Back to Journals » Journal of Blood Medicine » Volume 12
The Level of vWF Antigen and Coagulation Markers in Hospitalized Patients with Covid-19
Authors Al Otair H, AlSaleh K, AlQahtany FS, Al Ayed K, Al Ammar H, Al Mefgai N, Al Zeer F
Received 15 May 2021
Accepted for publication 22 June 2021
Published 30 August 2021 Volume 2021:12 Pages 809—817
DOI https://doi.org/10.2147/JBM.S318940
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Martin H Bluth
Hadeel Al Otair,1 Khalid AlSaleh,2 Fatmah S AlQahtany,3 Khalid Al Ayed,1 Hessah Al Ammar,4 Noura Al Mefgai,4 Faisal Al Zeer5
1Department of Medicine, King Saud University Medical city (KSUMC), King Saud University, Riyadh, Saudi Arabia; 2Department of Medicine, Hematology/ oncology division, College of Medicine, King Saud University, Riyadh, Saudi Arabia; 3Department of Pathology, Hematopathology Unit, College of Medicine, King Saud University, King Saud University Medical City, Riyadh, Saudi Arabia; 4Department of Medicine, King Saud University, Riyadh, Saudi Arabia; 5College of Medicine, King Saud University, King Saud University, Riyadh, Saudi Arabia
Correspondence: Hadeel Al Otair
Department of Medicine, King Saud University Medical City, King Saud University, P.O. Box 2925(38), Riyadh, 11461, Saudi Arabia
Tel +966(1) 8066519
Fax +966(1) 4692365
Email [email protected]
Background: The coagulopathy of COVID-19 still awaits more clarification, and one approach that has not been investigated is to compare the hemostatic changes between COVID-19 and non-COVID-19 infected patients.
Objective: This study aims to study COVID-19 coagulopathy by measuring markers of endothelial injury and coagulation, including anticoagulants (TFPI, protein C, protein S, and AT) in COVID-19 patients and compare them with non-COVID-19 patients early in the course of the disease.
Methodology: This is an observational, prospective cross-sectional study comparing the levels of protein C, protein S, antithrombin (AT) III, clotting factor (F) VIII, von Willebrand factor (vWF) and coagulation screening tests (PT and a PTT), fibrinogen, D-dimer in COVID-19 patients admitted during the same time with non-COVID-19 infections. The demographic and clinical data of the patients were collected from electronic medical records during admission. Blood tests were extracted within 24 hours of admission for both groups.
Results: Fifty-four (66.7% males) consecutive COVID-19 patients and 24 (59% males) non-COVID-19 controls were enrolled in the study from October 2020 till December 2020. COVID-19 patients were significantly older than non-COVID-19 (57.7± 14.2 vs 50± 19.8 years, p= 0.005). Fibrinogen level was significantly higher in COVID-19 patients compared to controls (5.9± 1.48 vs 3.9± 1.57, p< 0.001). There was no statistically significant difference in the level of FVIII, protein C, S, ATIII, and D-dimer between the two groups. The level of vWF Ag was statistically higher in COVID-19 patients (276.7± 91.1 vs 184.7± 89.4, p=0.0001). There was significant thrombocytopenia and lymphopenia among COVID-19 patients. Inflammatory markers, CRP, ferritin, and LDH, were increased in COVID-19 patients compared to non-COVID-19, but the difference was not statistically significant. High fibrinogen and vWF AG levels were the two independent variables found in COVID-19 patients.
Conclusion: The level of vWF Ag is increased early in the course of COVID-19 infection. This can be used as a biomarker for endothelial injury, which is peculiar to COVID-19 infection.
Keywords: COVID-19, vWF, fibrinogen, coagulopathy, endothelium
Introduction
Coronavirus disease (COVID-19) started in Wuhan, China, as multiple cases of pneumonia of unclear cause.1–3 On 11th March 2020, WHO declared COVID-19 as a pandemic after affecting more than 118,319 patients globally.4 Currently, more than 127 million cases are confirmed worldwide with 2,799,030 deaths.5 In the Kingdom of Saudi Arabia, the total number of cases has reached 388,860 with 6656 deaths, according to the last report (29th March 2021) from the Saudi Ministry of Health and the Saudi Centre of Disease Prevention and Control (CDC).6
It is well known now that severe acute respiratory syndrome corona virus2 (SARS-CoV-2) utilizes angiotensin-converting enzyme 2 (ACE2) receptor to enter human host cells.31 Specifically, SARS-CoV-2 surface spike protein binds to human ACE2 on the surface of the cell through its receptor-binding domain (RBD) which is activated by transmembrane protease serine 2 (TMPRSS2). This in turn induces virus-plasma membrane fusion and subsequent cell entry. Therefore, it plays a fundamental role in SARS-CoV-2 cellular infectivity as well as reduced viral recognition by neutralizing antibodies. Its expression by endothelial cells of the respiratory and digestive tracts explains many of the clinical presentations of COVID-19 infection.32–34
Patients with DM have an upregulation of ACE2 expression (total and glycosylated forms) on the surface of the cells secondary to the renin-angiotensin system activation.35 This contributes to the higher prevalence and worse prognosis of COVID-19 infection in patients with type 2 DM in conjunction with microvascular damage and overt inflammation mediated by high plasma levels of IL-6 and other pro-inflammatory cytokine.36
Similarly, the higher binding of COVID‐19 and ACE2 could explain the higher rate of hypertension among patients infected with covid-19 and their complicated course. ACE2 is a known modulator of the renin-angiotensin system (RAS) and responsible for many of the pathways underlying hypertension.37
Recently, many papers have reported an increased prevalence of venous and arterial thrombosis in COVID-19 patients.7–10 This is especially true in patients with non-O blood groups who have higher risk for arterial and venous thrombosis. Possibly related to alteration in hemostatic markers, vWF and FVIII, and over-inflammation.38
Similarly, postmortem studies have demonstrated the presence of widespread multiple microthrombi.11 Pulmonary embolism and deep vein thrombosis have also been reported in-69%of critically ill patients.9
During the last year, COVID-19 coagulopathy has been the subject of numerous publications, and it is now well established that the laboratory findings in COVID-19 coagulopathy are quite different from the usual findings of disseminated intravascular coagulation (DIC) seen commonly in septicemia.12,13
In hospitalized COVID-19 patients, the most observed abnormalities are elevations of plasma fibrinogen and D-dimer, along with a parallel rise in markers of inflammation (eg, CRP and cytokines), and minimum prolongation of prothrombin time (PT), activated partial thromboplastin time (aPTT), thrombin time (TT) and mild thrombocytopenia (platelet count ~100 x109/L).14,15 This does not fit in the findings noted in classical DIC.16
These unique features of COVID-19 have been researched extensively in the last few months, and no consensus on its pathophysiology has been reached. A recent article in Nature has described it rightly as the COVID-19 mystery.17,18
With this background in mind, we conducted a cross-sectional study to explore the mechanism of clot formation in COVID-19, specifically the level of clotting factor (F) VIII, von Willebrand factor (vWF), and natural anticoagulants in COVID-19 infection on admission to the hospital and compared it to the non-COVID-19 patients. We believe this approach of comparing markers of endothelial injury and coagulation between patients with COVID-19 pneumonia and bacterial pneumonia would bring out differences in the coagulopathy between these two groups of patients and thereby shed some light on the peculiar mechanism of the COVID-19 coagulopathy and better understanding of its pathophysiology, which may pave the way for novel therapeutic and/or preventive measures to prevent this potentially fatal complication•
Materials and Methodology
This study is a cross-sectional prospective observational study comparing COVID-19 patients confirmed by positive real-time polymerase chain reaction rt-PCR test, Roche Light Cycler® 480, of nasopharyngeal swabs, and non-COVID-19 patients admitted at King Khalid University Hospital, Riyadh, Saudi Arabia, between October 2020 and December 2020.
Informed consent was obtained from all patients or their next of kin for reviewing their electronic medical records and collection of blood samples for the laboratory coagulation tests. The study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Institutional Review Board of the College of Medicine-King Saud University, clinical trial number E-20-5099.
Patient Selection
The study included patients aged 18–80 years. We excluded incompetent or mentally disabled patients, oncology patients, pregnant or lactating women, patients known to have nephrotic syndrome and liver cirrhosis, and patients recently diagnosed with venous thromboembolism (<3 months) and those on anticoagulants.
For the control patients (non-COVID-19) two negative screening rt-PCR test and diagnosis of community-acquired pneumonia (ATS definition) was required for enrolment.19
Demographic and clinical data were collected from the patients’ electronic charts and recorded in a data entry form. These included age, sex, basal metabolic rate (BMI), smoking, comorbidities, medication, and clinical presentation for COVID-19.
The metrics for all the baseline laboratory investigations were collected from the system (HbA1C, D-dimer, CBC with differential count, serum ferritin, LDH, Cr, BUN, AST, ALT, Albumin, Bilirubin LDH and CRP).
Using a citrated tube, blood samples for natural coagulation factors inhibitors (Protein C, S, Antithrombin (AT) III) were extracted by the attending nurse, within 24 hours of admission, for both COVID-19 and non-COVID-19 patients. Samples were then transferred to Hematopathology Laboratory at King Khalid University Hospital.
Coagulation Tests
The performed assays included PT, aPTT, fibrinogen, D-dimer, quantification of coagulation FVIII, and physiological inhibitor proteins (protein C, free protein S, and AT). The PT, aPTT, and plasma fibrinogen assays were determined on the NeoPTimal using STA®, PTT A ⑤, Liquid FIB respectively and D-Dimer assay on the Liatest® D-Di PLUS. The Protein S, Protein C, antithrombin assays were determined on the Staclot, Stachrom, Stachrom ATIII STA®, respectively. The ristocetin cofactor activity of vWF-Rco was determined by vWF: RCo and vWF: Ag using Liatest ® vWF: Ag STA®.
Statistical Analysis
For descriptive and inferential statistical data analyses, Statistical Package for Social Sciences software, version 25.0 (IBM SPSS Inc., Chicago, IL), was used. Both descriptive and inferential statistics involving the Chi-square test and T-independent Test were used to present the results. For each test, a p-value of less than 0.05 was considered statistically significant. Multiple logistic regression analysis and ROC curves were used to identify the independent variable.
Results
Fifty-four (66.7% males) consecutive COVID-19 patients and 24 (59% males) non-COVID-19 controls were enrolled in the study, from October 2020 till December 2020. The control group patients were diagnosed with community-acquired pneumonia, and 6 of them had acute decompensated heart failure. Seven patients (7.4%) of COVID-19 patients died, 2 patients developed PE and one patient DVT during hospitalization. The severity of Infection with Covid 19 was moderate in 15 patients, severe in 20 patients who required high flow oxygen or CPAP. Out of nineteen patients (35%) admitted to ICU, seven were put on mechanical ventilation (37%), and eight patients received anti-IL-6 (tocilizumab) therapy. Blood group O positive was the predominant ABO phenotype in both Covid-19 and non-COVID-19 patients, 56% and 48%, respectively.
COVID-19 patients were significantly older than non-COVID-19 patients (57.7 + 14.2 years vs 50 ±19.8 years, p=0.005) and were more obese (BMI = 31.3 ±7.5 vs 25.7 ±6.9 kg/m2, P=0.003). Their mean Glycosylated Hb (HbA1C) was 7.69±2.1% (Table 1). Thirty-one patients (57%) of Covid-19 patients had type2DM and were on anti-hyperglycemic drugs, while 24 patients (44.4%) were hypertensive There were more smokers in the control group compared to the COVID-19 group (Table 2). There was no difference in comorbid conditions between the COVID-19 and non-COVID-19 groups apart from chronic lung disease, which was more common in the COVID-19 group (18.5% vs 0%, p=0.024) (Table 3). Forty-nine patients (90.7%) of COVID-19 patients versus 18 patients (75%) of controls received LMWH, enoxaparin for VTE prophylaxis, but the difference was not statistically significant (p=0.065). Additionally, the use of antiplatelets was similar among the 2 groups (22.2% vs 33.3%, p=0.3)(Table 3)
 |
Table 1 The Laboratory Result Values of COVID-19 Patients and Control Subjects |
 |
Table 2 Demographic Profile of Study Participants |
 |
Table 3 Comparison of Co-Morbid Conditions Between (COVID-19 Patients and Control Individuals) |
Laboratory Results
Plasma fibrinogen was significantly higher in COVID-19 patients compared to controls (5.9 ±1.5 vs 3.9 ±1.57, p=0.000). There was no statistically significant difference in the level of proteins C, S, ATIII between the two groups. Similarly, the level of FVIII, although it was elevated in both groups high, it did not differ significantly between the 2 two groups (196.8 ±83.3% vs 227.4±82.9%, p=0.138). However, the level of factor vWF AG was statistically higher in COVID-19 patients (276.7 ±91.01 vs 184.7 ±89.4, p=0.0001) (Table 1). There was a trend towards increased vWF activity in Covid-19 patients, but this did not reach statistical significance, probably due to the small sample size (191,5.31±68,8.18% vs 177.1 ±64.5%, p=0.08). The level of clotting FVIII was increased in COVID-19 as well as in non-COVID-19 patients, with no significant difference between the two groups (p=0.138).
There was significant thrombocytopenia and lymphopenia in the COVID-19 group, but there were no differences found in coagulation tests PT, aPTT, and D-dimers levels (Table 1). Inflammatory markers CRP, Ferritin in, and LDH were highly elevated in both COVID-19 and non-COVID-19 patients, but there was no statistical difference between both COVID-19 and non-COVID-19 patients (Table 1).
In the multivariate logistic regression analysis of the laboratory values, high fibrinogen and vWF: AG levels were the 2 independent variables found in COVID-19 patients (Table 4). Plasma fibrinogen (OR = 2.552; 95% CI= 1.2835.077; P <0.05) and vWF Ag (OR = 1.011; 95%) COVID-19 patients were used to generate ROC curves (Figure 1). The area under the ROC curve of 0.0.652 for age (P >0.05), of 0.738 for BMI (P <0.05), of 0.678 for smoking (P <0.05), of 0.309 for sex (P <0.05), of 0.202 for lymphopenia (P 5), of 0.797 for Hg (P <0.05), of 0.404 for PT (P <0.05), of 0.862 for fibrinogen (P < 0.05) and of 0.795 for VWF Ag (P <0.05) (Figure 1).
 |
Table 4 Multivariate Logistic Regression Analysis of the Laboratory Result Values Obtained from COVID-19 Patients and Control |
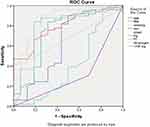 |
Figure 1 ROC curves for multivariate logistic regression models of significant variables among COVID-19-patients. |
Discussion
This study investigated some of the markers of endothelial dysfunction, coagulation factors, and level of natural anticoagulants early in the course of COVID-19 infection in comparison to non-COVID-19 patients admitted with community-acquired pneumonia CAP during the same time period. We found that the level of vWF Ag, which is a marker of endothelial injury, was significantly higher in COVID-19 patients than in bacterial infections. Its release following SARS-CoV-2 infection of endothelial cells leads to platelet activation and increased levels of FVIII. We also found an Increased level of D-dimer and fibrinogen early in COVID-19 infection. Our findings highlight the important role of endotheliitis in COVID-19 coagulopathy.
The high level of vWF Ag and activity may indicate that endothelial stimulation has taken place very early in the course of COVID-19, resulting in the release of vWF from the endothelium. This process is mediated by ACE2 receptors for SAR-Cov-2 on the surface of endothelial cells20 and contributes to the upregulation of fibrinogen and other procoagulants. This goes in parallel with the increase in the inflammatory markers IL6, ferritin, LDH. CRP and suggests that VWF can be a predictive marker of severe infection.21,39 The direct infection of the endothelial cells also leads to platelet activation and increased levels of VWF and FVIII, all of which contribute to thrombin generation and fibrin clot formation.22 The resultant endothelial cell activation can, to a great extent, explain the pulmonary microvascular thrombosis found in post-mortem examination of deceased patients with COVID-19,23,24 The level of FVIII in this study cohort of COVID-19 patients was increased early in the disease and the platelet count was mildly reduced.
Interestingly, the levels of natural anticoagulants (Pr C, S, ATIII) in COVID-19 patients were low normal but were not different from that found in patients with non-COVID-19 patients with CAP. This could indicate that depletion of natural anticoagulants occurs in both bacterial and viral infection at a later stage.
In addition, this study found that biomarkers of coagulation (such as D-dimer, fibrinogen, platelet count) were affected early in the COVID-19 infection. Previous studies reported that D-dimer could be used to differentiate between COVID-19 patients with severe versus mild disease.22,25
A cut-off value of D-dimer of ≥2 µg/mL (fourfold increase) within 24 hours after hospital admission was reported by Zhang et al to predict in-hospital mortality with a sensitivity of 92.3% and a specificity of 83.3%.26 Of note, the two study groups were not different in the anticoagulant agent used for VTE prophylaxis (Table 3); therefore, the changes noted in D-dimer, fibrinogen and coagulation factors were not related to the type of anticoagulant agent.
The increase in fibrinogen noticed early in COVID-19 infection helps differentiate bacterial sepsis or DIC from COVID-19 induced coagulopathy.27 Besides, the associated thrombocytopenia and prolonged activated partial thromboplastin time tend to be mild.18 This supports the theory that arterial thrombosis in COVID-19 is the result of direct endotheliitis caused by SARS-CoV-2 infection of endothelial cells through the two receptors of angiotensin-converting enzyme which results in disseminated microthrombosis, reactive endotheliitis and release of von Willebrand (vWF) multimers.18,39 This seems to be peculiar for COVID-19 and not shared with other viruses that present with decreased plasma fibrinogen concentrations, such as Ebola or Dengue, responsible for hemorrhagic fever and associated with the hypercoagulable state.28
In this study, the lymphocyte count of COVID-1919 pts was statistically lower than non-COVID-19 and occurred early in the disease. This is in agreement with previous studies that reported lymphopenia in 70.3% of hospitalized COVID-19 patients29 and can be considered as a biomarker of adaptive immune response and was found to be associated with COVID-19 severity.30
Limitations of This Study
Including the small sample size and being a single-center study, other inflammatory markers, eg, ferritin.IL 6 and procalcitonin were not compared among the two groups. Future studies in a larger number of patients are needed to confirm our findings and probably try to identify other soluble and cellular markers of early endothelial derangement. This will help to further reveal the role of endotheliitis in the procoagulant mechanism of SARs-cov2 infection, eg, plasma VWF propeptide (VWF pp).
Conclusion
Endothelial injury activation markers are increased early in COVID-19 infection, which is peculiar to COVID-19. The levels of VWF-Ag and fibrinogen are higher in COVID-19 infection than in non-COVID-19 bacterial infections.
We probably need to target endothelial injury in early COVID-19 to halt the activation of the coagulation system and consumption of natural anticoagulants and triggering of inflammatory response.
VWF Ag can be used as a biomarker for endothelial injury in COVID-19 early in the course of infection and may play a role as a prognostic indicator as demonstrated in other recent studies.
Ethics Approval and Consent to Participate
The research proposal for this study was approved by the Institutional Review Board (IRB) of the King Saud University, Riyadh Saudi Arabia (IRB Approval Project No. E-205099) for human studies. Informed consents were obtained from the subjects or authorized family representatives with strict confidentiality of information gathered. The study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
The authors are grateful to the College of Medicine Research centre and Deanship of Scientific Research, King Saud University (KSU), Riyadh; Saudi Arabia for support and funding.
Funding
This study was supported and funded by the College of Medicine Research Centre CMRC and the Deanship of Scientific Research of King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors of this paper have no conflicts of interest, including specific financial interests, relationships, and/or affiliations relevant to the subject matter or materials included.
References
1. Zhu N, Zhang D, Wang W, et al.; China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engle J Med. 2020;382(8):727–733. doi:10.1056/NEJMoa2001017
2. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239. doi:10.1001/jama.2020.2648
3. World Health Organization. A novel coronavirus (2019-nCoV). Situation report - 1. 2020.
4. World Health Organization. B Coronavirus disease 2019 (COVID-19). Situation report – 51. 2020.
5. World Health Organization. Coronavirus disease (COVID-19) weekly epidemiological update and weekly operational update. March. 2021.
6. Weqaya A. COVID-19-19 Daily Update of Cases. Riyadh, Saudi Arabia: Weqaya-Saudi Center for Disease Control and Prevention; 2021.
7. Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi:10.1016/j.thromres.2020.04.013
8. Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18(6):1421–1424. PMID: 32271988. doi:10.1111/jth.14830
9. Llitjos JF, Leclerc M, Chochois C, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020;22(10):1111.
10. Lodigiani C, Iapichino G, Carenzo L, et al. Humanitas COVID-19 task force. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. PMID: 32353746. doi:10.1016/j.thromres.2020.04.024
11. Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann Intern Med. 2020:M20–2003. PMID: 32374815.
12. Mucha SR, Dugar S, McCrae K, et al. Coagulopathy in COVID-19. Cleve Clin J Med. 2020. PMID: 3240943.
13. Becker RC. COVID-19 update: COVID-19-associated coagulopathy. J Thromb Thrombolysis. 2020;50(1):54–67. PMID: 32415579. doi:10.1007/s11239-020-02134-3
14. Görlinger K, Dirkmann D, Gandhi A, Simioni P. COVID-19-associated coagulopathy and inflammatory response: what do we know already and what are the knowledge gaps? Anesth Analg. 2020;131(5):1324–1333. PMID: 33079850; PMCID: PMC7389937. doi:10.1213/ANE.0000000000005147
15. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi:10.1111/jth.14768
16. Levi M, Jonge E, van der Poll T. de Sepsis and disseminated intravascular coagulation. J Thromb Thrombolysis. 2003;16(1/2):43–47. doi:10.1023/B:THRO.0000014592.27892.11
17. Callaway E, Ledford H, Mallapaty S. Six months of coronavirus: the mysteries scientists are still racing to solve. Nature. 2020;583(9):178–179. doi:10.1038/d41586-020-01989-z
18. Shalhub S. The mystery of COVID-19-associated arterial thrombosis. J Vasc Surg. 2021;73(2):390–391. doi:10.1016/j.jvs.2020.08.022
19. Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J. Diagnosis and treatment of adults with community-acquired pneumonia. an official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7).
20. Escher R, Breakey N, Lämmle B. Severe COVID-19 infection associated with endothelial activation. Thromb Res. 2020;190:62. doi:10.1016/j.thromres.2020.04.014
21. Levi M, van der Poll T. Inflammation and coagulation. Crit Care Med. 2010;38(2 Suppl):S26–34. doi:10.1097/CCM.0b013e3181c98d21
22. Abou-Ismail MY, Diamond A, Kapoor S, Arafah Y, Nayak L. The hypercoagulable state in COVID-19: incidence, pathophysiology, and management. Thromb Res. 2020;194:101–115. doi:10.1016/j.thromres.2020.06.029
23. Ward SE, Curley GF, Lavin M; Irish COVID-19 Vasculopathy Study (ICVS) Investigators. Von Willebrand factor propeptide in severe coronavirus disease 2019 (COVID-19): evidence of acute and sustained endothelial cell activation. Br J Haematol. 2020;16. PMID: 33326604. doi:10.1111/bjh.17273
24. Elsoukkary S, Mostyka S, Dillard A. Autopsy findings in 32 patients with COVID-19: a single-institution experience. Pathobiology. 2021;88(1):56–68. doi:10.1159/000511325
25. Gao Y, Li T, Han M, et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol. 2020;92(7):791–796. doi:10.1002/jmv.25770
26. Zhang L, Yan X, Fan Q, et al. D-dimer levels on admission to predict in-hospital mortality in patients with COVID-19. J Thromb Haemost. 2020;18(6):1324–1329. doi:10.1111/jth.14859
27. Stief TW, Ijagha O, Weiste B, Herzum I, Renz H, Max M. Analysis of hemostasis alterations in sepsis. Blood Coagul Fibrinolysis. 2007;18(2):179–186. doi:10.1097/MBC.0b013e328040bf9a
28. Scarlatescu E, Lance MD. Lance Crimean-Congo haemorrhagic fever: test early with ROTEM? Lancet Infect Dis. 2019;19(8):796–797. doi:10.1016/S1473-3099(19)30298-1
29. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585
30. Henry BM. COVID-19, ECMO, and lymphopenia: a word of caution. Lancet Respir Med. 2020;8(4):e24. doi:10.1016/S2213-2600(20)30119-3
31. Shang J, Wan Y, Luo C, et al. Cell entry mechanisms of SARS-CoV-2. Proc Natl Acad Sci U S A. 2020;117(21):11727–11734. doi:10.1073/pnas.2003138117
32. Brojakowska A, Narula J, Shimony R, Bander J. Clinical implications of SARS-CoV-2 interaction with renin angiotensin system: JACC review topic of the week. J Am Coll Cardiol. 2020;75(24):3085–3095. doi:10.1016/j.jacc.2020.04.028
33. Matarese A, Gambardella J, Sardu C, Santulli G. miR-98 regulates TMPRSS2 expression in human endothelial cells: key implications for COVID-19. Biomedicines. 2020;8(11):462. doi:10.3390/biomedicines8110462
34. Glowacka I, Bertram S, Muller MA, et al. Evidence that TMPRSS2 activates the severe acute respiratory syndrome coronavirus spike protein for membrane fusion and reduces viral control by the humoral immune response. J Virol. 2011;85(9):4122–4134. doi:10.1128/JVI.02232-10
35. D’Onofrio N, Scisciola L, Sardu C, et al. Glycated ACE2 receptor in diabetes: open door for SARS-COV-2 entry in cardiomyocyte. Cardiovasc Diabetol. 2021;20(1):99. PMID: 33962629; PMCID: PMC8104461. doi:10.1186/s12933-021-01286-7
36. Sardu C, Gargiulo G, Esposito G, et al. Impact of diabetes mellitus on clinical outcomes in patients affected by Covid-19. Cardiovasc Diabetol. 2020;19(1):76. doi:10.1186/s12933-020-01047-y
37. Sardu C, Maggi P, Messina V, et al. Could anti-hypertensive drug therapy affect the clinical prognosis of hypertensive patients with COVID-19 infection? Data from centers of southern Italy. J Am Heart Assoc. 2020;9(17):e016948. Epub 2020 Jul 7. PMID: 32633594; PMCID: PMC7660768. doi:10.1161/JAHA.120.016948
38. Sardu C, Marfella R, Maggi P, et al. Implications of AB0 blood group in hypertensive patients with covid-19. BMC Cardiovasc Disord. 2020;20(1):373. doi:10.1186/s12872-020-01658-z
39. López Reboiro ML, Suárez Fuentetaja R, Gutiérrez López R, et al. Role of lupus anticoagulant and von Willebrand factor in chronic reactive endotheliitis in COVID-19. J Infect. 2021;82(6):e27–e28. Epub 2021 Mar 15. PMID: 33737115; PMCID: PMC7959681. doi:10.1016/j.jinf.2021.03.006
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
