Back to Journals » Clinical Ophthalmology » Volume 17
The Impact of the COVID-19 Pandemic on Wait-Times for Ophthalmic Surgery in Ontario, Canada: A Population-Based Study
Authors Balas M , Vasiliu D, Austria G, Felfeli T
Received 21 February 2023
Accepted for publication 2 May 2023
Published 26 June 2023 Volume 2023:17 Pages 1823—1831
DOI https://doi.org/10.2147/OPTH.S409479
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Michael Balas,1 Diana Vasiliu,2 Gener Austria,2 Tina Felfeli3– 5
1Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada; 2Health System Intelligence Team, Health System Performance & Support Portfolio, Ontario Health, Toronto, ON, Canada; 3Department of Ophthalmology and Vision Sciences, University of Toronto, Toronto, ON, Canada; 4Toronto Health Economics and Technology Assessment (THETA) Collaborative, University Health Network, Toronto, ON, Canada; 5The Institute of Health Policy, Management and Evaluation (IHPME), University of Toronto, Toronto, ON, Canada
Correspondence: Tina Felfeli, Toronto Western Hospital, 399 Bathurst Street, 6-East Room 432, Toronto, ON, M5T 2S8, Canada, Tel +1 647 678 1634, Fax +1 416 340 3459, Email [email protected]
Objective: To investigate the effects of the COVID-19 pandemic on case volumes and wait-times for ophthalmic surgery in Ontario, Canada.
Design: Population-based retrospective cohort study.
Participants: Patients undergoing ophthalmic surgery in Ontario, Canada, from 2010 to 2021, collected from the Ontario Health Wait Times Information System (WTIS) database.
Methods: The WTIS contains non-emergent surgical case volume and wait-time data for six ophthalmic subspecialty surgery types, three priority levels (low, medium, high) and 14 different regions in Ontario. Case volume and wait-times were compared between the COVID-19 pandemic (2020– 2021) and the preceding time period (2010– 2019) across all stratifications.
Results: There was a significant decrease in case volumes and significant increase in wait-times across geographic regions, priority levels, and subspecialty surgeries from the pre-pandemic to pandemic period. Moreover, COVID-19 exacerbated pre-existing wait-time disparities between sexes, with females waiting 4.1 days longer than males overall to receive surgery in 2010– 2019 compared to waiting 8.8 days longer in 2020– 2021 (117% increase).
Conclusion: These findings highlight the impact of the COVID-19 pandemic on ophthalmic surgical wait times in Ontario. Cataract, strabismus and oculoplastic surgeries, the Waterloo Wellington, Central, and South East regions of Ontario, and those with female sex had the greatest relative increases in wait-times during the pandemic.
Keywords: ophthalmology, surgery, wait time
Introduction
The COVID-19 pandemic has had a significant impact on the delivery of healthcare around the world,1 including accessibility to ophthalmic surgery.2–6 In Ontario, Canada, wait-times for ophthalmic surgery have been an ongoing concern, with increasing delays in surgery being linked to reduced patient satisfaction and poor outcomes.7–10 While various strategies have been employed to try to reduce wait-times and improve access to care, the COVID-19 pandemic has presented additional challenges and may have had a substantial impact on wait-times for ophthalmic surgery. Moreover, it exposed and exacerbated health disparities that resulted in poorer outcomes for certain patient populations.11
This study aims to investigate the effects of the COVID-19 pandemic on wait-times and case volumes for patients receiving ophthalmic surgery in Ontario, Canada. Understanding the impact of the pandemic on ophthalmic surgery in Ontario will provide valuable insights into the challenges faced by the healthcare system and may inform future strategies to improve access to care.
Methods
This retrospective cohort study used data from the Ontario Health Wait Times Information System (WTIS) database from 2010 to 2021.12–14 It followed the Reporting of Studies Conducted using Observational Routinely-collected Data (RECORD) guidelines and was approved by the University of Toronto Research Ethics Board (RIS protocol number: 41582).15
Data Source
This study used the WTIS database, which was implemented in 2008.14,16,17 The WTIS collects and stores data on wait times for non-emergency surgeries performed under the Ontario Health Insurance Plan (OHIP) publicly funded health services for eligible residents.18 For triaging and resource allocation purposes when using the WTIS, surgeons assign each case a priority level according to WTIS guidelines, ranging from level 1 emergent cases (not included in the WTIS database) to high priority (level 2, severe symptoms, which are likely worsening), medium priority (level 3, some pain or other symptoms, which do not dramatically impact quality of life), and low priority (level 4, the patient’s condition may be worsening and medical management may be failing to help).19
According to the WTIS, wait time is defined as the number of days between the decision to operate and the time of surgery. Wait-list queues with only 1–5 cases per month are coded as “low volume” by the WTIS and were excluded from this study. The WTIS database captures annual wait-time data for the following types of non-emergency ophthalmic surgery: cataract, cornea, glaucoma, oculoplastic, vitreoretinal, and adult strabismus surgery. This data is further divided into 14 geographical regions called Local Health Integration Networks (LHINs), which comprise the subdivision of Ontario healthcare delivery. In April 2021, they were grouped into five regions, however, the results presented in this study use the previously defined 14 LHINs. The original LHINs covered the following areas: Erie St. Clair, South West, Waterloo Wellington, Hamilton Niagara Haldimand Brant, Central West, Mississauga Halton, Toronto Central, Central, Central East, South East, Champlain, North Simcoe Muskoka, North East, and North West.
Study Objectives
We aimed to compare patient volumes and wait-times for different types of ophthalmic surgeries stratified by region and priority between pre-pandemic (2010–2019) and pandemic (2020–2021) time periods. We also investigated whether the COVID-19 pandemic affected patient demographics across different strata, with particular focus on sex-based differences in wait-times.
Statistical Analysis
Cohort characteristics were stratified by ophthalmic surgery type, priority level, geographic region, and sex, and were reported descriptively. We compared the differences in surgical volume and wait-time between the pandemic (2020–2021) and an average of all previous years (2010–2019). An independent-samples t-test was used to analyze the aggregate data for continuous outcomes (mean with SD and sample number volumes) for the two groups. All analyses were conducted using R version 3.5.0 (R Foundation for Statistical Computing, Vienna, Austria). To reduce the probability of Type I errors, a conservative value of P<0.001 was chosen a priori to denote statistical significance.
Results
In Ontario, Canada, from 2010 to 2021, there was an average 1.49 adults per 100,000 scheduled for non-emergency ophthalmic surgery per year. The mean wait time for all surgery types and priority levels over this period was 82 days (SD 85). The mean age of these patients was 71 years (SD 11), and 44% of all patients were male. Both age and proportion of males remained consistent at 71 years and 44%, respectively, across all years from 2010 to 2021.
Surgical Volume
There was a significant reduction in surgical volume in 2020 and 2021 due to COVID-19. From 2010 to 2019, there was an average annual 153,388 adults (SD 5094) that underwent ophthalmic surgery compared to an average annual 129,090 (SD 22,395) in 2020–2021. However, reductions in case volumes were proportionally similar between both sexes, with males receiving 67,167 annual surgeries in 2010–2019 compared to 57,495 in 2020–2021 (14% reduction), and females receiving 86,221 annual surgeries in 2010–2019 compared to 71,595 in 2020–2021 (17% reduction). When stratifying by priority level, there was a significantly higher proportion of patients undergoing high and medium priority surgery during the pandemic, while a higher proportion of low priority surgeries were performed pre-pandemic (p<0.001, Table 1).
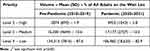 |
Table 1 Overall Volume of Ophthalmic Surgery in Ontario Stratified by Priority Level |
Surgical Wait-Time
Despite the reduction in case volumes, the pandemic also increased wait-times, with an average 74.6 days (SD 76.2) in 2010–2019 compared to 116.4 days (SD 127.4) days in 2020–2021 across all surgical surgery types, geographic regions, and priority levels (56.0% increase, p<0.001). The subspecialties that had the highest wait-time delays included cataract (p<0.001), strabismus (p<0.001), and oculoplastic surgeries (p<0.001). Those that were less affected included vitreoretinal (p<0.001), glaucoma (p<0.001), and corneal surgeries (p=0.78). The overall wait-times for each surgery in 2010–2019 compared to 2020–2021 are summarized in Figure 1.
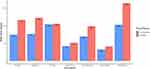 |
Figure 1 Bar graph illustrating the difference in wait-times (days) between the pre-pandemic (2010–2019) and pandemic (2020–2021) period, stratified by the type of subspecialty surgery. |
Furthermore, the wait-time disparity between males and females significantly grew in 2020–2021 during the pandemic (Figure 2). Overall, sex-based differences in wait-times more than doubled (117% increase), with females waiting 4.1 days longer in 2010–2019 to waiting 8.8 days longer in 2020–2021 (p<0.001). Glaucoma surgery (1150% increase, p<0.001), oculoplastic surgery (230% increase p<0.001), and strabismus surgery (140% increase, p<0.001) had the greatest relative increases in wait-time disparities during COVID-19. Cataract (103% increase, p<0.001) and vitreoretinal (60% increase, p<0.001) surgeries also experienced significant increases in wait-time disparities during the pandemic. Only corneal surgery (26% decrease, p<0.001) had a reduced disparity in wait-times between sexes in 2020–2021, although females still waited 3.9 days longer on average.
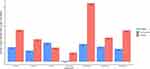 |
Figure 2 Bar graph illustrating the number of days females wait longer than males between the pre-pandemic (2010–2019) and pandemic (2020–2021) period, stratified by the type of subspecialty surgery. |
Geographic Differences
The COVID-19 pandemic disproportionally affected some regions more than others when comparing wait-times for ophthalmic surgery (Figure 3A, Table 2). For example, Waterloo Wellington (173% increase, p<0.001), Central (136% increase, p<0.001), and the South East (75.5% increase, p<0.001) regions had the greatest increases in wait-times from 2010–2019 to 2020–2021. Whereas regions including North Simcoe Muskoka (25.0% increase, p<0.001) and the Central West (24.5% increase, p<0.001) demonstrated the smallest increase. All 14 Ontario LHINs each had significantly longer wait-times during the pandemic (p<0.001). Furthermore, all of the LHINs except for North Simcoe Muskoka had significantly decreased volume during the pandemic (p<0.001, Figure 3B, Table 3).
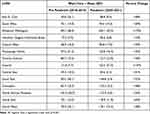 |
Table 2 Overall Wait-Time of Ophthalmic Surgery in Ontario Stratified by Local Health Integration Network (LHIN) |
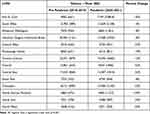 |
Table 3 Overall Volume of Ophthalmic Surgery in Ontario Stratified by Local Health Integration Network (LHIN) |
With regard to sex-based wait-time disparities across geographic regions, 12/14 regions in Ontario had an increasing wait-time gap between sexes in 2020–2021 (Figure 3C, Table 4). North Simcoe Muskoka had the smallest increase at 3%, with females waiting 6.7 days longer in 2010–2019 compared to waiting 6.9 days longer in 2020–2021 (p=0.22). Regions that were most affected by the pandemic were the Waterloo Wellington (1245% increase, p<0.001), Central (515% increase, p<0.001), Central West (425% increase, p<0.001), Mississauga Halton (254% increase, p<0.001), and Toronto Central (125% increase, p<0.001) LHINs. When stratifying the region with the greatest disparity, Waterloo Wellington, by priority level, females waited 5.3 (883% increase from 0.6 days to 5.9 days, p<0.001) and 34.8 (1289% increase from 2.7 days to 37.5 days, p<0.001) days longer for low and medium priority levels, respectively, in pandemic compared to pre-pandemic time periods. However, for high priority level cases, females waited 4.6 days longer than males in 2010–2019 and 2.4 days less than males in 2020–2021 (91.7% decrease, p=0.003). Only two regions in Ontario had a reduced wait-time gap between sexes in 2020–2021: the South West (21% decrease, p<0.001) and North West (6% decrease, p=0.003).
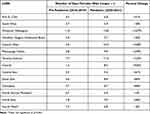 |
Table 4 Overall Number of Days Females Wait Longer Than Males for Ophthalmic Surgery in Ontario Stratified by Local Health Integration Network (LHIN) |
Discussion
This population-based retrospective cohort study highlights the substantial effects of the COVID-19 pandemic on case volumes and wait-times for ophthalmic surgery in Ontario, Canada. There were fewer case volumes overall and a significant increase in wait-times for all subspecialty surgeries, geographic regions, and priority levels. We also found that the COVID-19 pandemic severely exacerbated pre-existing sex-based differences in surgical wait-times, where males have significantly shorter waiting times compared to females. In certain cases, the difference between male and female waiting times increased ten-fold from pre-pandemic to pandemic periods.
We noted a significant reduction in surgical volume during the pandemic (approximately 25,000 less patients per year) that remained proportionally similar between males and females. However, the volume of high priority cases nearly doubled in 2020–2021, with slightly more medium priority cases performed as well. This is likely due to the prioritization of more urgent cases during the pandemic as healthcare systems were faced with limited resources. In contrast, there was a higher volume of low-priority surgery prior to the pandemic, given the availability of more resources and the ability to prioritize a wider range of cases. There was also considerable variability in case volume reductions from pre-pandemic to pandemic between LHINs, with some regions (eg Central West) losing a third of all cases, while others (eg South West) exhibited almost no change. Only one region, North Simcoe Muskoka, had increased volume during the pandemic, with approximately 30% more cases compared to 2010–2019.
Even with a lower volume of surgical cases, there were significantly longer wait-times for ophthalmic surgery during the pandemic. The reasons for this prolonged wait-time are likely multifaceted, but could include the need for additional safety measures, the diversion of resources to address the pandemic, and the challenges faced by healthcare systems in managing the increased demand for care. Specifically, cataract, strabismus, and oculoplastic surgeries had the largest increase in wait-times, whereas corneal surgery wait-times were largely unaffected by the pandemic. With exception to corneal surgery, the degree to which wait-times increased corresponded to the proportion of high-priority cases. For instance, glaucoma (11.4%) and vitreoretinal (18.6%) surgeries had the highest proportion of high-priority cases, while having some of the smallest increases in wait-times during the pandemic. Likewise, cataract (1.1%), strabismus (1.0%), and oculoplastic (2.8%) surgeries had the lowest proportions of high-priority cases. This relationship did not apply to corneal surgery, which also had a low proportion of high-priority cases (3.5%). Instead, corneal wait-times may have remained unchanged between 2010–2019 and 2020–2021 due to the limited supply of eye bank corneal tissue, which could have a stronger rate-limiting mechanism than the effects of the pandemic.20 Overall, these findings highlight the need for more resources and strategies to mitigate the impact of future public health crises on ophthalmic surgery wait-times and avoid extensive surgical backlogs.2
In addition to increasing overall wait-times for ophthalmic surgery, the COVID-19 pandemic also amplified the difference in wait-times between males and females. In our dataset, this disparity more than doubled overall during the pandemic and worsened over all priority levels of ophthalmic surgery. Moreover, this disparity significantly grew for all but one of the ophthalmic subspecialties (corneal surgery) and 12 out of the 14 LHINs in Ontario. Females in Toronto Central, the region with the highest population density, procedural volume, and ratio of ophthalmologists per 100,000 in Ontario (8.87), experienced one of the greatest disparities and went from waiting 7.7 days longer than males in 2010–2019 to waiting 17.3 days longer in 2020–2021.21 A complex interplay of socio-political and cultural factors, including taking on the role of a caregiver and prioritizing the needs of other family members over personal appointments, may contribute to females experiencing longer wait-times, according to previous studies.22,23 Further research is necessary to determine the underlying contributing factors to longer wait times for females.
Limitations and Future Directions
The WTIS data used in this study did not include patient or hospital-level covariates, such as institutional pandemic safety measures or COVID-19 status, and thus these variables could not be included in the analysis. This includes a lack of data on the specific ophthalmic procedures performed within each subspecialty in addition to the frequency and types of ophthalmic disease presentations. WTIS also does not include information on the time from primary care referral to diagnostic work-up. Additionally, the WTIS database only recorded patient sex, not gender or other self-reported identities, and so the findings may not accurately represent the wait-time differences experienced by nonbinary individuals or self-identifying men and women.24 There may also be some variability in how different surgeons assign patient priority-levels in the database that could affect results. Future research should aim to fully characterize sex-based differences in wait-times by analyzing the full spectrum of care, from symptom onset to specialist consultation to surgery and even post-operative follow-up. This would be essential in understanding the potential role of patient and provider characteristics in the observed trends.
Conclusion
This retrospective cohort study explored the difference in eye surgery case volumes and wait-times between the COVID-19 pandemic (2020–2021) and the time period immediately preceding it (2010–2019). Our findings provide valuable insights into the challenges faced by the healthcare system during the pandemic and highlight the need for ensuring equitable access to care for all patients, regardless of sex or other characteristics.
Acknowledgments
The authors would like to thank Reeza Menalo and Claudia Zanchetta for their support.
Funding
Tina Felfeli has received grants from the Vanier Canada Graduate Scholarship, Canada Graduate Scholarship-Masters, the Vision Science Research Program, Fighting Blindness Canada, and Postgraduate Medical Education Research Awards as part of postsecondary research funding. The funding organizations had no role in the design or conduct of this research.
Disclosure
No conflicting relationship exists for any author.
References
1. Kaye AD, Okeagu CN, Pham AD, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: international perspectives. Best Pract Res Clin Anaesthesiol. 2021;35(3):293–306.
2. Felfeli T, Ximenes R, Naimark DM, et al. The ophthalmic surgical backlog associated with the COVID-19 pandemic: a population-based and microsimulation modelling study. Can Med Assoc J. 2021;9(4):E1063–E1072.
3. Wiseman SM, Crump RT, Sutherland JM. Surgical wait list management in Canada during a pandemic: many challenges ahead. Can J Surg. 2020;63(3):E226. doi:10.1503/cjs.006620
4. Eshghi SRT, Cheema M, Damji KF. Effect of the COVID-19 pandemic on elective cataract surgery wait times. Can J Ophthalmol. 2022. doi:10.1016/j.jcjo.2022.09.001
5. Saggaf MM, Anastakis DJ. The impact of COVID-19 on the surgical wait times for plastic and reconstructive surgery in Ontario. Plast Surg. 2021;22925503211064381. doi:10.1177/2292550321106438
6. Wong JSH, Cheung KMC. Impact of COVID-19 on orthopaedic and trauma service: an epidemiological study. J Bone Joint Surg Am. 2020;102(14):e80. doi:10.2106/JBJS.20.00775
7. Felfeli T, Austria G, Menalo R, et al. Temporal trends in ophthalmic surgical demand in a universal healthcare system: an Ontario population-based study of over two decades. BMJ. 2022;7:e000937.
8. Felfeli T, Balas M, Austria G, Menalo R, Vasiliu D, Zanchetta C. Regional trends in ophthalmic surgical wait times in Ontario, Canada. Can J Ophthalmol. 2023;58(3):e104–e106.
9. McMullen M, Netland PA. Wait time as a driver of overall patient satisfaction in an ophthalmology clinic. Clin Ophthalmol. 2013;7:1655. doi:10.2147/OPTH.S49382
10. Hodge W, Horsley T, Albiani D, et al. The consequences of waiting for cataract surgery: a systematic review. CMAJ. 2007;176(9):1285–1290. doi:10.1503/cmaj.060962
11. Gray DM, Anyane-Yeboa A, Balzora S, Issaka RB, May FP. COVID-19 and the other pandemic: populations made vulnerable by systemic inequity. Nat Rev Gastroenterol Hepatol. 2020;17(9):520–522. doi:10.1038/s41575-020-0330-8
12. Ontario ministry of health and long-term care. Ontario Wait Times; 2008. Available from: https://www.health.gov.on.ca/en/pro/programs/waittimes/surgery/data.aspx.
13. Ontario Health. Ontario wait times strategy; 2022. Available from: https://www.ontariohealth.ca.
14. Kirby M. Review of Ontario’s Wait Time Information System. Ministry of Health and Long-Term Care; 2007.
15. Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi:10.1371/journal.pmed.1001885
16. MacLeod H, Hudson A, Kramer S, Martin M. The times they are a-changing: what worked and what we learned in deploying Ontario’s wait time information system. Healthc Q. 2009;12(Sp):8–15. doi:10.12927/hcq.2009.20744
17. Closson T. Ontario’s wait time information system: learning from success. Healthc Q. 2009;12(sp):1. doi:10.12927/hcq.2009.20743
18. Ministry of Health. Apply for OHIP and get a health card; 2017. Available from: https://www.ontario.ca/page/apply-ohip-and-get-health-card.
19. Health Quality Ontario. Measuring wait times for other surgeries and procedures; 2022. Available from: https://www.hqontario.ca/System-Performance/Measuring-System-Performance/Measuring-Wait-Times-for-Other-Surgeries-and-Procedures.
20. Humphreys C, Maru K, Yeung SN, Rocha G, Chan CC. Canadian demand and access to corneal transplantation: a provincial comparison. Cell Tissue Bank. 2022;23(4):685–693. doi:10.1007/s10561-021-09968-y
21. Lin T, Xu M, Hooper PL. Adequacy of the ophthalmology workforce under Ontario’s local health integration networks. Can J Ophthalmol. 2016;51(3):142–146. doi:10.1016/j.jcjo.2015.10.012
22. Razmjou H, Lincoln S, Macritchie I, Richards RR, Medeiros D, Elmaraghy A. Sex and gender disparity in pathology, disability, referral pattern, and wait time for surgery in workers with shoulder injury. BMC Musculoskelet Disord. 2016;17(1):1–9. doi:10.1186/s12891-016-1257-7
23. Armstrong P, Armstrong H. Thinking It Through: Women, Work and Caring in the New Millennium. Healthy Balance Research Program Halifax; 2001.
24. Nahmias J, Zakrison TL, Haut ER, et al. Call to action on the categorization of sex, gender, race, and ethnicity in surgical research. J Am Coll Surg. 2021;233(2):316–319. doi:10.1016/j.jamcollsurg.2021.04.025
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

