMI >30 kg/m2, 11 (3.4%) had dyslipidemia, 115 (36.6%) had mitral regurgitation (MR), and 49 (15.6%) had chronic (shown in Table 2).
 |
Table 2 Comorbidity History of Patients Who Underwent Cardiac Surgery at Tikur Anbessa Specialized Hospital Cardiac Centre, Ethiopia (n = 324) |
Surgical Characteristics of Participants
Of the total number of patients who underwent cardiac surgery, 57 (18.2%) had mitral stenosis (MS) before surgery and 57 (18.2%) had heart failure symptoms before surgery. Of the total, 20 (6.4%) participants had an associated history of previous cardiac surgery and 296 (94.3%) participants underwent elective surgery; the leading type of surgery undergone was on-pump 298 (94.9%). Regarding the majority of preoperative diagnoses, 207 (63.9%) were due to chronic rheumatic valvular heart disease (CRVHD), followed by an atrial septal defect (ASD), followed by a ventricular septal defect (VSD). Regarding procedures performed, mitral valve (MV) replacement accounts for 110 (34.0%), followed by MV repair at 64 (19.8%), an ASD at 36 (11.1%), and a VSD at 25 (7.7%). The majority of procedures (299, 92.3%) were completed in less than 240 minutes. The majority (57.7%) of the procedure took between 3 and 4 hours; see details in Table 3.
 |
Table 3 Surgical History of Participants Who Underwent Cardiac Surgery at Tikur Anbessa Specialized Hospital Cardiac Center, Ethiopia (n = 324) |
Postoperative Patient Characteristics
The majority of the length of hospital stay (LOS) in days after surgery (n = 266, 75.2%) took less than 10 days; the mean pre-op hospital stay of pts time being 14 days (range: 7–14 days). About 48 (15.3%) patients needed postoperative inotropic drugs. Of the total, 100 (35.5%) patients have post-op atrial fibrillation present (Table 4).
 |
Table 4 Postoperative Characteristics of Patients Who Underwent Cardiac Surgery at Tikur Anbessa Specialized Hospital Cardiac Center, Ethiopia (n = 324) |
Magnitude and Reasons of 30-Day Hospital Readmission
The magnitude of 30-day readmission among patients who underwent cardiac surgery in Tikur Anbessa Specialized Hospital Cardiac Center, Ethiopia, was 26 (8%) which ranges with 95% CI from 5.2% to 11.1% (Figure 1).
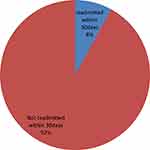 |
Figure 1 Magnitude of 30 days of readmission after cardiac surgery in Tikur Anbessa Hospital Cardiac Center, Ethiopia, 2021. |
The most important details in this text are that 4.6% of the cardiac patients readmitted were aged 19–40 years, while 3.4% were under the age of 18. Thirteen of 212 female patients (4.0%) were readmitted, with an equal percentage of males (112; 4%). Two of 20 hypertensive patients (0.6%) were readmitted compared to 24 of 318 (7.4%) non-hypertensive patients. One of 24 obese patients with a BMI >30 kg/m2 (0.3%) was readmitted. Four of 11 patients with a history of dyslipidemia were readmitted compared to 22 of 313 patients without a history of dyslipidemia. Three of 10 patients with a smoking history were readmitted compared to 23 of 314 patients without a history of readmission. The most common causes of readmission were pericardial effusion (2.4%), bleeding (2.2%), tamponade (2.2%), stacked MV (0.6%), pericarditis (0.6%), and pulmonary artery pressure (0.3%).
Reasons for 30-Day Readmissions
The most important details revealed by Figure 2 are that 8.0% of the 26 readmitted patients after cardiac surgery were readmitted within 30 days after hospital discharge due to complications such as pericardial effusion, bleeding or lemonade, Stack MV, pericarditis, and pulmonary artery HTN; see details in Figure 2.
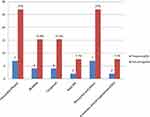 |
Figure 2 Reasons of 30-day readmission among patients underwent cardiac surgery at Tikur Anbessa Hospital Cardiac Center, Ethiopia, 2021. |
Factors Associated with 30 Days of Hospital Readmission After Cardiac Surgery
Both binary and multiple logistic regressions were run to identify associated factors at a P value of 0.05 with a 95% CI, which was considered statistically significant. Based on the binary logistic stepwise logistic regression model for early readmission, the predictors to include in the model show those variables that were selected for the final model. At binary logistic analysis, it was identified that candidate variables such as age, gender, history of HTN, history of MS, history of chronic atrial fibrillation, MR), status of surgery, duration of cardiopulmonary bypass (CPB) in minutes (240 minutes), cross-clamp time, history of diabetes mellitus (DM), and type of surgery undergone were, respectively. The final mode multivariable analysis was used at P value of 0.05, and adjusted odds ratio (AOR) with 95% CI to identify associated with 30-day readmission after cardiac surgery is presented in Table 5.
 |
Table 5 Factors Associated with 30-Day Readmission After Cardiac Surgery in Tikur Anbessa Hospital Cardiac Center, Ethiopia, 2021 |
Obese patients (BMI ≥3 kg/m2) before surgery were 14 times [AOR 14.01; 95%Cl (1.11–17.3)] more likely to be readmitted within 30 days as compared to normal BMI.
Patients with a history of dyslipidemia were 18 times [AOR 17.96; 95%Cl (2.43–32.32)] more likely to be readmitted within 30 days after cardiac surgery compared to had not have dyslipidemia.
Patients with a history of left ventricular ejection fraction (LVEF) ≥40% were 7 times [AOR 7.018; 95% Cl (1.152–42.75)] more likely to be readmitted within 30 days after cardiac surgery compared to those who had less than 40% LVEF.
Patients with a history of smoking cigarettes were 12 times [AOR 12; 95% CI (1.78–75.16)] more likely to be readmitted within 30 days after cardiac surgery than nonsmokers.
Patients who had 10–14 days stayed postoperative in the hospital were 5 times [AOR 4.89;95% CI (1.83–13.064)] more likely to be readmitted as compared to those who had stayed postoperative less than 10 days.
Patients who had treated with postoperative inotropic drugs were 7 times [AOR 7.17; 95% CI (2.6–19.54)] more likely to be readmitted as compared to those not treated with post-op inotropic drugs, as shown in Table 5.
Discussion
According to this study, hospital readmission is an episode when a patient who has been discharged from a hospital is admitted again within a specified time interval. Thirty-day readmission is defined as readmission to the hospital for any reason within 30 days of discharge from the index hospitalisation after cardiac surgery. Decreasing 30-day readmissions was considered a target in health-care strategies aimed at reducing unnecessary costs and burden.
This study determined the magnitude of readmissions within 30 days among patients who had undergone cardiac surgery in Ethiopia was moderate (8%), compared to the USA, where the postoperative intensive care unit readmission rate varies widely from 5% to 13% of all admissions.18 This study was also consistent with the findings in the study conducted in the USA where 9.8% were reported to have 30 days of readmission following cardiac surgery.9 A study conducted in Iran in 2019 found that 30 days of readmission after open-heart surgery was 11.7%, which is nearly comparable to the present study.1 Similarly, a study in the UK between 2004 and 2010 reported that the 30-day readmission after discharge following cardiac surgery was 7%, which supports these findings.6 Moreover, a study conducted by Shajedur and reported that the 30-day readmission after discharge following CABG surgery was 12.9%, which is consistent with the present study.19 In the present study, more than half (65.4%) of respondents were female. This study was similar to the study conducted by Parvin, where 55.4% were female.1 However, contradicting to this study was the study conducted in Egypt where the majority of respondents were male (67.7%). The reason for this contradiction may be due to their sampling technique where convenience sampling technique was used compared to the simple random sampling technique in the present study.2 The average age of the patients in this study is very young compared to other countries, but there are evidences that supported findings that the younger versus older people have higher odds of readmission following index admissions due to differences in the type, pathophysiology, and health-care needs of chronic conditions. For example, the onset of heart failure in younger versus older people may indicate a higher severity and complexity of illness.20,21
Of the 324 patients in the overall surgery, none of them were admitted due to non-cardiac causes, and 100% were due to cardiac causes. After cardiac surgery, pericardial effusion (2.4%) was the most common cause of the 30-day readmission in the present study. This was followed by bleeding (2.2%), cardiac tamponade, (2.2%); Stack MV (0.6%), and pericarditis (0.6%). This study was not comparable with the study conducted by Harsh Mainier where pericardial effusion accounts for 18.5%.10 The reason for this difference may be due to their large sample size (n = 50,158) and the greater number of centers. Furthermore, a study in northern England analyzed the reasons for readmission within 30 days and found that arrhythmia, infection, and pericardial effusion were the most common reasons for readmission. In the current study, 2.2% of the patients were readmitted within 30 days due to cardiac tamponade. This study was slightly in line with the study conducted in Iran, where 8.9% of the readmissions were due to tampons.
This study identified factors that increase the likelihood of 30-day hospital readmissions among patients who had undergone cardiac surgery in Ethiopia, such as history of smoking, BMI, dyslipidemia, LVEF <40%, and LOS <10 days. These factors impose a burden on the health-care system because they frequently occur within a short period after discharge. Regarding predictors associated with 30-day readmission following cardiac surgery, Hannan et al retrospectively analyzed 30 days of readmission among patients who underwent CABG in New York and identified several significant predictors, of which one of them supports this finding. These factors include age, women, extensive aortic atherosclerosis, DM, postoperative renal failure, and longer lengths of stay. Except for the LOS, all predictors mentioned were not consistent with the present study.7
The current study revealed that BMI >30 kg/m2 was significantly associated with 30-day readmission which is supported by the previous study, ie, higher the BMI, greater are the chances of being readmitted to the hospital.3 BMI >40 kg/m2 was an independent predictor for readmission to the intensive care unit after cardiac surgery, and also other studies reported that BMI >30 kg/m2 negatively affects patients’ daily living activity, recovery from surgeries, and thus increases the possibility of readmission to the hospital.22 Similarly, this is in agreement with that of Mohammed et al, who proved this.
This study identified that prolonged LOS between 10 and 14 days postoperatively was associated with 30-day readmission after cardiac surgery which is in line with a study done on a similar population that revealed a positive correlation between length of stay and readmission in open-heart surgery patients was significantly associated with length of stay result in increasing the odds of readmissions within 30 days,8 and another study done in Canada revealed that the LOS between 7 and 14 days was associated with 30-day readmission.6 This study suggested that premature discharge may predispose to readmission, which was supported by the previous study.23 However, shorter admissions do not necessarily translate into a greater risk for readmission, due to the fact that more complicated patients, either medically or socially, require longer hospital stays. Earlier studies have also found that congestive heart failure, chronic obstructive pulmonary disease (COPD), DM, and longer LOS were independently associated with higher readmission rates.2 However, in the present study, congestive heart failure, COPD, and DM were not associated with 30-day readmission. The present study significantly associated postoperative inotropic drug use with 30-day readmission following cardiac surgery. This finding was consistent with the study conducted on prolonged inotropic infusion, which was a postoperative risk factor associated with readmission.5,24
Regarding smoking, numerous studies have shown it to be a strong risk factor associated with early readmission14 This is similar to the present study where smoking was one of the independent predictors associated with 30-day readmission. Furthermore, another study showed that smoking was significantly associated with readmission supporting the present study.25 t A persistently identified risk factor about LVEF in previous studies found that decreased LVEF was a risk factor associated with increased odds of readmission after cardiac surgery.4,12,25 This is in line with the present study where LVEF <40% was an independent predictor of 30-day readmission in patients who underwent cardiac surgery in Tikur Anbessa Hospital Cardiac Center, Ethiopia. Moreover, patients with dyslipidemia had a higher risk of readmission within 30 days after surgery in the current study (AOR 18.92; 95% Cl [3. 096–11.56]). The finding was consistent with a study in Saudi Arabia where patients with dyslipidemia were more likely to be readmitted (P = 0.04).26
Strengths
This study can serve as a baseline study done in Ethiopia for the first time on cardiac surgery readmissions and encourages further exploration of readmissions and risk factors for cardiac surgery. Give information on the 30-day readmission following cardiac surgery.
Limitation
- The retrospective cross-sectional study does not show a causal relationship and selection bias is not avoidable. Being secondary data, there may be data incompleteness.
- Since the study was conducted in a single center, it may limit the generalizability of the result.
Conclusion
The magnitude of 30-day readmission after cardiac surgery in Tikur Anbessa Specialized Hospital Cardiac Center, Ethiopia, was moderate, with identified factors that increase the likelihood of 30-day hospital readmissions among patients who had undergone cardiac surgery in Ethiopia, such as history of smoking, BMI, dyslipidemia, LVEF <40%, and LOS <10 days. These factors impose a burden on the health-care system because they frequently occur within a short period after discharge. The root causes and ramifications associated with 30-day readmissions after surgery is an important step in improving patient outcomes after cardiac surgery.
The authors suggest that improving postoperative comorbidities and preventing major postoperative complications may decrease readmissions and improve the quality of cardiac surgery.
In light of these findings, the studies emphasize the need of planning multiprofessional perioperative treatment for elective heart surgery, as well as the idealization of risk factor reduction for 30-day readmissions. Providing health-care providers with information regarding readmissions, the relationship between clinical practice and hospital 30-day readmission rates may improve hospitals’ best practices. The study also would provide data to health-care workers; hospital administrators and other hospital leaders who can help them improve services patients and the hospital administrators may reduce cost. Therefore, policymakers and health planners would develop strategy and protocol guidelines to improve the quality of cardiac surgery to prevent readmission after cardiac surgery.
This finding provides evidence of within 30-day readmissions after surgery to health-care professionals, hospital managers, and other hospital executives who might assist them to improve the quality of care cardiac surgery, potentially lowering hospital expenditures.
- Health-care providers should identify high-risk patients, such as those with high BMI history, patients with LVEF <40%, patients with a history of smoking, patients with a history of dyslipidemia, at the head of surgery and all the necessary precautions should be taken.
- Health planners and decision-makers should develop strategies and guidelines to reduce 30-day readmission and improve the quality of care.
- Non-governmental organizations working in this area should participate in creating awareness in the community concerning 30-day readmissions after cardiac surgery.
For researchers
- Since this is a retrospective study, researchers are recommended to increase sample size and conduct the prospective study using this study as a baseline.
Abbreviations
ASD, atrial septal defect; BMI, body mass index; CABG, coronary artery bypass graft; CPB, cardiopulmonary bypass; CRVHD, chronic rheumatic valvular heart disease; CI, confidence interval; DM, diabetes mellitus; HTN, hypertension; LVEF, left ventricular ejection fraction; LVOTO, left ventricular outlet tract obstruction; MR, mitral regurgitation; MS, mitral stenosis; PDA, patent ductus arteriosus; OR, odds ratio; USA, United States of America; UK, United Kingdom.
Data Sharing Statement
Datasets used in the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from St. Paul Hospital Millennium Medical College Ethical Review Board Ref. No. Pm23/599 This requirement was not waived by the Institutional Review Board. NB: Written informed consent from the legally authorized representatives of the patient prior to study initiation was obtained from Black Lion Special Hospital Cardiac Center, Ethiopia. After getting ethical clearance, written permission was obtained from Black Lion Specialized Hospital Cardiac Center. The authors confirmed that informed consent was obtained from all subjects and/or their legal guardian(s), and informed consent was obtained from participants involved in the study. Finally, all methods were carried out in accordance with relevant guidelines and regulations. Study participants were recruited only after informed written consent was obtained from each of them. All the data were obtained anonymously and treated confidentially. All the procedures for data collection were conducted according to the principles of the Helsinki Declaration.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study obtained funding for data collection from St. Paul’s Hospital Millennium Medical College. The college had no role in the design of the study and collection, analysis, or interpretation of the data.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Ebrahimi P, Taghi Nattaj Darzi Naghibi M, Vatankhah S, Faghanzadeh GG. The relationship between performance indicators and readmission of patients with open heart surgery: a case study in Iran. Hosp Pract Res. 2019;4(2):62–67. doi:10.15171/hpr.2019.11
2. Abd-Elnabey SR, Elfeky HA, Badr SA. Readmission after cardiac surgery: study of predictors and frequency. Med J Cairo Univ. 2013;81(2):1–10.
3. Stone JL, Hoffman G. Medicare hospital readmissions: issues, policy options and PPACA. Congressional Research Service Washington, DC; 2010.
4. Dreyer R, Viljoen A. Evaluation of factors and patterns influencing the 30-day readmission rate at a tertiary-level hospital in a resource-constrained setting in Cape Town, South Africa. S Afr Med J. 2019;109(3):164–168. doi:10.7196/SAMJ.2019.v109i3.13367
5. Brown JR, Parikh CR, Ross CS, et al. Impact of perioperative acute kidney injury as a severity index for thirty-day readmission after cardiac surgery. Ann Thorac Surg. 2014;97(1):111–117. doi:10.1016/j.athoracsur.2013.07.090
6. Maali Y, Perez-Concha O, Coiera E, Roffe D, Day RO, Gallego B. Predicting 7-day, 30-day and 60-day all-cause unplanned readmission: a case study of a Sydney hospital. BMC Med Inform Decis Mak. 2018;18(1):1–11. doi:10.1186/s12911-017-0580-8
7. Hannan EL, Zhong Y, Lahey SJ, et al. 30-day readmissions after coronary artery bypass graft surgery in New York State. JACC Cardiovasc Interv. 2011;4(5):569–576. doi:10.1016/j.jcin.2011.01.010
8. Zhou H, Della PR, Roberts P, Goh L, Dhaliwal SS. Utility of models to predict 28-day or 30-day unplanned hospital readmissions: an updated systematic review. BMJ open. 2016;6(6):e011060. doi:10.1136/bmjopen-2016-011060
9. Kalateh SA, Bagheri Lankarani K, Tabrizi R, Rahnavard F, Zakerabasali S. Evaluation of 30-day unplanned hospital readmission in a large teaching hospital in Shiraz, Iran. Shiraz E Med J. 2017;18(4). doi:10.5812/semj.39745
10. Maniar H. Hospital readmissions after cardiac surgery: is it a game worth playing? J Thorac Cardiovasc Surg. 2015;149(3):858. doi:10.1016/j.jtcvs.2014.11.069
11. Edmondson D, Green P, Ye S, Halazun HJ, Davidson KW. Psychological stress and 30-day all-cause hospital readmission in acute coronary syndrome patients: an observational cohort study. PLoS One. 2014;9(3):e91477. doi:10.1371/journal.pone.0091477
12. Iribarne A, Chang H, Alexander JH, et al. Readmissions after cardiac surgery: experience of the National Institutes of Health/Canadian Institutes of Health research cardiothoracic surgical trials network. Ann Thorac Surg. 2014;98(4):1274–1280. doi:10.1016/j.athoracsur.2014.06.059
13. Kline LE. The effects of implementing best practices on 30-day readmission rates in adults following CABG surgery; 2015.
14. Spurling GK, Mansfield PR, Montgomery BD, et al. Information from pharmaceutical companies and the quality, quantity, and cost of physicians’ prescribing: a systematic review. PLoS Med. 2010;7(10):e1000352. doi:10.1371/journal.pmed.1000352
15. Polites SF, Potter DD, Glasgow AE, et al. Rates and risk factors of unplanned 30-day readmission following general and thoracic pediatric surgical procedures. J Pediatr Surg. 2017;52(8):1239–1244.
16. Bradley EH, Curry L, Horwitz LI, et al. Contemporary evidence about hospital strategies for reducing 30-day readmissions: a national study. J Am Coll Cardiol. 2012;60(7):607–614. doi:10.1016/j.jacc.2012.03.067
17. Silverstein MD, Qin H, Mercer SQ, Fong J, Haydar Z. Risk factors for 30-day hospital readmission in patients≥ 65 years of age.
18. Barnett SD, Sarin E, Kiser AC, et al. Examination of a proposed 30-day readmission risk score on discharge location and cost. Ann Thorac Surg. 2020;109(6):1797–1803. doi:10.1016/j.athoracsur.2019.09.048
19. Shawon MSR, Odutola M, Falster MO, Jorm LR. Patient and hospital factors associated with 30-day readmissions after coronary artery bypass graft (CABG) surgery: a systematic review and meta-analysis. J Cardiothorac Surg. 2021;16(1):1–15. doi:10.1186/s13019-021-01556-1
20. Greutmann M, Tobler D, Kovacs AH, et al. Increasing mortality burden among adults with complex congenital heart disease. Congenit Heart Dis. 2015;10(2):117–127. doi:10.1111/chd.12201
21. Ranasinghe I, Wang Y, Dharmarajan K, Hsieh AF, Bernheim SM, Krumholz HM. Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: a retrospective observational cohort study. PLoS Med. 2014;11(9):e1001737. doi:10.1371/journal.pmed.1001737
22. Chin DL, Bang H, Manickam RN, Romano PS. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff. 2016;35(10):1867–1875. doi:10.1377/hlthaff.2016.0205
23. Reynolds K, Butler MG, Kimes TM, Rosales AG, Chan W, Nichols GA. Relation of acute heart failure hospital length of stay to subsequent readmission and all-cause mortality. Am J Cardiol. 2015;116(3):400–405. doi:10.1016/j.amjcard.2015.04.052
24. Lazar HL. Glycemic control during coronary artery bypass graft surgery. Int Sch Res Notices. 2012;2012:14.
25. Sanaiha Y, Ou R, Ramos G, Juo -Y-Y, Shemin RJ, Benharash P. Day of discharge does not impact hospital readmission after major cardiac surgery. Ann Thorac Surg. 2018;106(6):1767–1773. doi:10.1016/j.athoracsur.2018.07.031
26. Alghafees MA, Alsubaie NA, Alsadoon LK, Aljafari SA, Alshehri EA, Suliman IF. Thirty-day readmission rates and associated risk factors after coronary artery bypass grafting. J Taibah Univ Medical Sci. 2020;15(4):292–297. doi:10.1016/j.jtumed.2020.05.004
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
