Back to Journals » Vascular Health and Risk Management » Volume 19
The Indirect Impact of COVID-19 Pandemic on Lower Extremity Amputations – An Australian Study
Authors Anthony L, Gillies M, Iyer V, Goh D
Received 17 June 2023
Accepted for publication 13 October 2023
Published 11 December 2023 Volume 2023:19 Pages 797—803
DOI https://doi.org/10.2147/VHRM.S426434
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Lakmali Anthony,1 Madeline Gillies,2 Vikram Iyer,1 David Goh1,3
1Department of Vascular Surgery, Northern Health, Epping, Victoria, Australia; 2Department of Surgery, Goulburn Valley Health, Shepparton, Victoria, Australia; 3Department of Vascular Surgery, Royal Melbourne Hospital, Parkville, Victoria, Australia
Correspondence: Lakmali Anthony, Email [email protected]
Background: The COVID-19 pandemic has had indirect and deleterious effects on patient health due to interruptions to routine provision of healthcare. This is particularly true for patients with chronic conditions like peripheral vascular disease (PVD). This study aims to evaluate the impact of the pandemic on patients with PVD in Australia by analysing rates of amputation, indications for amputation and urgency of surgery in the pre-pandemic and pandemic periods.
Methods: The Australian Vascular Audit was used to capture lower extremity amputation data in Victoria, Australia, in the 22 months before and after the start of the pandemic.
Results: The number of total amputations increased from 1770 pre-pandemic to 1850 during the pandemic, a 4.3% increase. This was largely driven by a statistically significant, 19% increase in major amputations. The number of minor amputations remained relatively similar in the two time periods. Amputations due to tissue loss secondary to arterial insufficiency increased from 474 to 526, an 11% increase, potentially indicating disruptions to revascularisation procedures contributing to the rise in amputations. Elective and emergency surgeries fell by 14% and 18%, respectively, while semi-urgent amputations increased by 32%.
Conclusion: This study found an increase in the number of amputations overall and a significant increase in major amputations during the pandemic compared to pre-pandemic times. Tissue loss secondary to arterial insufficiency was an increasingly common indication for amputation that was observed in the pandemic group, indicating that disruption to revascularisation likely contributed to this increase in amputations. These findings can inform and direct future vascular surgery service delivery to prepare for the post-pandemic recovery. Additionally, this study further confirms that patients with chronic diseases are often disproportionately disadvantaged when global crises affect routine provision of healthcare and calls for better systems to be developed that can be used in such crises in the future.
Keywords: amputation, COVID-19, pandemic, major amputation, minor amputation, peripheral vascular disease
A Letter to the Editor has been published for this article.
Introduction
Severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) was first identified in China in 2019 and subsequently spread across the world, leading to a global pandemic (COVID-19) in 2020. As the spread of the pandemic continued, claiming millions of lives worldwide, governments across the globe placed various infection control measures such as lockdowns, closures of schools, universities, and workplaces and restrictions on travel in an effort to slow the spread of the virus.1 Healthcare systems quickly became overwhelmed with a large number of patients acutely unwell with COVID-19. Due to the increased demand for COVID-related care, several measures were put in place to redirect the medical workforce. As a result, elective surgeries were cancelled and many regular outpatient follow-up clinics were cancelled or delayed.
As the second year of the pandemic ended in 2022, with lifting of lockdowns and easing of restrictions on schools, workplaces, and travel, many indirect effects of the pandemic on patient health have surfaced. The COVID 19 pandemic has had an impact on management of all diseases, especially the chronic ones, due to barriers caused by self-isolation, lockdowns, delays in follow-up and delays in elective surgery.2 Patients with peripheral vascular disease (PVD) requiring limb salvage procedures are among those affected by this disruption.
Studies from around the world have found an increase in lower limb amputation rates during the pandemic, with some countries reporting a 3-fold increase in minor amputations.3 Similar increases in amputation rates have been reported in India, Poland, China, Indonesia, Bangladesh, USA, and Argentina.4–10 Some studies have also found a major drop in lower limb revascularisation procedures.11,12 However, not all studies have found the same trend, with a few reporting no differences in amputation rates and two studies reporting a reduction in amputation rates during the pandemic.12–17 The studies that reported a reduction in amputation procedures, however, reflect a shorter follow-up time of 3–4 months into the pandemic that only included the initial lockdown period of the pandemic and therefore fail to capture the intermediate to long-term effects of delayed procedures or follow-ups.12,14
The state of Victoria had some of the strictest restrictions in Australia during the pandemic. Melbourne, the capital city of Victoria, has had one of the longest cumulative lockdowns in the world since the start of the pandemic, at 263 days.18 This large amount of time spent in lockdown combined with delays in routine follow-up and cancellations of elective surgery likely had deleterious effects on patients with chronic diseases including peripheral vascular disease. To the best of our knowledge, no studies have evaluated the indirect effects of the pandemic on patients with peripheral vascular disease in Australia yet. In this study, we hypothesise that Australia follows a similar trend to the rest of the world with considerable increases in the rates of lower limb amputations. If this was found to be the case, then PVD will require significant resource allocation to overcome this shortfall in the wake of the post-pandemic era. This study can inform and direct future vascular surgery service delivery and help prepare for the post pandemic recovery.
Materials and Methods
The Australasian Vascular Audit (AVA) was used to capture de-identified data on all lower limb amputation procedures between May 2018 and December 2021 in the state of Victoria.19 The AVA is a national audit mandated for all members of the Australian and New Zealand Society for Vascular Surgery (ANZSVS) who perform vascular procedures. It captures quality assurance and outcomes data. The procedures captured were divided into two groups based on when they were performed. Amputations conducted in the 22 months before the pandemic, between May 2018 and February 2020, were classified as the pre-pandemic group and those conducted in the 22 months since the start of the pandemic, between March 2020 and December 2021, were classified as the pandemic group. Amputations performed due to trauma were excluded. Amputations due to infection, ulceration (arterial and non-arterial), acute ischaemia, and rest pain (pain experienced at rest in the feet due to arterial insufficiency indicating chronic limb threatening ischaemia) were included. Information on demographics (age and sex), level of amputation, indication for surgery and category (emergency, semi-urgent, elective) were collected. Major amputations include above knee amputations (AKA) and below knee amputations (BKA). Minor amputations include toe and forefoot amputations.
Statistical analysis
Statistical analysis was performed with IBM SPSS Statistics version 29.0 (IBM Corp: Armonk, NY, USA). Descriptive data were presented as mean ± standard deviation (SD) for continuous variables and value and percentage for categorical variables. Continuous variables were compared using Student’s t-test while categorical variables were compared using chi-square test. A p-value < 0.05 was considered significant.
Results
The mean age and distribution of genders were similar in pre-pandemic and pandemic groups with no significant differences between them (Table 1). A majority of patients in both groups had co-morbidities of diabetes and ischaemic heart disease (IHD). Notably, during the pandemic, there was a statistically significant shift in the demographic profile of patients undergoing amputations with a statistically significant reduction in patients with IHD and a statistically significant increase in those with diabetes (Table 1)
 |
Table 1 Patient Demographics |
The total number of amputations increased from 1768 in the pre-pandemic group to 1847 in the pandemic group, a 4.3% increase (Table 2). Major amputations increased from 392 to 468, a 19.4% increase and this was statistically significant (Table 2). In the subgroup analysis of major amputations, above knee amputations (AKAs) increased from 120 in the pre-pandemic group to 149 in the pandemic group, a 24.2% increase. Similarly, below knee amputations (BKAs) increased from 272 to 318, a 16.9% increase. In minor amputations, forefoot amputations decreased from 236 to 228, a 3.4% decrease and toe amputations were roughly similar in the two groups – 1140 in the pre-pandemic group compared to 1152 in the pandemic group, a 1% increase. None of the observed changes in these subgroups of amputations were statistically significant (Table 2).
 |
Table 2 Number of Amputations in Pre-Pandemic and Pandemic Groups |
In terms of indication for surgery, the number of amputations done due to infection, non-arterial ulcer, acute ischaemia, and rest pain were similar in pre-pandemic and pandemic groups (Table 3). However, amputations due to tissue loss (ulcer/gangrene) secondary to arterial insufficiency increased from 474 in the pre-pandemic group to 526 in the pandemic group, an 11% increase during the pandemic. None of the observed differences in indication for surgery were statistically significant (Table 3).
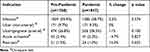 |
Table 3 Indications for Amputation in Pre-Pandemic and Pandemic Groups |
Given the significant increase in major amputations, subgroup analyses for indications for major and minor amputations were carried out (Table 4). A statistically significant increase was observed in major amputations carried out due to arterial ulcers or gangrene and for minor amputations carried out due to infection (Table 4).
 |
Table 4 Indications for Major and Minor Amputations in Pre-Pandemic and Pandemic Groups |
In terms of type of surgery, elective procedures reduced from 543 to 465 (p = 0.014), a 14.4% decrease, and emergency surgeries decreased from 464 to 379 (p = 0.003) during the pandemic, an 18.3% decrease (Table 5). Semi-urgent procedures increased significantly from 761 to 1003 (p = <0.001), a 32% increase. These observed differences between the groups in terms of type of surgery were all statistically significant (Table 5).
 |
Table 5 Surgery Type in Pre-Pandemic and Pandemic Groups |
Discussion
The COVID-19 pandemic has had a profound negative impact on patient health due to the interruptions to standard provision of healthcare.2–11 Many patients with chronic diseases were unable to have their regular follow-up visits due to infection control methods such as lockdowns while many others avoided or delayed presenting to hospital with acute deteriorations of their chronic conditions due to fear of contracting COVID-19.20,21 Patients with PVD were further affected by cancellation of their scheduled, elective surgeries which likely delayed vital revascularisation and limb salvage procedures.22
In the current study, we investigated the indirect impact of the COVID-19 pandemic on patients with PVD by evaluating the lower limb amputation rates during the pandemic period and comparing it to pre-pandemic times. We found an increase in amputations during the pandemic in Victoria, Australia; however, this increase was less severe than what has been reported in other countries.2–11 In Italy, a 3-fold increase in amputations has been reported.3 Similarly, a >50% increase in major amputations has been reported in India.6 Given that Victoria had some of the harshest restrictions during the pandemic, it is worth investigating strategies that vascular surgery units in Victoria used to somewhat reduce the effects of the pandemic on their services. No studies exist that explore such strategies yet.
This study also found that the observed increase in total amputations was primarily driven by a significant increase in major amputations (BKAs and AKAs) which strongly suggests delayed presentations with more severe disease and delays in revascularisation procedures as potential contributors to this increase in amputations. Consistent with this hypothesis, a few studies have found that patients were presenting with more severe critical limb threatening ischaemia during the pandemic compared to pre-pandemic times and other studies have reported a reduction in revascularisation procedures during the pandemic.22–25
In terms of indication for amputation, a lot more amputations were carried out due to tissue loss (ulcer/gangrene) secondary to arterial insufficiency during the pandemic, and this finding was statistically significant for major amputations, further indicating that delayed revascularisation procedures likely played a significant role in this rise in major amputations in the pandemic period. A few studies in the literature have evaluated the effect of the pandemic on lower limb revascularisation procedures, and they have produced mixed results. Some studies report a reduction in revascularisation procedures during the pandemic, while one study from Australia report an increase in endovascular revascularisation procedures during the pandemic.24,26,27 As such, further investigation into this topic is warranted.
This study also found a significant increase in amputations done as “semi-urgent” surgeries and significant reductions in “elective” and “emergency” surgeries. The reduction in elective surgery is unsurprising given the cancellations of these procedures during the pandemic. The reduction in emergency surgeries, however, is an unexpected result. It can, however, most likely be explained by the impact of the pandemic on health services overall. A vascular surgery procedure gets classified as an “emergency” if a patient is taken to theatre on the day of their presentation to hospital or as “semi-urgent” if the surgery can be delayed to the following day. It is possible that the reduction in emergency surgery during the pandemic reflects the delays that occurred as a consequence of the pandemic. Factors such as staff shortages due to self-isolation requirements and infection control measures may have contributed to these delays.2,11 Additionally, the increased demand for COVID-related healthcare services may have also contributed to the reduction in the ability to carry out emergency surgery as many hospitals were not able to operate at full theatre capacity during the pandemic.2,11
One limitation of the current study is the use of AVA data. Whilst it is a robust, national database, it relies on surgeons consistently and accurately logging their procedures to the database. While the vast majority of surgeons would comply, the possibility of missed entries cannot be excluded. Therefore, our data may not reflect all the procedures carried out in the state of Victoria during the study period. One strength of this study, however, is the large sample size. With a large sample size, a few missed entries are unlikely to affect the observed results in any meaningful way. Another strength of our study is its duration. A study time period of twenty two months before and after the start of the pandemic is an adequate length of time to observe any adverse effects of delayed revascularisation surgeries and delayed follow-up on a population level. Another limitation of our study is the inability to distinguish between amputations secondary to deterioration of diabetes and those secondary to PVD alone. It is worth noting that many of the studies we have referenced for comparison predominantly focus on amputations associated with diabetic foot complications. Given the fact that a significant majority of our study population had a diagnosis of diabetes and that coexistence of diabetes and PVD is generally common, we deemed it appropriate to compare our study findings with those primarily focused on diabetic foot-related amputations. Nevertheless, it is crucial to recognise and acknowledge this notable limitation of our study.
In terms of future research, this study highlights the need for evaluating the rates of lower limb revascularisation procedures during the pandemic and their correlation to amputation rates. It also highlights the need for an exploration of methods various vascular surgery units have used during the pandemic to minimise disruption to their service delivery and the effectiveness of those strategies so that they can be adopted when such crises arise in the future.
Conclusions
This study found an increase in the number of amputations overall and a significant increase in major amputations during the pandemic compared to pre-pandemic times. Tissue loss secondary to arterial insufficiency was an increasingly common indication for amputation that was observed in the pandemic group, indicating that disruption to revascularisation surgery likely contributed to this increase in amputations. This information can be used for making triage decisions and allocation of resources in vascular surgery services in the post-pandemic period. Additionally, this study provides evidence that patients with chronic diseases such as peripheral vascular disease are often disproportionately disadvantaged when global crises affect routine provision of healthcare. This calls for better systems to be developed that can be used in such crisis situations in the future and calls for an evaluation of the effectiveness of the strategies used by various countries during this pandemic.
Institutional Review Board Statement
This was a retrospective, population-based study with de-identified data obtained from the Australasian Vascular Audit (AVA). AVA is a national audit mandated for all members of ANZSVS, the governing body for vascular surgeons in Australia and New Zealand. There was no personally identifiable material within the data set obtained from AVA. As per National Health and Medical Research Council’s (NHMRC) guidelines, Royal Australasian College of Surgeons (RACS) Human Research Ethics Committee (HREC) has deemed AVA data as low risk and has informed that no ethics committee approval is required. As such, individual patient consent or individual hospital ethical approval was not required.
Data Sharing Statement
The dataset is available on demand from the corresponding author.
Acknowledgments
The authors would like to thank the Australasian Vascular Audit for providing the de-identified data set that was used to carry out this study.
Funding
This research received no external funding.
Disclosure
The authors declare no conflict of interest.
References
1. World Health Organization. COVID-19 Dashboard. Geneva: World Health Organization; 2020. Available from: https://covid19.who.int/.
2. Miranda C, Zanette G, Da Ros R. Diabetic foot disease during the COVID-19 pandemic: lessons learned for our future. Arch Med Sci Atheroscler Dis. 2022;7:e94–e103. doi:10.5114/amsad/151047
3. Caruso P, Longo M, Signoriello S, et al. Diabetic foot problems during the COVID-19 pandemic in a tertiary care center: the emergency among the emergencies. Diabetes Care. 2020;43(10):e123–e124. doi:10.2337/dc20-1347
4. Kleibert M, Mrozikiewicz-Rakowska B, Bąk PM, Bałut D, Zieliński J, Czupryniak L. Breakdown of diabetic foot ulcer care during the first year of the pandemic in Poland: a retrospective national cohort study. Int J Environ Res Public Health. 2022;19(7):3827. doi:10.3390/ijerph19073827
5. Liu C, You J, Zhu W, et al. The COVID-19 outbreak negatively affects the delivery of care for patients with diabetic foot ulcers. Diabetes Care. 2020;43(10):e125–e126. doi:10.2337/dc20-1581
6. Viswanathan V, Nachimuthu S. Major lower-limb amputation during the COVID Pandemic in South India. Int J Low Extrem Wounds. 2021;15347346211020985. doi:10.1177/1534734621102098
7. Yunir E, Tarigan TJE, Iswati E, et al. Characteristics of diabetic foot ulcer patients pre- and during COVID-19 Pandemic: lessons learnt from a national referral hospital in Indonesia. J Prim Care Community Health. 2022;13:21501319221089767. doi:10.1177/21501319221089767
8. Ahmed J, Saha H, Rouf MA, Wadud MA, Islam S, Russel SM. Prevalence of major amputation in COVID-19 era compared to non-COVID-19 Era- A descriptive retrospective single centre study. Fortune J Health Sci. 2022;5:29–36.
9. Casciato DJ, Yancovitz S, Thompson J, et al. Diabetes-related major and minor amputation risk increased during the COVID-19 pandemic. J Am Podiatr Med Assoc. 2020;20–224. doi:10.7547/20-224
10. Carro GV, Carlucci EM, Torterola I, Breppe P, Ticona Ortiz MÁ, Palomino Pallarez JE. Diabetic foot and COVID-19. Medical consultation and severity of lesions compared to 2019. Pie diabético y COVID-19. Número de consultas y gravedad de las lesiones comparadas con 2019. Medicina. 2020;80(6):30–34.
11. Mariet AS, Benzenine E, Bouillet B, Vergès B, Quantin C, Petit JM. Impact of the COVID-19 Epidemic on hospitalization for diabetic foot ulcers during lockdown: a French nationwide population-based study. Diabet Med. 2021;38(7):e14577. doi:10.1111/dme.14577
12. Valabhji J, Barron E, Vamos EP, et al. Temporal trends in lower-limb major and minor amputation and revascularization procedures in people with diabetes in England during the COVID-19 pandemic. Diabetes Care. 2021;44(6):
13. de Mestral C, Gomez D, Wilton AS, et al. A population-based analysis of diabetes-related care measures, foot complications, and amputation during the COVID-19 pandemic in Ontario, Canada. JAMA network open. 2022;5(1):e2142354. doi:10.1001/jamanetworkopen.2021.42354
14. Schmidt BM, Munson ME, Rothenberg GM, Holmes CM, Pop-Busui R. Strategies to reduce severe diabetic foot infections and complications during epidemics (STRIDE). J Diabetes Complications. 2020;34(11):107691. doi:10.1016/j.jdiacomp.2020.107691
15. Rubin G, Feldman G, Dimri I, Shapiro A, Rozen N. Effects of the COVID-19 pandemic on the outcome and mortality of patients with diabetic foot ulcer. Int Wound J. 2023;20(1):63–68. doi:10.1111/iwj.13837
16. Ergişi Y, Özdemir E, Altun O, Tıkman M, Korkmazer S, Yalçın MN. Indirect impact of the COVID-19 pandemic on diabetes-related lower extremity amputations: a regional study. Jt Dis Relat Surg. 2022;33(1):203–207. doi:10.52312/jdrs.2022.564
17. Mayoral E, Ravé R, Rodriguez de Vera P, et al. Temporal trends in hospitalizations due to diabetes complications during COVID-19 pandemic in Andalusia, Spain. BMJ Open Diabetes Res Care. 2022;10(2):e002623. doi:10.1136/bmjdrc-2021-002623
18. Lockdown stats Melbourne. Available from: https://lockdownstats.melbourne/.
19. Beiles CB, Bourke B, Thomson I. Results from the Australasian vascular surgical audit: the inaugural year. ANZ J Surg. 2012;82(3):105–111. doi:10.1111/j.1445-2197.2011.05987.x
20. Bansal S, Roy M, Chatterjee T, Roy AK. Deaths due to delayed presentation to the hospital from fear of contracting COVID-19 during lockdown period: a tertiary care center experience. J Community Hosp Intern Med Perspect. 2021;11(3):299–301. doi:10.1080/20009666.2021.1918440
21. Gluckman TJ, Wilson MA, Chiu ST, et al. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiology. 2020;5(12):1419–1424. doi:10.1001/jamacardio.2020.3629
22. Erman A, Ramsay LC, Sander B, et al. Impact of COVID-19 on scheduled lower extremity revascularization for chronic limb-threatening ischemia. Br J Surg. 2021;109(1):e5–e7. doi:10.1093/bjs/znab404
23. Guarinello GG, D’Amico RC, Miranda ANM, Novack J, Coral FE. Impact of COVID-19 on the surgical profile of vascular surgery patients at a tertiary hospital in Curitiba Brazil. J Vascul Brasil. 2022;21:e20220027. doi:10.1590/1677-5449.202200271
24. Keller K, Schmitt VH, Hobohm LMA, Brochhausen C, Münzel T, Espinola-Klein C. Temporal trends in patients with peripheral artery disease influenced by COVID-19 pandemic. J Clin Med. 2022;11(6433):6433. doi:10.3390/jcm11216433
25. Trunfio R, Deslarzes-Dubuis C, Buso G, et al. The effects of COVID-19 pandemic on patients with lower extremity peripheral arterial disease: a near miss disaster. Ann Vasc Surg. 2021;77:71–78. doi:10.1016/j.avsg.2021.07.006
26. Grima MJ, Dimech AP, Pisani D, Chircop F, Warrington E, Cassar K. COVID-19 pandemic lockdown: uncovering the hard truth on lower limb ischaemic outcomes? A single centre observational study. Eur J Vasc Endovasc Surg. 2022;63(2):e32. doi:10.1016/j.ejvs.2021.12.011
27. Cai YT, Fisher G, Loa J. Changing patterns in Australian and New Zealand: vascular surgery during COVID-19. ANZ J Surg. 2021;91(11):2389–2396. doi:10.1111/ans.17200
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
