Back to Journals » Substance Abuse and Rehabilitation » Volume 14
The Impact of Injectable Opioid Agonist Treatment (iOAT) on Involvement in Criminalized Activities: A Secondary Analysis from a Clinical Trial in Vancouver, BC
Authors Dobischok S, Guh D, Marchand K, MacDonald S, Lock K, Harrison S, Lajeunesse J, Schechter MT, Oviedo-Joekes E
Received 26 September 2023
Accepted for publication 7 November 2023
Published 15 November 2023 Volume 2023:14 Pages 147—156
DOI https://doi.org/10.2147/SAR.S438451
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rajendra D. Badgaiyan
Sophia Dobischok,1,2 Daphne Guh,2 Kirsten Marchand,2 Scott MacDonald,3 Kurt Lock,2,4 Scott Harrison,3 Julie Lajeunesse,3 Martin T Schechter,2,5 Eugenia Oviedo-Joekes2,5
1Department of Education and Counselling Psychology, McGill University, Montreal, QC, Canada; 2Centre for Advancing Health Outcomes, Providence Health Care, Vancouver, BC, Canada; 3Providence Health Care, Providence Crosstown Clinic, Vancouver, BC, Canada; 4BC Centre for Disease Control, Provincial Health Services Authority, Vancouver, BC, Canada; 5School of Population and Public Health, University of British Columbia, Vancouver, BC, Canada
Correspondence: Eugenia Oviedo-Joekes, Centre for Advancing Health Outcomes, St. Paul’s Hospital, 575-1081 Burrard St, Vancouver, BC, V6Z 1Y6, Canada, Tel +1 604-682-2344 Ext. 62973, Fax +1-604-806-8210, Email [email protected]
Purpose: A significant portion of the economic consequences of untreated Opioid Use Disorder (OUD) relate to individuals’ involvement in the criminal justice system. The present study uncovers if treatment with iOAT is related to the number of criminal charges amongst participants, what type of crime participants were involved in, and the frequency with which participants were victims of crime. This study contributes to the body of research on the effectiveness of iOAT reducing criminal involvement.
Patients and Methods: This is a secondary analysis of police record data obtained from the Vancouver Police Department over a three-year period during the Study to Assess Longer-term Opioid Medication Effectiveness clinical trial. The data was obtained from participants (N = 192) enrolled in the trial through a release of information form.
Results: During the three-year period, most charges (45.6%) were property offences, and 25.5% of participants were victims of crime. Participants with no treatment prior to randomization into the SALOME trial were 2.61 (95% CI = 1.64– 4.14) more likely to have been charged with a crime than during the iOAT state.
Conclusion: IOAT can reduce individuals’ involvement with the criminal justice system and is thus a crucial part of the continuum of care. Addiction should be conceptualized as a healthcare rather than criminal issue.
Keywords: heroin assisted treatment, diacetylmorphine, hydromorphone, crime, charges, police
Introduction
Unregulated opioid use has historically been associated with criminal involvement due to a complex and nuanced intersection of psychological, social, environmental, and political factors (eg, poverty, mental illness, histories of trauma, the War on Drugs).1–3 Beyond the acute personal costs that individuals may experience from contact with the criminal justice system, economic analyses indicate that lost property and policing, prosecuting, and incarcerating people who use drugs incurs immense societal costs.4,5 The global economic burden of enforcing drug-related criminalized activities is more than $100 billion annually.6 Opioid use disorder (OUD) treatment’s ability to reduce clients’ interactions with the criminal justice system is thus an outcome of interest to benefit both the individual and society.
Treatment with oral opioid agonist treatment (OAT) such as buprenorphine-naloxone methadone can reduce clients’ involvement in criminal activity,7,8 with the largest reductions in clients retained in care longer-term.9 While oral OAT effectively retains many clients into care,10 it does not meet the needs of a crucial subset of clients.11 Left by the healthcare system to rely on the contaminated illicit supply, these individuals are at heightened overdose risk12 and have more interactions with the criminal justice system than those retained in oral OAT.13 As such, the continuum of care for OUD continues to expand to include innovative and evidence-based options for clients who find oral options ineffective or undesirable.14
Injectable OAT (iOAT) is a form of prescribed safer supply15 in which clients receive pharmaceutical grade heroin (diacetylmorphine, or DAM) or an analogue (such as hydromorphone, or HDM; more injectable medications are continually becoming available). Over two decades of international clinical trials overwhelmingly conclude that iOAT is safe and effective to treat severe OUD.16–20 While pharmaceutical heroin has a higher direct cost than oral OAT medications, iOAT is more cost-effective overall when considering the indirect social costs of untreated or ineffectively treated OUD.21–23 For example, prescription heroin trials in Switzerland suggest that heroin assisted treatment substantially reduces criminal involvement across a broad range of criminal activities (eg, property theft, selling illegal substances, use/possession of illegal substances), even in the post-treatment period.24 Furthermore, a recent systematic review of ten randomized control trials concluded that iOAT reduces clients’ engagement in illegal activities.25
Cost-effectiveness studies reveal that most of the savings from iOAT stem from clients’ reduced involvement in criminal activity during treatment.23 Methods to report and record criminal involvement vary in the iOAT evidence-base. Besides self-reported data and court records, police records provide a system-level perspective on iOAT’s impact beyond clients’ engagement with clinical services. The current paper is a secondary analysis of police record data obtained from the Vancouver Police Department (VPD) over a three-year period during the Study to Assess Longer-term Opioid Medication (SALOME) clinical trial.17 We aimed to determine how treatment with injectable DAM or HDM relates to participants’ criminal justice system involvement. Specifically, we examined if iOAT is related to the number of criminal charges amongst participants, the type of crime participants were involved in, and the frequency with which participants were victims of crime. This analysis contributes to the extant evidence on the effectiveness of iOAT reducing criminal involvement.
Materials and Methods
Design, Setting, and Participants
The current study is a secondary analysis from a Phase III, double-blind non-inferiority trial that compared DAM with HDM to treat individuals not benefitting from other OUD treatment (SALOME).17 Participants were recruited between December 2011 and December 2013 from the greater Vancouver area. The trial occurred at a single site (Crosstown Clinic) in downtown Vancouver. Inclusion criteria for the trial were individuals aged 19 and over with a history of severe, chronic OUD with injection drugs who lived in Vancouver, Canada.17 Exclusion criteria were any mental or physical conditions that were contraindicated for DAM or HDM. Recruitment procedures have been described in depth previously.26
Of the 202 total participants involved in the trial, 102 were randomly assigned to DAM and 100 to HDM for a period of six months. The participants’ baseline characteristics have been previously published.27 In brief, most participants had long histories of using injection heroin (greater than 15 years), an average of approximately 5 previous attempts at oral methadone treatment, past involvement in the criminal justice system, and current involvement in illegal activities.
During the consent process, participants were required to sign a release of information (ROI) form that permitted researchers to obtain their criminal records from the Vancouver Police Department (VPD) and other local police jurisdictions from one year prior to their specific date of randomization to two years after. As consent was an ongoing process, participants could drop out of the trial and rescind their ROI without any negative repercussions. We obtained ROIs to access police data from 192 of the 202 participants (five had passed away, and five were lost to follow up). Specifically, the ROI permitted the research team to obtain the following information over the three-year study period:
- records of criminal convictions for which the participant has not been pardoned (may not include criminal convictions in other jurisdictions that have not yet been entered in the CPIC database);
- records of outstanding charges against the participant which are pending disposition;
- records of all charges against the participant, regardless of disposition; and
- all police records, information and details of allegations of criminal conduct or of statutory offences committed or that the participant is suspected of having committed.
While these official police record data encompass the comprehensive range of criminalized activities, it is unable to encompass criminal activities that were not identified by police.
Data and Analysis
The primary record category of interest is official criminal charges. These records indicate that criminal charges were recommended against the accused individual by the criminal justice system. Charged is a distinct category from suspected chargeable, which is defined as records in which grounds exist to recommend a charge against the individual, but the police/complainant/victim do not pursue them. Charged is also distinct from recommended charge, which are records where the police recommend charges but the Crown dropped them.
Each participant was followed from one year prior to their specific randomization date, to two years after or death (whichever date was earlier). The exposure of interest is treatment state during the observed period. We defined the sequence of treatment episodes for each participant first for iOAT, and for other treatments (including oral methadone and other forms of OAT) where treatment discontinuation for a given treatment was defined as ≥7 consecutive days without the treatment. Then, to have a clear understanding of the role of iOAT in treatment discontinuation, two periods of no-treatment were defined. The first period was before participants were randomized to the SALOME trial, as at the time the only available treatment option was oral methadone and possibly buprenorphine, but this medication was not recommended to the study population, and consequently there was very little use of it. The second no-treatment state was specific to after randomization into the SALOME trial, meaning any participant that stopped treatment after iOAT was available to them, as well as other forms of OAT (eg, oral hydromorphone). As such, our exposure of interest has four mutually exclusive treatment states: i) iOAT; ii) other treatment (oral OAT or oral methadone but no iOAT); iii) no-treatment (ie, no form of OAT and no oral methadone) prior to randomization into the SALOME trial and iv) no-treatment after randomization into the SALOME trial.
The charges will be presented by offence type, which refers to the categories of crime and their associated specific charges as determined by the local police department. Descriptive analysis for the total sample will be presented with mean (SD) for continuous variables and proportions for categorical variables on participants’ sociodemographics, self-reported history of engagement with the criminal system, illegal activities, drug use, and health status. Bivariate analysis comparing those with and without criminal charges will be performed. Finally, the impact of iOAT will be measured using the rate of criminal charges per 100 treatment days, comparing iOAT with the other three treatment states: 1) no-treatment prior randomization into the SALOME trial, 2) no-treatment after randomization into the SALOME trial and 3) other treatment. Generalized linear mixed-effects models with negative binomial distribution for count data were used to estimate the unadjusted and adjusted rate ratios where age, gender, race (indigenous ancestry vs other), usual housing status (unstable including living on the street vs stable) in the past 3 years, the Opiate Treatment Index (OTI) health scale and experience of serious depression in life (yes vs no) were controlled for. All analyses were performed in SAS 9.4 and R (Version 4.1.2).
Results
Participant Characteristics
The sociodemographic information for the 192 participants the study was able to obtain ROIs for is presented in Table 1. On average, participants were 44.5 years old and almost three quarters identified as male (70.3%). Fifty-eight participants, or nearly a third of the sample, identified as having Indigenous ancestry, and over half of participants (55.2%) reported chronic medical problems. At baseline, the self-reported average number of months previously incarcerated was 37.3, and the average number of days of illegal activities in the prior month was 13.9 days. Bivariate analyses indicated that participants with and without charges were similar. However, those who were younger, had longer histories of incarceration, more days of illegal activities in the prior month, spent more money on drugs in the prior month, and for whom prior treatments did not work were more likely to have charges during the study period.
 |
Table 1 Sample Characteristics |
Over the three-year period from one year prior to each participants’ randomization date to two years after, there were a total of 1,337 records (ie, any event from any category in Table 2) affiliated with 160 of the 192 participants whose police data the researchers could access. Of the 1,337 overall events, 259 records belonged to the “charge” category. These charge events were linked to 81 out of the 192 participants, meaning that 81 participants were charged a total of 259 times in the three-year study period. Of note, 25.5% (49) of participants had records in which their role was victim of a crime. The records received from the police encompassed eleven different categories which are described in Table 2.
 |
Table 2 Number of Records by Role Definition. Records Obtained from the Vancouver Police Department (VPD) from One Year Prior to Participants’ Specific Date of Randomization to Two Years After |
Offence Type
A breakdown of the charges by offence type is presented in Figure 1. The offences fell into four categories: Property, Substance, Violent, and Other. The largest offence category was Property, with 118 of the overall 259 charges in this category. The most frequent property offence was “Theft—Shoplifting under $5000”, which comprised 76 of the 118 property offence records. Followed by the Property category, the second largest category was Other (62 charges). The two most frequent charges in this category were “Breach of Probation—Adult” and “Breach/Bail Violations” which combined for 39 of the 62 charges in this category. Third was the Substance category, with 45 of the 259 total charges. This category was composed of substance trafficking (29 charges) and substance possession (16 charges). Finally, the smallest offence category was violent offences, comprising only 33 of the 259 total charges. In this category, the most frequent offence was “Assault—With Weapon or Causing Bodily Harm” (13 charges).
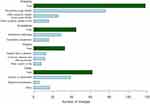 |
Figure 1 Total number of charges by offence type for the 259 overall charges divided into four categories (green) with associated grouped offence subcategories (blue). |
Number of Charges
The most charges occurred in the No Treatment – Prior SALOME trial state (n = 132) followed by the No Treatment – Post SALOME trial state (n = 56), the iOAT state (n = 48) and finally the Other Treatment state (n = 17). The criminal charges were compared across the four treatment states, with the iOAT state being the reference state (Table 3). The number of charges, considering the unadjusted rate per person days, were statistically significantly lower in the iOAT state compared to no-treatment state prior to randomization and after randomization into the SALOME trial state; the unadjusted rate ratio was 2.73 (95% CI: 1.96–3.80) and 2.08 (95% CI: 1.41–3.05), respectively. When compared to the other treatment state, the rate of charges was also lower in the iOAT state, but the difference was not statistically significant (rate ratio 1.27, 95% CI: 0.73–2.21).
 |
Table 3 Pair Comparisons of Incidence of Official Criminal Charges During the Period Receiving Injectable Opioid Agonist Treatment Over Three Years |
Adjusted by age, gender, Indigeneity (self-reported Aboriginal ancestry), housing, physical and mental health, the model ratified the difference, where participants with no treatment prior to randomization into the SALOME trial were 2.61 (95% CI = 1.64–4.14) times more likely to have been charged with a crime than during the iOAT state.
Discussion
The current secondary analysis of the SALOME clinical trial used police data over a three-year period (one year prior to randomization to two years after) to investigate 1) the types of charges that individuals with severe opioid use acquired over the three-year period; 2) the impact that iOAT had on the number of charges participants had during the three-year period; and 3) the frequency with which participants were victims of charges themselves. This study was conducted in a context where political and policing systems often construe addiction as a criminal issue, when research indicates it should be understood and addressed as a matter of healthcare.28 To reach the best outcome for both people who use drugs and society, it is essential that the focus shift from finding ways to penalize people who use drugs to finding ways to engage them into care that they find effective, accessible, and agreeable to meet their self-identified goals. For people with OUD, prior research has consistently shown that engagement in addiction care such as oral OAT can reduce clients’ involvement in illegal activities, and that these reductions yield substantial societal savings from costs that were previously funneled into the criminal justice system.7,13,29
The comparison by treatment states showed that participants had significantly higher charges during the no-treatment state prior randomization into the SALOME trial compared to the iOAT state. Stated differently, iOAT clients were 2.6 times less likely to be charged with a crime compared to the period of no-treatment prior to SALOME. These results align with previous analyses that suggest that OAT broadly, and iOAT specifically, are associated with reduced involvement in illegal activities.9,25 These results add to the growing scientific consensus that care, rather than criminalization, is the avenue that leads to alleviated burden on the criminal justice system, reduced social costs, and the best outcomes for people who use drugs.
The analyses of the types of offences committed by our sample during the entire three-year period indicated that most charges against participants were low-value property theft (coded by the police department as “Theft – Shoplifting under $5000”). While there is great societal stigma about violence among people who use heroin, and a link does exist between opioid use and risk of violence,30 our findings are consistent with previous research that indicates the primary offence committed by people who use injection drugs is indeed low-value theft and not violent crime.31 In fact, a Swedish study found that people incarcerated for violent crime had the lowest prevalence of injection drug use compared to any other crime in a population of incarcerated people with substance use problems.32 While the current study did not explore specific reasons why criminal involvement decreased, it is conceivable based on the analyses of types of offences and the available literature that once participants no longer had to procure funds to purchase street substances, theft was no longer a necessity to meet their needs.33,34
The police data showed that 25.5% of trial participants were victims of a violent crime during the three-year period. While there may be an impulse to characterize people who use opioids as perpetrators of crime due to their persistent criminalization by the political and criminal justice systems, our results suggest that the participants in the iOAT trial were the victims of crime at a disproportionate rate. These findings highlight that clients who access iOAT should not be characterized as a risky population, but rather one at-risk of victimization. People who use drugs have long been at risk of heightened victimization,35 and the findings from this trial indicate the risk remains a concern. For example, an analysis of over 82000 individuals admitted into substance use treatment in Denmark found a strong association between substance use disorders and violent victimization.36 Cost analyses have also shown that the increased victimization of people who use drugs contributes to an increased social cost by forcing more people into contact with the criminal justice system at great expense.37 Thus, the role of iOAT in preventing victimization, potentially through trauma-informed implementation, requires further examination.
The role of police is not adequate to meet nuanced, integrated healthcare needs of people with severe OUD.38 To support engagement in care programs that are best equipped to meet individuals where they are at in their addiction, a paradigm shift to healthcare over criminalization is essential. This shift is particularly important to support populations who experience heightened inequity from the criminal justice system (ie, minority racial groups).39 This secondary analysis suggests that iOAT is one effective option that can help reduce people with severe OUD’s contact with the criminal justice system. By continuing to expand the scope of available medications and formulations and prioritizing accessible treatment delivery,40 the addiction care system can better engage and retain clients into care, prevent encounters between clients and the criminal justice system, and reduce the economic burden of addiction. Future research might investigate the intersection of iOAT and criminal activity in the years since SALOME, particularly given British Columbia’s recent decriminalization of small amounts of substances as of January 31st, 2023.41 Qualitative research could also investigate participants’ perspectives on how iOAT influences their participation in criminalized activities.
This study has key limitations to acknowledge. Firstly, the data analyzed was collected several years prior to the current analysis and may not be consistent with current iOAT client patterns of criminalized activities. Particularly, drug enforcement laws in British Columbia have shifted since that time.41 Despite the time delay, the data validity remains strong as it was obtained directly from official police records, and iOAT delivery is almost identical to how it was administered during the SALOME trial.42 There are very few opportunities internationally to investigate data in this setting and population, and to our knowledge, there has been no other research group that was able to hold similar data or is currently collecting data in this form. Thus, the data remain important although we were not able to put it forward until this time. Secondly, the only alternative option to iOAT at the time of the trial was oral OAT. At the same time, this limitation should be understood in the context that many countries only have oral OAT as their singular OUD treatment option. Thirdly, most participants were male and non-Indigenous and thus may not be representative of the broader population. The sample was recruited for a clinical trial based on the inclusion criteria, so any extrapolation can be understood in that context. Finally, this secondary analysis does not permit us to infer causality (ie, that iOAT itself lead to the reduction in charges). To account for other factors that might have impacted the results, we adjusted our model by age, gender, ethnicity, housing, and mental/physical health.
Conclusion
IOAT is an effective component of the opioid use continuum of care that can reduce clients’ involvement in the criminal justice system. Prioritizing healthcare over criminalization can support caring for the unique needs of people with severe OUD in a way that benefits both the individual and society.
Acknowledgments
The authors respectfully acknowledge the unceded and traditional territory of the Coast Salish Peoples, including the traditional territories of xʷməθkwəýəm (Musqueam), Sḵwxw ú7mesh (Squamish), and Səlí̓ lwətaɬ (Tsleil-Waututh) Nations, upon which this research took place. We graciously thank all the SALOME participants, and the research and clinical teams.
Funding
SALOME was funded by an operating grant from the Canadian Institutes of Health Research [MCT-103817] in partnership with Providence Health Care and financing from the InnerChange Foundation, Providence Health Care Research Institute, St. Paul’s Hospital Foundation, and Vancouver Coastal Health. Additional financial support was provided by the Michael Smith Foundation for Health Research Career Award and the Canada Institutes of Health Research New Investigator Award (EOJ) and the Canada Research Chairs Program (MTS). The funding sources were not involved in any aspect of the study or manuscript. The SALOME trial received ethical approval from the University of British Columbia and Providence Healthcare research ethics boards, and all participants provided informed written consent.
Disclosure
Dr Martin Schechter reports grants from Canadian Institutes for Health Research during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Hall W, Bellb J, Carless J. Crime and drug use among applicants for methadone maintenance. Drug Alcohol Depend. 1989;31(1993):123–129. doi:10.1016/0376-8716(93)90064-W
2. Teesson M, Marel C, Darke S, et al. Long-term mortality, remission, criminality and psychiatric comorbidity of heroin dependence: 11-year findings from the Australian treatment outcome study. Addiction. 2015;110(6):986–993. doi:10.1111/add.12860
3. Pierce M, Hayhurst K, Bird SM, et al. Insights into the link between drug use and criminality: lifetime offending of criminally-active opiate users. Drug Alcohol Depend. 2017;179:309–316. doi:10.1016/j.drugalcdep.2017.07.024
4. Degenhardt L, Whiteford H, Hall WD. The Global Burden of Disease projects: what have we learned about illicit drug use and dependence and their contribution to the global burden of disease? Drug Alcohol Rev. 2014;33(1):4–12. doi:10.1111/dar.12088
5. Jiang R, Lee I, Lee TA, Pickard AS. The societal cost of heroin use disorder in the United States. PLoS One. 2017;12(5). doi:10.1371/journal.pone.0177323
6. Rolles S, Murkin G, Powell M, Kushlick D, Slater J. The alternative world drug report: counting the costs of the war on drugs; 2012.
7. Lind B, Chen S, Weatherburn D, Mattick R. The effectiveness of methadone maintenance treatment in controlling crime: an Australian aggregate-level analysis. Brit J Criminol. 2005;45(2):201–211. doi:10.1093/bjc/azh085
8. Sun HM, Li XY, Chow EPF, et al. Methadone maintenance treatment programme reduces criminal activity and improves social well-being of drug users in China: a systematic review and meta-analysis. BMJ Open. 2015;5(1):e005997. doi:10.1136/bmjopen-2014-005997
9. Bukten A, Skurtveit S, Gossop M, et al. Engagement with opioid maintenance treatment and reductions in crime: a longitudinal national cohort study. Addiction. 2012;107(2):393–399. doi:10.1111/j.1360-0443.2011.03637.x
10. Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;2014(2). doi:10.1002/14651858.CD002207.pub4
11. Piske M, Zhou H, Min JE, et al. The cascade of care for opioid use disorder: a retrospective study in British Columbia, Canada. Addiction. 2020;115(8):1482–1493. doi:10.1111/add.14947
12. Pearce LA, Min JE, Piske M, et al. Opioid agonist treatment and risk of mortality during opioid overdose public health emergency: population based retrospective cohort study. BMJ. 2020:368. doi:10.1136/bmj.m772
13. Russolillo A, Moniruzzaman A, McCandless LC, Patterson M, Somers JM. Associations between methadone maintenance treatment and crime: a 17-year longitudinal cohort study of Canadian provincial offenders. Addiction. 2018;113(4):656–667. doi:10.1111/add.14059
14. Vogel M, Meyer M, Westenberg JN, et al. Safety and feasibility of intranasal heroin-assisted treatment: 4-week preliminary findings from a Swiss multicentre observational study. Harm Reduct J. 2023;20(1). doi:10.1186/s12954-023-00731-y
15. National Safer Supply Community of Practice. Emerging evidence brief on prescribed safer supply and client experiences; 2023.
16. Oviedo-Joekes E, Brissette S, Marsh DC, et al. Diacetylmorphine versus methadone for the treatment of opioid addiction. N Engl J Med. 2009;361(8):777–786. doi:10.1056/nejmoa0810635
17. Oviedo-Joekes E, Guh D, Brissette S, et al. Hydromorphone compared with diacetylmorphine for long-term opioid dependence. JAMA Psychiatry. 2016;73(5):447. doi:10.1001/jamapsychiatry.2016.0109
18. Strang J, Groshkova T, Uchtenhagen A, et al. Heroin on trial: systematic review and meta-analysis of randomised trials of diamorphine-prescribing as treatment for refractory heroin addiction. Br J Psychiatry. 2015;207(1):5–14. doi:10.1192/bjp.bp.114.149195
19. Haasen C, Verthein U, Degkwitz P, Berger J, Krausz M, Naber D. Heroin-assisted treatment for opioid dependence: randomised controlled trial. Br J Psychiatry. 2007;191(JULY):55–62. doi:10.1192/bjp.bp.106.026112
20. Demaret I, Quertemont E, Litran G, et al. Efficacy of heroin-assisted treatment in Belgium: a randomised controlled trial. Eur Addict Res. 2015;21(4):179–187. doi:10.1159/000369337
21. Nosyk B, Guh DP, Bansback NJ, et al. Cost-effectiveness of diacetylmorphine versus methadone for chronic opioid dependence refractory to treatment. CMAJ. 2012;184(6):E317–E328. doi:10.1503/cmaj.110669
22. Byford S, Barrett B, Metrebian N, et al. Cost-effectiveness of injectable opioid treatment v. oral methadone for chronic heroin addiction. Br J Psychiatry. 2013;203(5):341–349. doi:10.1192/bjp.bp.112.111583
23. Bansback N, Guh D, Oviedo-Joekes E, et al. Cost-effectiveness of hydromorphone for severe opioid use disorder: findings from the SALOME randomized clinical trial. Addiction. 2018;113(7):1264–1273. doi:10.1111/add.14171
24. Ribeaud D. Long-term impacts of the Swiss Heroin prescription trials on crime of treated heroin users. J Drug Issues. 2004;34(1):163–194. doi:10.1177/002204260403400108
25. Smart R, Reuter P. Does heroin-assisted treatment reduce crime? A review of randomized-controlled trials. Addiction. 2022;117(3):518–531. doi:10.1111/add.15601
26. Oviedo-Joekes E, Marchand K, Lock K, Macdonald S, Guh D, Schechter MT The SALOME study: recruitment experiences in a clinical trial offering injectable diacetylmorphine and hydromorphone for opioid dependency; 2015. Available from: http://www.substanceabusepolicy.com/content/10/1/3.
27. Oviedo-Joekes E, Marchand K, Macdonald DS, Krausz M History of treatment access and drug use among participants in a trial testing injectable opioids under supervision for long-term heroin injectors; 2015. Available from: https://www.researchgate.net/publication/278406606.
28. Volkow ND, Poznyak V, Saxena S, Gerra G. Drug use disorders: impact of a public health rather than a criminal justice approach. World J Psychiatry. 2017;16(2):213–214. doi:10.1002/wps.20428
29. Havnes I, Bukten A, Gossop M, Waal H, Stangeland P, Clausen T. Reductions in convictions for violent crime during opioid maintenance treatment: a longitudinal national cohort study. Drug Alcohol Depend. 2012;124(3):307–310. doi:10.1016/j.drugalcdep.2012.02.005
30. Zhong S, Yu R, Fazel S. Drug use disorders and violence: associations with individual drug categories. Epidemiol Rev. 2020;42(1):103–116. doi:10.1093/epirev/mxaa006
31. Sanders B, Lankenau SE, Bloom JJ, Hathaz DS. A typology of drug-related offending among youth homeless injection drug users. J Drug Issues. 2009;39(4):777–802. doi:10.1177/002204260903900401
32. Håkansson A, Jesionowska V. Associations between substance use and type of crime in prisoners with substance use problems – a focus on violence and fatal violence. Subst Abuse Rehabil. 2018;9:1–9. doi:10.2147/sar.s143251
33. Sutherland R, Sindicich N, Barrett E, et al. Motivations, substance use and other correlates amongst property and violent offenders who regularly inject drugs. Addict Behav. 2015;45:207–213. doi:10.1016/j.addbeh.2015.01.034
34. Ellefsen R, Wüsthoff LEC, Arnevik EA. Patients’ satisfaction with heroin-assisted treatment: a qualitative study. Harm Reduct J. 2023;20(1):73. doi:10.1186/s12954-023-00808-8
35. McElrath K, Chitwood DD, Comerford M. Crime victimization among injection drug users. J Drug Issues. 1997;27(4):771–783. doi:10.1177/002204269702700406
36. Seid AK, Hesse M, Houborg E, Thylstrup B. Substance use and violent victimization: evidence from a cohort of >82,000 patients treated for alcohol and drug use disorder in Denmark. J Interpers Violence. 2022;37(13–14):NP12427–NP12452. doi:10.1177/0886260521997456
37. French MT, Mccollister KE, Alexandre PK, Chitwood DD, Mccoy CB. Revolving roles in drug-related crime: the cost of chronic drug users as victims and perpetrators. J Quant Criminol. 2004;20(3):217–241. doi:10.1023/B:JOQC.0000037732.00489.ad
38. Butler A, Zakimi N, Greer A. Total systems failure: police officers’ perspectives on the impacts of the justice, health, and social service systems on people who use drugs. Harm Reduct J. 2022;19(1). doi:10.1186/s12954-022-00629-1
39. Nicosia N, MacDonald JM, Arkes J. Disparities in criminal court referrals to drug treatment and prison for minority men. Am J Public Health. 2013;103(6):e77–e84. doi:10.2105/AJPH.2013.301222
40. Meyer M, Westenberg JN, Strasser J, et al. Nasal administration of diacetylmorphine improved the adherence in a patient receiving heroin-assisted treatment. Harm Reduct J. 2022;19(1). doi:10.1186/s12954-022-00644-2
41. British Columbia Government. Decriminalizing people who use drugs in B.C; 2023. Available from: https://www2.gov.bc.ca/gov/content/overdose/decriminalization#:~:text=Under%20this%20exemption%2C%20adults%20(18,Crack%20and%20powder%20cocaine.
42. Oviedo-Joekes E, Dobischok S, Carvajal J, et al. Clients’ experiences on North America’s first take-home injectable opioid agonist treatment (iOAT) program: a qualitative study. BMC Health Serv Res. 2023;23(1):553. doi:10.1186/s12913-023-09558-6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
