Back to Journals » Chronic Wound Care Management and Research » Volume 9
The Magnitude and Associated Factors of Diabetic Foot Ulcer Among Patients with Chronic Diabetic Mellitus in Northeast Ethiopia, 2021
Authors Atinafu BT , Tarekegn FN , Mulu GB , Kebede WM, Abinew Y , Mossie Y
Received 18 March 2022
Accepted for publication 13 July 2022
Published 26 July 2022 Volume 2022:9 Pages 13—21
DOI https://doi.org/10.2147/CWCMR.S364288
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Marco Romanelli
Bantalem Tilaye Atinafu,1 Fetene Nigussie Tarekegn,1 Getaneh Baye Mulu,1,2 Worku Misganaw Kebede,1 Yideg Abinew,3 Yalew Mossie3
1School of Nursing and Midwifery, Asrat Weldeyes Health Science Campus, Debre Berhan University, Debre Berhan, Ethiopia; 2Clinical and Psychosocial Epidemiology, Faculty of Medical Sciences, University of Groningen, Groningen, the Netherlands; 3School of Nursing and Midwifery, College of Health Sciences, Haramaya University, Harare, Ethiopia
Correspondence: Bantalem Tilaye Atinafu, School of Nursing and Midwifery, Asrat Weldeyes Health Science Campus, Debre Berhan University, Po. Box 445, Debre Berhan, Ethiopia, Email [email protected]
Introduction: Diabetic disease and its complications are major public health problems that result in long-term hospitalization, amputation, and poor quality of life for patients. This study aimed to determine the magnitude and associated factors of diabetic foot ulcers among patients with chronic diabetic mellitus in northeast Ethiopia.
Methods: An institutional-based cross-sectional study was conducted. The sample was selected using a systematic random sampling technique based on inclusion criteria. Data were collected using a self-administered pre-tested structured questionnaire. The collected data were entered into EpiData 3.1 and exported to SPSS 25 for statistical analysis. A binary logistic regression model was used to analyze the association between dependent and independent variables. All variables with P-value < 0.25 were included in multivariable logistic regression. Adjusted odds ratio at 95% confidence intervals and considered significant with P-value < 0.05 in final statistical significance was used to determine the level of association.
Results: The overall 283 samples of diabetic cases in the follow-up were included. The magnitude of diabetic foot ulcer was 7.1% (95% CI=3.92, 47.2%). Duration greater than 5 years (AOR=2.28, 95% CI=3.04, 17.69), history of ulceration (AOR=7.24, 95%, CI=1.25, 11.78), peripheral neuropathy (AOR=5.77, 95% CI=1.33, 12.155), oral hypoglycemic (AOR=3.2, 95% CI=4.02, 4.36) and insulin (AOR=2.6, 95% CI=1.75, 4.36) were found to be the significant factors of diabetic foot ulcer.
Conclusion: The magnitude of diabetic foot ulcer patients was 7.2% and associated with duration of diabetes mellitus, history of ulceration, peripheral neuropathy, and oral hypoglycemic medication. Therefore, attention is needed for prevention, early detection, and caring for foot ulcers.
Keywords: diabetes, magnitude, Ethiopia, foot ulcer, factors
Introduction
Diabetes mellitus is one of the top causes of micro-vascular and macro-vascular complications around the world. In 2019, around 463 million adults had diabetes, with this number anticipated to rise to 700 million adults by 2045.1 A diabetic foot ulcer is a long-term macro-vascular diabetic complication of diabetes mellitus. World Health Organization (WHO) reported in 2016, around 1.6 million diabetes mellitus complications due to diabetic foot ulcers with a lifetime incidence of foot ulcers occurring in one-fourth of diabetic people.2 According to the International Diabetic Federation, 9.1–26.1 million patients get DFU each year.3 The global and African prevalence of diabetic foot ulcer was 6.3% and 7.2% which was higher in males and type 2 diabetes mellitus respectively.4 Diabetes complications are more common in sub-Saharan Africa as a result of delayed diagnosis and inadequate case management.5,6
Diabetic foot ulceration has a significant cause of physical, psychological, and financial burden for both patients and healthcare sectors in patients with diabetes. It showed that a total of 15% of diabetic individuals face a lifetime risk and also around 20% of diabetic patients hospital admissions due to diabetic foot ulcers.4,7 Diabetic foot ulceration acts as an antecedent to the development of gangrene and lower limb amputation is carried out more than 20 times as frequently in people with diabetes than in those without diabetes if necessary care is not given. Although, once DFU has developed, there is greater chance of ulcer advancement which could lead to amputation. Furthermore, it is reported that every 30 seconds one leg is amputated due to DFU worldwide with more than 50% mortality rate after diagnosis. An increase in the number of individuals who have diabetic-related amputation makes the mortality rate worse than other several common cancers.8,9
Several studies reported that factors that contribute to development of diabetic foot ulceration were old age, duration of diabetes mellitus, poor self-care practice, and delay in medical attention typically in the setting of peripheral arterial disease, peripheral neuropathy, and trauma. In addition, the presence of comorbidities like ischemia from peripheral vascular disease, obesity, and hypertension act as fuel to develop.10,11
DFU is associated with significant mortality included from peripheral neuropathy, and early effective prevention, detection and caring through health education, controlling of blood sugar, and preventing trauma may improve severe complications and quality life of the patients.7 In developing countries like Ethiopia most complications of diabetic mellitus develop due to delayed diagnosis, high cost of treatment, and other related socio-economic problems. For example, the cost of DFU is estimated as one-third of the total cost of diabetic-related treatment.9,12 In Ethiopia, the magnitude and associated factor varies depending on sitting and time. Since there is no study in this area even if the fact that the disease is on the rise, this study is aimed to investigate the magnitude of diabetic foot ulcers and associated factors in the northeast part of Ethiopia.
Materials and Methods
Study Design, Study Area, and Study Period
An institutional-based cross-sectional study design was conducted to assess diabetic foot ulcers among patients with chronic diabetes at DBCSH from January–February. The study was conducted in Debre Berhan Comprehensive Specialized Hospital. It is located in North Shoa Zone, Amhara regional state, northeast part of Ethiopia. It is 130 km far from the capital city Addis Ababa, and 695 km far from the regional city Bahir Dar. The town has nine kebeles. According to data obtained from 2007 Central Statistics Agency of Ethiopia, Debre Berhan town has a total population of 108,825. There is one governmental referral hospital in the town.
Population
Source population was all patients with diabetes who have a diabetic follow-up in the diabetic clinic of DBCSH. The study populations were all patients with diabetes who were under follow-up at the DBCSH during the study period.
Sample Size Determination, Sampling Procedure, and Study Variables
The sample size was calculated using a single population proportion formula by considering the prevalence from a study done on diabetic foot ulcers in Felege Hiwot Referral Hospital Ethiopia at 21.2%23 at a 95% confidence level and a 5% margin of error. It gives an initial sample size of 257 by taking into consideration a 10% nonresponse rate; the final sample size was 283.
A systematic random sampling technique was employed to select study participants. The diabetes clinic runs twice weekly and there were about 565 patients with diabetes on follow-up taken from the diabetes mellitus outpatient clinic register. First, the total number of patients with diabetes patients was determined. Then, we got a total of 565 patients with diabetes mellitus. To get the final sample size, the interval was taken by dividing 565 by the final sample size (283). Then, we got Kth interval of two. Then, the first patient was selected randomly from the one or two by a lottery method, and the next patient was interviewed and examined in every second interval.
Dependent variable: Diabetic foot ulcer
Independent variables: Socio-demographic factors, Clinical characteristics, and Behavioral characteristics
Operational Definitions
Diabetic foot ulcers: These are non-traumatic lesions of the skin on the foot distal to malleoli of a person who has diabetes mellitus.
Gangrene: is a death of body tissue due to a lack of blood supply.
Fitting footwear: is footwear which is properly fitted to the patient who wears it with the absence of too tight, or too wide, high heel, poor quality, or hard leather.
Diabetic foot self-care practice: this means assessing the diabetic foot self-care practice of the patients. Based on the question and response of the study participants’ responses, mean will be used as a cutoff point to determine the level of self-care practice. Patients with DM who score less than the mean score are considered as poor foot self-care practice. Above the mean designated as “Good foot self-care practice”.
Peripheral vascular disease: palpate the posterior tibial artery and dorsalis pedis artery in both feet and record pulsations as absent or present.
Neuropathy (painful neuropathy): it was diagnosed if the patient had at least one manifestation from the following list of manifestations: describe sharp, stabbing, burning, shooting, or electric shock type pain, which may be worse at night and can disrupt sleep.
Inappropriate footwear: the shoes that are not appropriate with the shape and size of the shoe with the foot.
Data Collection Tools and Methods
The data were collected by using a data extraction tool adapted from different studies which consisted of socio-demographic, clinical, and behavioral characteristics factors. Interview and self-administered structured questionnaire were conducted. The questionnaires were first prepared in English language and translated to the local Amharic language to facilitate the data collection process. Finally, the questionnaires were re-translated to English by language experts for analysis purposes. Two BSC nurses and one MSC supervisor were involved in the data collection in a specific period.
Data Quality Assurance
To ensure the quality of the data the questionnaires were adapted from different published articles with some modification and checked by senior researcher and academician. Pretest on 5% was done before the actual data collection. The finding of the pretest was discussed among data collectors and supervisors to ensure a better understanding of tools and procedures so that it was modified for final data collection accordingly. The principal investigators and supervisors made day-to-day on-site supervision during the whole period of data collection and checked the collected data for completeness, clarity, and consistency on a daily basis. Both data collectors and supervisors were trained for two days on the data collection tool.
Data Processing and Analysis Plan
The collected data were cleaned, edited coded, entered into EpiData 3.1 software, and exported into SPSS version 25 for final analysis. Descriptive statistical analysis was computed to calculate means, standard deviations, frequencies, and percentages. Logistic regression analysis was performed separately to estimate the effects of each factor. Crude odds ratios (COR) and corresponding 95% confidence intervals were used to quantify an unadjusted strength of association between the independent and the outcome variables. Independent variables which result in a p-value less than 0.25 in bivariate analysis were candidates to be considered for the final multivariable model. During multivariable analysis, variables having a p-value <0.05 were taken as significant determinants of diabetic foot ulcers. Finally, the findings were presented by tables, figures, and narrations.
Results
Socio-Demographic Characteristics
A total of 283 diabetes mellitus follow-up clients participated in this study with a response rate of 100%. Of whom greater than half of the participants (55.8%) were females and their mean age was 55.32±29.27 years. Slightly more than half (55.5%) were living in rural areas and 59.4% were married. From total respondents, those who cannot read and write were 6.4% (Table 1).
 |
Table 1 Socio-Demographic Characteristics to Determine the Magnitude of Diabetic Foot Ulcer Among Chronic Diabetic Mellitus Patients at DBCSH Northeast Ethiopia, 2021 (n=283) |
Behavioral and Clinical Characteristics of the Respondents
More than two-thirds of participants, 230 (81.3%), were not made physical exercise and 261 (92.2%) were followed for the treatment of type II diabetes mellitus. Two hundred and forty-two (85.5%) of the respondents had good foot self-care practice. Around 26% of the respondents developed peripheral neuropathy. Regarding the treatment of medication, about 237 (83.7%) patients took oral hypoglycemia. Whereas, 24 (8.5%) patients took both insulin and oral hypoglycemia. Two-thirds of participants had more than 5-year duration with diabetes mellitus after diagnosis (Table 2).
 |
Table 2 Clinical and Diabetic Information of the Study Participants in DBCSH Northeast Ethiopia, 2021 (n=283) |
The Magnitude of Diabetic Foot Ulcer Among Study Participants
The magnitude of diabetic foot ulcers was 7.1% (95% CI=3.92, 47.2%). This study is based on Wagner’s classification of severity of the ulcer; the vast majority of the patients with diabetic foot ulcer were classified as grade 0. The magnitude of patients with diabetic foot ulcer in this study is shown in Figure 1.
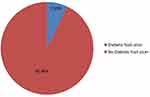 |
Figure 1 The magnitude of diabetic foot ulcer patients in DBCSH northeast Ethiopia, 2021 (n=283). |
Factors Associated with the Development of Diabetic Foot Ulcer
In bivariate analysis, sex, occupation, alcohol intake, duration of DM treatment, history of ulceration, peripheral neuropathy, and current medications were fitted at a p-value less than or equal to 0.25. These variables fitted at bivariate logistic regression analysis were entered into multivariate analysis. In multivariate analysis, duration on DM treatment, history of ulceration, peripheral neuropathy, and current medications were found to be significant factors for diabetic foot ulcer with a p-value less than 0.05 level of significance. Those who had the symptom of peripheral neuropathy disease were 6.23 times more likely to develop diabetic foot ulcers than those who had not peripheral neuropathy disorder (AOR=6.23, 95% CI=1.49, 26.003) (Table 3).
 |
Table 3 Bivariate and Multivariate Regression Analysis of Factors Associated with Diabetic Foot Ulcer Among DM Patients in DBCSH Northeast Ethiopia, 2021 (n=283) |
Discussion
Tthis cross-sectional study showed the magnitude and associated factors in the diabetic foot which gives clues to the magnitude and contributed factors in the study area. The overall magnitude of foot ulcers in diabetic patients was 7.1%. This is comparable with a similar study in Indian (8%),13 Pakistan (7.02%),14 and Norway (7.4%).15 Whereas, this finding is lower than the previous study done in the Harari region in Ethiopia (21.1%),2 Addis Ababa (20.7%),16 and Tanzania (15%),17 and higher than that of a study conducted in Dessie, Ethiopia (4.4%).18 The variation may be in different sample sizes and study design used, some were retrospective follow-up studies for a long time.
This study revealed that those diabetic patients who had peripheral neuropathy disease were 6.23 times more likely to develop diabetic foot ulcers as compared to those who had no peripheral neuropathy disorder (AOR=6.23, 95% CI=1.49, 26.003). This finding was supported by a study conducted in Gondar university hospital diabetes patients with peripheral neuropathy who were 21.76 times more likely to develop diabetic foot ulcer compared to those without.19 The other study in southern Ethiopia revealed that a presence of peripheral neuropathy was 4.48 times more likely to develop diabetic foot ulcer than those patients who had no peripheral neuropathy.20 In another case–control study done in Tikur Anbessa Hospital, Ethiopia patients with peripheral neuropathy were 7.56 times more likely to develop foot ulcers.21 A possible explanation is that in patients with peripheral neuropathy, the sensitivity and loss of vibration sensation significantly increases the risk of trauma, and the patient is unaware of the onset of sores/ulcers.
This study showed that patients with diabetes who take only oral hypoglycemic medication were 3.2 times more likely to develop diabetic foot ulcers than those patients who take a combination of oral hypoglycemic medication and insulin. Patients who took insulin only were 2.6 times more likely to develop diabetic foot ulcer than those patients who took a combination of oral hypoglycemic medication and insulin. This is supported by a case–control study done in Tikur Anbessa Specialized Hospital in Ethiopia patients who take a combination of oral hypoglycemic medication and insulin were 89% less likely to develop diabetic foot ulcers than patients who took insulin only.21
This study showed that patients who lived with DM for more than 5 years were 2.28 times more likely develop diabetic foot ulcer than patients who lived with DM for less than 5 years (AOR=2.28, 95% CI=3.04, 17.69). This is supported by a study done in Felege Hiwot referral hospital at Bahir Dar, Ethiopia that revealed that patients who follow for 6–10 years were 2.44 times more likely to develop DM complications than those who are living with DM for <5 years respectively.10 Another study conducted in the southern part of Ethiopia showed patients living with diabetes mellitus greater than 10 years were 1.91 times more likely to develop diabetic foot ulcer than patients living with diabetes mellitus for less than 5 years.20 A study in Sudan bared that diabetic patients who had follow-up for 5 years or more were 1.09 times more likely to develop DFU than those patients with DM for less than 5 years (AOR=1.09; 95% CI=1.05, 1.14).22 This is perhaps due to a diabetic person may have been exposed to hyperglycemic conditions for a lifetime, and cumulative glycemic load can have toxic consequences and affect any part of the body including skin and feet. Long-term hyperglycemia triggers a reaction between glucose and collagen, leading to the formation of advanced glycation end products.23
As a limitation, the nature of the cross-sectional study does not show the relation of causes and effects. There might be recall bias or reporting bias regarding the contributing factors, such as alcohol use or exercise frequency.
Conclusion and Recommendation
The study showed that the magnitude of diabetic foot ulcers among people with diabetes attending diabetic follow-up clinics at DBCSH was 7.1%. The major associated factor for DFU, history of ulceration, peripheral neuropathy, and current medication ware has a high contribution for DFU in this study. The study recommended that health education for patients and attendants should be provided regularly and further community-based and prospective follow-up studies will be beneficial to identify the clear incidence and prevalence of diabetic foot ulcers and to determine the potential risk factor of diabetic foot ulcers.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; DBCSH, Debre Berhan Comprehensive Specialized Hospital; DM, diabetes mellitus; DUF, diabetes foot ulcer; WHO, World Health Organization.
Data Sharing Statement
Data will be available upon request from the corresponding author.
Ethical Approval and Consent
Ethical clearance for the proposed study was obtained from School of Nursing and Midwifery, Asrat Woldeyes Health Science Campus, Debre Berhan University research ethical committee (DBU 070/21). A letter of cooperation was sent to the director of Debre Berhan Comprehensive Specialized Hospital, then to the department coordinators. The letters of informed consent granted by the School of Nursing, and Midwifery, and the purpose of the study were explained to the study participants. Then, the signed written informed consent was obtained from study participants. Confidentiality of the information was kept throughout the study by excluding the names of study participants as identification in the data collection form, and the data were used only for the proposed study. To maintain confidentiality, all collected data were coded and locked in a separate room before entering the computer. After entering the computer, the data were locked by password, and the data were not disclosed to any person other than the principal investigator. The study follows the declaration of Helsinki ethical principles.
Acknowledgment
First and foremost, all the praises and thanks to God for being with me all the time. We are grateful to Addis Ababa University, College of Health Science, School of Nursing and Midwifery, Department of Nursing for giving us a chance to conduct this research. We would like to thank the staff members who work in tertiary hospitals, data collectors, and card extractors.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. doi:10.1016/j.diabres.2019.107843
2. Tola A, Regassa LD, Ayele Y. Prevalence and associated factors of diabetic foot ulcers among type 2 diabetic patients attending chronic follow-up clinics at governmental hospitals of Harari Region, Eastern Ethiopia: a 5-year (2013–2017) retrospective study. SAGE Open Med. 2021;9:2050312120987385. doi:10.1177/2050312120987385
3. Everett E, Mathioudakis N. Update on the management of diabetic foot ulcers. Ann N Y Acad Sci. 2018;1411(1):153. doi:10.1111/nyas.13569
4. Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med. 2017;49(2):106–116. doi:10.1080/07853890.2016.1231932
5. Tadesse Tolossa BM, Mulisa D, Fetensa G, Turi E, Abajobir A. Prevalence and associated factors of foot ulcer among diabetic patients in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2020;20(41):1–4.
6. Armstrong DG, Boulton AJ, Bus SA, Ingelfinger JR. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367–2375. doi:10.1056/NEJMra1615439
7. Leila Yazdanpanah MN, Adarvishi S. Literature review on the management of diabetic foot ulcer. World J Diabetes. 2015;15:37–53. doi:10.4239/wjd.v6.i1.37
8. Mairghani M, Elmusharaf K, Patton D, et al. The prevalence and incidence of diabetic foot ulcers among five countries in the Arab world: a systematic review. J Wound Care. 2017;26(Sup9):S27–S34. doi:10.12968/jowc.2017.26.Sup9.S27
9. Meza-Torres B, Carinci F, Heiss C, Joy M, De Lusignan S. Health service organisation impact on lower extremity amputations in people with type 2 diabetes with foot ulcers: systematic review and meta-analysis. Acta Diabetol. 2021;58:1–13.
10. Lebeta R, Argaw Z, Walle B. Prevalence of diabetic complications and its associated factors among diabetes mellitus patients attending diabetes mellitus clinics; institution based cross sectional study. Am J Health Res. 2017;5(2):38. doi:10.11648/j.ajhr.20170502.13
11. Yazdanpanah L, Nasiri M, Adarvishi S. Literature review on the management of diabetic foot ulcer. World J Diabetes. 2015;6(1):37.
12. Wagnew F, Eshetie S, Kibret GD, et al. Diabetic nephropathy and hypertension in diabetes patients of sub-Saharan countries: a systematic review and meta-analysis. BMC Res Notes. 2018;11(1):1–7. doi:10.1186/s13104-018-3670-5
13. Nagaraj C, Ramakuri M, Konapur KS. Burden of foot problems in diabetic subjects-a community-based study among urban poor in Bangalore, India. Education. 2014;48:73–85.
14. Younis BB, Shahid A, Arshad R, Khurshid S, Ahmad M, Yousaf H. Frequency of foot ulcers in people with type 2 diabetes, presenting to specialist diabetes clinic at a Tertiary Care Hospital, Lahore, Pakistan. BMC Endocr Disord. 2018;18(1):1–6. doi:10.1186/s12902-018-0282-y
15. Molvær AK, Graue M, Espehaug B, Østbye T, Midthjell K, Iversen MM. Diabetes-related foot ulcers and associated factors: results from the Nord-Trøndelag Health Survey (HUNT3) (2006–2008). J Diabetes Complications. 2014;28(2):156–161. doi:10.1016/j.jdiacomp.2013.10.010
16. Yimam A, Hailu A, Murugan R, Gebretensaye T. Prevalence of diabetic foot ulcer and associated factors among diabetic patient in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. J Africa Nurs Sci. 2021;14:100285. doi:10.1016/j.ijans.2021.100285
17. Chiwanga FS, Njelekela MA. Diabetic foot: prevalence, knowledge, and foot self-care practices among diabetic patients in Dar es Salaam, Tanzania–a cross-sectional study. J Foot Ankle Res. 2015;8(1):1–7. doi:10.1186/s13047-015-0080-y
18. Seid MA, Akalu Y, Gela YY, et al. Microvascular complications and its predictors among type 2 diabetes mellitus patients at Dessie town hospitals, Ethiopia. Diabetol Metab Syndr. 2021;13(1):1–8. doi:10.1186/s13098-021-00704-w
19. Tesfamichael G, Abebaw A, Tesfaye E. Prevalence of diabetic foot ulcer and associated factors among adult diabetic patients who attend the diabetic follow-up clinic at the University of Gondar Referral Hospital, North West Ethiopia. Diabetes Res Clin Pract. 2016;2016:1–18.
20. Asegid R, Befikadu T, Esekezaw A, Busera S. Magnitude of diabetic foot ulcer and associated factors among diabetic patients who attended diabetic follow-up clinics in Gamo and Gofa Zones, Southern Ethiopia. Int J Diabetes Clin Res. 2021;8(2). doi:10.23937/2377-3634/1410139
21. Woldemariam GT, Atnafu NT, Radie YT, et al. Determinants of diabetic foot ulcer among adult patients with diabetes attending the diabetic clinic in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia: unmatched case-control study. Diabetes Metab Syndr Obes. 2020;13:3739. doi:10.2147/DMSO.S265988
22. Abdelbagi OM, Musa IR, Altigani SA, Osman A, Adam I. Prevalence of diabetic foot amongst adults with diabetes mellitus in northern Sudan: a cross‐sectional study. Int J Clin Pract. 2021;75(12):e14892. doi:10.1111/ijcp.14892
23. Newton V. Key considerations for assessment and management of limited joint mobility in the diabetic foot. Diabet Foot J. 2012;16:108–114.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
