Back to Journals » Clinical Interventions in Aging » Volume 17
The Impact of Frailty on Perioperative Outcomes in Patients Receiving Short-Level Posterior Lumbar Interbody Fusion: A Stepwise Propensity Score Matching Analysis
Authors Cui P , Wang P, Wang J, Liu X , Kong C, Lu S
Received 13 June 2022
Accepted for publication 20 August 2022
Published 25 August 2022 Volume 2022:17 Pages 1297—1306
DOI https://doi.org/10.2147/CIA.S378327
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Peng Cui,1,2,* Peng Wang,1,2,* Jialin Wang,1,2 Xu Liu,1,2 Chao Kong,1,2 Shibao Lu1,2
1Department of Orthopedics, Xuanwu Hospital, Capital Medical University, Beijing, People’s Republic of China; 2National Clinical Research Center for Geriatric Diseases, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Chao Kong; Shibao Lu, Email [email protected]; [email protected]
Background: There are many studies on the impact of frailty on postoperative complications; however, there are few studies focusing on stepwise propensity score matching (PSM) to offset the influence of age.
Methods: We gathered data for patients undergoing short-level posterior lumbar interbody fusion from January to December 2021. According to the Fried frailty phenotype, we categorized patients into non-frail, pre-frail, and frail groups, then, stepwise PSM for age, sex, American Society of Anesthesiologists (ASA) and fusion levels were performed to keep comparable clinical data between groups. Univariate and multivariate logistic regressions were used to determine the impact of clinical demographics on postoperative complications.
Results: A total of 559 consecutive patients with complete medical records were enrolled (237 males and 322 females; mean age 72.55 ± 5.86 years). After PSM, we found that pre-frail patients were more vulnerable to develop urinary retention (p = 0.031) and surgical site infections (p = 0.021) than non-frail patients. Longer length of stay (LOS), delayed ambulation and removal of urinary catheter times were observed in pre-frail patients. However, there was a significant difference only in LOS between pre-frail and frail patients. Binary logistic regression revealed that C-reactive protein (CRP) and frail status were independently associated with postoperative complications between non-frail and pre-frail patients, while only CRP was independently correlated with complications between pre-frail and frail patients.
Conclusion: After PSM, we found higher rates of urinary retention and surgical site infections in pre-frail patients than in non-frail patients. CRP was independently related to postoperative complications, while frail status was only independently associated with postoperative complications between pre-frail and non-frail patients. Pre-frail/frail patients tended to have more severe stress responses than non-frail patients.
Keywords: frail, propensity score matching, lumbar, postoperative complications
Introduction
Kehlet proposed enhanced recovery after surgery (ERAS) in 19971. This modality is a multimodal, multidisciplinary management strategy,2,3 designed to reduce postoperative adverse events and accelerate recovery by decreasing stress responses, shortening the length of stay (LOS) and hospitalization costs.4,5 Established and maturely implemented in 20196, numerous patients benefited from ERAS in our department, although there was a reduction in LOS and lower complication rates, specific patients cannot be discharged as quickly as expected despite ERAS, demonstrating that some other preoperative evaluations should be emphasized.
Previous studies documented many factors associated with prolonged LOS, and postoperative complications have been discussed. According to a retrospective study of 217 patients, Strickland et al7 reported that elderly patients were more prone to develop postoperative urinary retention and had longer LOS. Kong et al8 demonstrated that the lower body mass index (<24.32kg/m2) was related to minor complications. In a retrospective study of 630 patients undergoing elective lumbar disc arthroplasty, Ansari et al9 found that longer operation length was correlated with prolonged LOS and patients with prolonged LOS were more vulnerable to venous thromboembolisms, pneumonia, surgical site infections, and reoperations.
Frailty is a syndrome characterized by decreased physiological reserve, daily activities and strength.10,11 Accurate risk stratification and prediction of postoperative complications over time are imperative in older patients undergoing lumbar fusion surgery.12 Many studies have reported convincing results inn recent years that frailty is a stronger predictor than age for postoperative morbidity.13,14 However, older adults are a heterogeneous group of patients and frailty is obviously related to age; therefore, when discussing the effect of frailty on postoperative outcomes, it is necessary to eliminate the effect of age on frail status. This study aimed to determine the effect of frailty on postoperative outcomes in patients undergoing short-level lumbar fusion surgery after eliminating the influence of age as a confounding factor according to propensity score matching.
Patients and Methods
Study Design
This was a retrospective, monocentric, and consecutive cohort study. We included all patients with complete demographic data who underwent short-level posterior lumbar interbody fusion between 1 January 2021 and 31 December 2021. As distinguished by Fried frailty phenotype and modified frailty index, Frailty was evaluated by trained nurses after admission to ward. And in this study, Fried frailty phenotype was utilized to describe frail status. Then, we grouped patients into 3 groups according to the frail status and stepwise PSM was performed to ensure groups with comparable clinical data. The institutional review board in Xuanwu Hospital Capital Medical University approved the study (No. 2018008), which followed the Declaration of Helsinki principles. Written informed consent was obtained from all participants.
Patient Selection
We retrospectively reviewed patients undergoing short-level posterior lumbar interbody fusion between 1 January 2021 and 31 December 2021. Inclusion criteria were as follows: 1) lumbar disk herniation, lumbar spinal stenosis, and lumbar spondylolisthesis according to radiographic examination and magnetic resonance imaging by two experienced surgeons; 2) no history of spinal surgery; 3) age greater than 65 years; and 4) short-level lumbar fusion surgery defined as the number of fusion levels no more than two. The exclusion criteria were as follows: 1) emergency surgery; 2) lack of clinical data; 3) combined surgery; and 4) other severe surgical contraindications. Finally, there were 559 patients with complete clinical data enrolled. The detailed flowchart is shown in Figure 1.
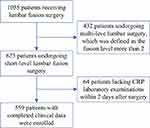 |
Figure 1 Patient selection flowchart. |
Data Collection
All information relating to patients was obtained from medical records. The collected preoperative clinical data included age, sex, body mass index (BMI), concomitant diseases (hypertension, diabetes, osteoporosis, gastrointestinal, heart diseases, and hyperlipidemia), operation time, estimated blood loss (EBL), fusion levels, 30-day readmission rates, postoperative intensive care units stays and American Society of Anesthesiologists (ASA) classification. As a routine postoperative laboratory examination item, c-reactive protein (CRP) was extracted according to the result of the first laboratory test within two days after surgery. LOS was defined as interval from the first day after operation to discharge. Besides, urinary catheter extraction time, and postoperative mobilization time (both defined as the interval from the first day after operation to the corresponding measures) were also extracted. Postoperative complications included nausea and vomiting, surgical site infection, cerebrospinal fluid leakage, urinary retention, urinary tract infection, deep venous thrombosis, and myocardial ischemia.
Fried Frailty Phenotype
The Fried frailty phenotype we used in this study was described by Fried et al,15 which was comprised of five variables including unintentional weight loss, self-reported exhaustion, low physical activity, slowness and weakness. The score assigns one point for these factors and the Fried frailty score was calculated for each subject by adding each variable. According to the Fried criteria, we categorized patients as non-frail (a score of 0), pre-frail (a score of 1–2), and frail (a score of 3–5).
Statistical Analysis
Continuous variables were expressed as mean value ± standard deviation (mean ± SD) when the normal distribution was met, if not, median with interquartile range was used. Continuous variables were analyzed using the t-test or analysis of variance, and the Bonferroni test was used for post hoc analysis, while categorical variables was analyzed using the Chi-square test or the Fisher's exact test. According to previous studies,16–18 we posited that frailty was significantly related to age. Hence, a 1:1 nearest-neighbor PSM for age, sex, fusion levels, and ASA was implemented between non-frail group and pre-frail group to keep preoperative comparable clinical data as much as possible. Analogously, the same procedure was performed to compare the pre-frail group and frail group. Match tolerance was set at 0.02. Univariate and multivariate logistic regressions were used to identify the impact of clinical demographics on postoperative complications. All statistical analyses were performed using SPSS software version 25.0 (SPSS, Inc., Armonk, NY, USA), and P-values < 0.05 were considered statistically significant.
Results
Baseline Demographics
There were 559 consecutive patients who met the criteria (237 males and 322 females; mean age 72.55 ± 5.86 years). According to the Fried frailty phenotype, 279 were non-frail with 57.3% being female, 185 pre-frail with 60% being female, and 95 were frail with 53.7% being female. The mean ages were 70.48 ± 4.87, 73.38 ± 5.70, and 77.01 ± 5.96 years, respectively. The clinical characteristics are displayed in Table 1. After PSM, there were 147 well-balanced pairs of patients between non-frail and pre-frail group, 84 well-balanced pairs of patients between pre-frail and frail group. The detailed demographic data after PSM are displayed in Table 2.
 |
Table 1 Patient Demographics |
 |
Table 2 Results of Propensity Score Matching Patient Groups |
Postoperative Outcomes
The detailed clinical demographics are displayed in Table 3. After PSM, we found that pre-frail patients were more vulnerable to develop urinary retention (p = 0.031), and surgical site infection (p = 0.021) than non-frail patients. However, there were no significant difference in nausea and vomiting, urinary tract infection, deep venous thrombosis, myocardial ischemia, postoperative intensive care units stays, 30-day readmission, or cerebrospinal fluid leakage between non-frail and pre-frail groups. Compared with pre-frail patients, the LOS was reduced from 7.21 ± 2.99 to 6.35 ± 2.66 days (p = 0.010), the ambulation time was reduced from 2.46 ± 1.29 to 2.06 ± 1.18 days (p = 0.006), and the removal of urinary catheter time was reduced from 2.14 ±1.30 to 1.79 ± 1.12 days (p = 0.015), respectively. Frail patients were more prone to have prolonged LOS (7.06 ± 2.95 versus 8.23 ± 3.40, p = 0.019) than pre-frail patients. However, there were no significant difference in other metrics. Binary logistic regression revealed that CRP and frail status were independently associated with postoperative complications between non-frail and pre-frail patients, while only CRP was independently correlated between pre-frail and frail patients. The detailed outcomes are shown in Table 4.
 |
Table 3 Postoperative Outcomes Between Matching Patient Groups |
 |
Table 4 Binary Logistic Regression for Postoperative Complications Between Matched Groups |
Crp
As an indicator to evaluate the stress response associated with surgery, CRP has been confirmed to be correlated with postoperative complications in previous studies,19–21 Consistent with previous studies, we found that pre-frail patients may be likely to have severe stress response than non-frail patients (12.26 ± 11.68 versus 17.25 ± 25.37 mg/L, p = 0.033) after PSM for age, sex, ASA, and fusion levels. An analogous situation was observed between pre-frail and frail patients (16.84 ± 26.43 versus 26.49 ± 32.73 mg/L, p = 0.038). The characteristics of these groups are expressed in Figure 2.
Discussion
While it is widely accepted that increased age serves as an indicator to predict postoperative complications, however, because the heterogeneity of different population, some younger people can be frail, and some older people can be robust.16 In recent years, the 5-item Fried frailty phenotype was one of the most commonly used indexes evaluating postoperative outcomes.22 Nevertheless, on the one hand, in previous literatures, comparing frailty and age, the superiority of predicting postoperative complications was the focus. In a retrospective analysis of 199 patients, Leung et al23 demonstrated that age was a significant moderator of the relationship between pre-frail and body measures. Analogously, in a retrospective analysis of 8174 patients, performed by Moguilner et al,17 the results of receiver operating characteristic curves indicated that adding age to a frailty index improved its mortality prediction. However, it cannot be ignored that frailty is significantly related to increasing age, verified in previous studies.16–18 On the other hand, in previous literatures, patients were dichotomized into non-frail and pre-frail/frail groups, without considering pre-frail as an independent group.16,24 Therefore, we employed PSM for age, sex, ASA and fusion levels in the present study to guarantee comparable clinical characteristics between groups. Pairwise comparisons were performed to compare the effects of frailty on complications. After PSM, we found that the LOS, the rate of urinary retention and surgical site infection of pre-frail patients were more significant than non-frail patients; meanwhile, the pre-frail patients were more vulnerable to greater stress response associated with surgery than non-frail patients. Binary logistic regression indicated that CRP and pre-frail were independently correlated with postoperative complications between non-frail and pre-frail patients. While there were significant differences only in LOS and CRP between pre-frail and frail patients, this reflected the reasonability of dichotomous grouping in some extent.
Frailty is being increasingly studied as a common characteristic impacting postoperative outcomes in spine surgery. In a prospective cohort analysis of 668 patients following spine surgery and frailty, as distinguished by the risk assessment index, Agarwal et al16 found that pre-frail and frail patients had longer LOS (3.9 d ± 3.6 vs 3.1 d ± 2.8, p < 0.001). In a retrospective cohort study of geriatric patients undergoing single-level lumbar fusion, after PSM, Shahrestani et al24 showed significantly greater LOS (9.9 ± 10.1 versus 4.0 ± 3.9, p < 0.0001) in frail than non-frail patients. In line with previous studies, we found that after PSM, pre-frail patients had longer LOS (7.21 ± 2.99 versus 6.35 ± 2.66, p = 0.010) than non-frail patients and a similar result was found between frail patients and pre-frail patients (8.23 ± 3.40 versus 7.06 ± 2.95, p = 0.019). With the aging population as well as the prevalence of frailty among spine surgery patients, evaluating the impact of frailty on postoperative complications has been a hot topic. In a retrospective review of 426 patients undergoing elective posterior thoracolumbar fusion surgery and frailty, as distinguished by a modified frailty index, Sun et al25 showed that frail was independently associated with adverse events. Shahrestani et al24 reported that frail patients encountered higher rate of urinary tract infection, infection, and 30-day readmission. Nevertheless, in a retrospective review of 5296 patients, Elsamadicy et al18 reported that the modified frailty index did not independently predict complications. In the present study, while there were higher rates of urinary retention (p = 0.031), and surgical site infection (p = 0.021) in pre-frail patients than in non-frail patients, there were no significant differences in other complications, binary logistic regression indicated that pre-frail was independently related to postoperative complications. However, similar results were not observed between pre-frail patients and frail patients. With regard to suboptimal outcomes with pre-frail and frail patients, some measures should be taken. In a recently published study, Porche et al26 reported significantly improved recovery of physiological function and LOS after the implementation of enhanced recovery after surgery. Early ambulation as the backbone of enhanced recovery after surgery may decrease the risk of adverse events for pre-frail/frail patients. The current findings were inconsistent with previous findings from our department. The possible explanations are as follows. First, compared with the results of Sun et al, “the severity of frailty independently predicted minor complications in the short spinal fusion group” whose frailty was evaluated using an 11-item modified frailty index, in the current research, however, we used a 5-item Fried frailty phenotype to describe frail status. Secondly, we performed PSM to offset the effects of confounding factors, increasing the reliability of our findings. The conflicting results suggest that high-quality studies are needed for a more precise evaluation of the impact of frail status on postoperative complications.
In previous studies,27,28 early ambulation significantly reduced the rate of postoperative complications and early mobilization within 24 hours after short-level lumbar fusion surgery was feasible. In our department, all patients receiving short-level fusion surgery were asked to ambulate within 24 hours if there was no patient-reported discomfort. In this matching cohorts, non-frail patients were more likely to ambulate (2.06 ± 1.18 versus 2.46 ± 1.29, p = 0.006) and have the urinary catheter removed earlier than pre-frail patients (1.79 ± 1.12 versus 2.14 ±1.30 p = 0.015). However, there were no significant differences between pre-frail and frail patients.
CRP is a marker of stress responses associated with surgery, which was confirmed to be correlated with postoperative complications.21,29 In the current study, after PSM, more severe stress responses were observed in pre-frail than non-frail patients (Figure 2A) and even frail patients suffered more stress responses than pre-frail patients (Figure 2B), suggesting that pre-frail and frail patients have higher risk of postoperative complications than non-frail patients. Therefore, in the perioperative management, in order to reduce postoperative complications, more attention should be paid to patients identified with pre-frail or frail.
There were several limitations in the present study. First, this was a monocentric, retrospective cohort study, which may have introduced selection bias. Secondly, as we included only patients undergoing short-level lumbar fusion surgery, after PSM, there were only 84 well-balanced patients between pre-frail and frail groups, the small sample sizes may lead to the biased results. Despite these limitations, segregating patients into three groups according to Fried frailty phenotype and comparing them stepwise represents a novel attempt to evaluate the impact of frailty on postoperative complications.
Conclusion
In this study, after PSM, we found higher rates of urinary retention and surgical site infection in pre-frail patients than non-frail patients. CRP was independently related to postoperative complications, while frail status was only independently associated with postoperative complications between pre-frail and non-frail patients.
Data Sharing Statement
The data used to support the findings of this study were included within the article.
Ethics Approval and Consent to Participate
The institutional review board in Xuanwu Hospital Capital Medical University approved the study (No. 2018008), which followed the Declaration of Helsinki principles. A written informed consent was obtained from all the participants in this study.
Acknowledgments
We thank the Department of Orthopedics, Xuanwu Hospital Capital Medical University staff and all the patients who participated in the study.
Funding
This work was supported by the Beijing Municipal Health Commission (Jing 2019-2), Beijing Hospitals Authority’s Ascent Plan (DFL20190802) and Beijing Hospitals Authority Clinical Medicine Development of Special Funding Support (XMLX202116). The funders played no role in the design of this study, the collection, analysis and interpretation of data, or preparation of the manuscript. The funders played no role in the design of this study, the collection, analysis and interpretation of data, or preparation of the manuscript.
Disclosure
Peng Cui and Peng Wang are co-first authors. The authors declare that there are no conflicts of interest in this work.
References
1. Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78:606–617. doi:10.1093/bja/78.5.606
2. Elsarrag M, Soldozy S, Patel P, et al. Enhanced recovery after spine surgery: a systematic review. Neurosurg Focus. 2019;46(4):E3. doi:10.3171/2019.1.FOCUS18700
3. Ljungqvist O. ERAS–enhanced recovery after surgery: moving evidence-based perioperative care to practice. JPEN J Parenter Enteral Nutr. 2014;38(5):559–566. doi:10.1177/0148607114523451
4. Wang P, Wang Q, Kong C, et al. Enhanced recovery after surgery (ERAS) program for elderly patients with short-level lumbar fusion. J Orthop Surg Res. 2020;15(1):299. doi:10.1186/s13018-020-01814-3
5. Debono B, Sabatier P, Boniface G, et al. Implementation of enhanced recovery after surgery (ERAS) protocol for anterior cervical discectomy and fusion: a propensity score-matched analysis. Eur Spine J. 2021;30(2):560–567. doi:10.1007/s00586-020-06445-0
6. Cui P, Wang P, Kong C, et al. Patients older than 75 years undergoing polysegmental lumbar fusion surgery can also benefit from enhanced recovery after surgery program. Clin Interv Aging. 2022;17:245–252.
7. Strickland AR, Usmani MF, Camacho JE, et al. Evaluation of risk factors for postoperative Urinary Retention in Elective Thoracolumbar spinal fusion patients. Global Spine J. 2021;11(3):338–344. doi:10.1177/2192568220904681
8. Kong C, Li X, Sun X, et al. Complications in elderly patients undergoing lumbar arthrodesis for spinal stenosis. World Neurosurg. 2019;132:e949–e955. doi:10.1016/j.wneu.2019.06.147
9. Ansari D, DesLaurier JT, Patel S, et al. Predictors of extended hospitalization and early reoperation after elective lumbar disc arthroplasty. World Neurosurg. 2021;154:e797–e805. doi:10.1016/j.wneu.2021.08.016
10. Beauchamp-Chalifour P, Flexman A, Street J, et al. The impact of frailty on patient-reported outcomes after elective thoracolumbar degenerative spine surgery. J Neurosurg Spine;2021. 1–9. doi:10.3171/2021.2.SPINE201879
11. Jung J, Chung C, Kim C, et al. The modified 11-Item frailty index and postoperative outcomes in patients undergoing lateral lumbar interbody fusion. Spine. 2022;47(5):396–404. doi:10.1097/BRS.0000000000004260
12. Ljungqvist O, de Boer HD, Balfour A, et al. Opportunities and challenges for the next phase of enhanced recovery after surgery: a review. JAMA Surg. 2021;156(8):775–784. doi:10.1001/jamasurg.2021.0586
13. Wolf JH, Hassab T, D’Adamo CR, et al. Frailty is a stronger predictor than age for postoperative morbidity in Crohn’s disease. Surgery. 2021;170(4):1061–1065. doi:10.1016/j.surg.2021.04.030
14. Santarpino G, Condello I, Serraino GF, et al. Age, comorbidities, frailty: who comes first? J Card Surg. 2021;36(7):2407–2409. doi:10.1111/jocs.15543
15. Fried L, Tangen C, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol a Biol Sci Med Sci. 2001;56(3):M146–156. doi:10.1093/gerona/56.3.M146
16. Agarwal N, Goldschmidt E, Taylor T, et al. Impact of frailty on outcomes following spine surgery: a prospective cohort analysis of 668 patients. Neurosurgery. 2021;88(3):552–557. doi:10.1093/neuros/nyaa468
17. Moguilner S, Knight SP, Davis JRC, et al. The importance of age in the prediction of mortality by a frailty index: a machine learning approach in the Irish Longitudinal Study on Ageing. Geriatrics. 2021;6:3. doi:10.3390/geriatrics6010003
18. Elsamadicy A, Freedman I, Koo A, et al. Modified-frailty index does not independently predict complications, hospital length of stay or 30-day readmission rates following posterior lumbar decompression and fusion for spondylolisthesis. Spine J. 2021;21(11):1812–1821. doi:10.1016/j.spinee.2021.05.011
19. Cabellos Olivares M, Labalde Martinez M, Torralba M, et al. C-reactive protein as a marker of the surgical stress reduction within an ERAS protocol (Enhanced Recovery After Surgery) in colorectal surgery: a prospective cohort study. J Surg Oncol. 2018;117(4):717–724. doi:10.1002/jso.24909
20. Kim J, Jung J, Lee J, et al. Can whole spine magnetic resonance imaging predict radiographic progression and inflammatory activity in axial spondyloarthritis? Joint Bone Spine. 2022;89(4):105352. doi:10.1016/j.jbspin.2022.105352
21. Hoeller S, Roch P, Weiser L, et al. C-reactive protein in spinal surgery: more predictive than prehistoric. Eur Spine J. 2021;30(5):1261–1269. doi:10.1007/s00586-021-06782-8
22. Roopsawang I, Zaslavsky O, Thompson H, et al. Frailty measurements in hospitalised orthopaedic populations age 65 and older: a scoping review. J Clin Nurs. 2021;31:1149–1163. doi:10.1111/jocn.16035
23. Leung AYM, Sun Q, Kwan RYC, et al. Moderating effect of age on the relationships between pre-frailty and body measures. Health Soc Care Community. 2021;29(2):515–525. doi:10.1111/hsc.13114
24. Shahrestani S, Ton A, Chen XT, et al. The influence of frailty on postoperative complications in geriatric patients receiving single-level lumbar fusion surgery. Eur Spine J. 2021;30(12):3755–3762. doi:10.1007/s00586-021-06960-8
25. Sun W, Lu S, Kong C, et al. Frailty and post-operative outcomes in the older patients undergoing elective posterior thoracolumbar fusion surgery. Clin Interv Aging. 2020;15:1141–1150.
26. Porche K, Yan S, Mohamed B, et al. Enhanced recovery after surgery (ERAS) improves return of physiological function in frail patients undergoing 1-2 level TLIFs: an observational retrospective cohort study. Spine J. 2022;22:1513–1522. doi:10.1016/j.spinee.2022.04.007
27. Debono B, Wainwright TW, Wang MY, et al. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Spine J. 2021;21(5):729–752. doi:10.1016/j.spinee.2021.01.001
28. Burgess L, Wainwright T. What is the evidence for early mobilisation in elective spine surgery? A narrative review. Healthcare. 2019;7:3.
29. Jiang W, Shi H, Deng X, et al. The incidence of incision infections after lumbar fusion and the significance of dynamically monitoring serum albumin and C-reactive protein levels. Ann Palliat Med. 2021;10(10):10870–10877. doi:10.21037/apm-21-2512
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

