Back to Journals » Clinical Ophthalmology » Volume 16
The Effects of Angle Kappa on Clinical Results and Patient-Reported Outcomes After Implantation of a Trifocal Intraocular Lens
Authors Sandoval HP, Potvin R , Solomon KD
Received 23 February 2022
Accepted for publication 19 April 2022
Published 27 April 2022 Volume 2022:16 Pages 1321—1329
DOI https://doi.org/10.2147/OPTH.S363536
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Helga P Sandoval,1 Richard Potvin,2 Kerry D Solomon1
1Carolina Eyecare Physicians, LLC, Mt. Pleasant, SC, USA; 2Science in Vision, Bend, OR, USA
Correspondence: Kerry D Solomon, Carolina Eyecare Physicians, LLC, 1101 Clarity Road, Suite 100, Mt Pleasant, SC, 29464, USA, Email [email protected]
Purpose: To objectively determine if angle kappa materially influenced clinical outcomes or patient-reported satisfaction and visual quality of patients implanted with a trifocal intraocular lens (IOL).
Methods: This was a non-interventional study of clinical outcomes. Subjects were patients choosing to be bilaterally implanted with a trifocal IOL (PanOptix®) who were then evaluated 3 months postoperative. Angle kappa (AK) was measured before surgery and at the 3-month visit. The 3-month visit included a manifest refraction, and measurement of uncorrected and distance corrected acuity at 4 m, 60 cm and 40 cm. Visual quality and satisfaction questionnaires were also administered.
Results: Data from 56 eyes of 28 subjects were analyzed; 26 eyes had an AK magnitude < 0.3 mm, 14 had an AK from 0.3 mm to less than 4 mm and 16 had an AK ≥ 0.4 mm. Neither visual disturbances (eg, glare, halos, starbursts), satisfaction nor spectacle dependence were correlated to the magnitude of angle kappa. The magnitude of postoperative AK was significantly lower than preoperative (0.24 ± 0.12 mm vs 0.30 ± 0.16 mm, p < 0.01).
Conclusion: The magnitude of preoperative Angle Kappa had no apparent effect on the refractive, visual acuity or subjective (visual disturbances, quality of vision, satisfaction) clinical outcomes with this trifocal IOL. The magnitude of angle kappa was significantly lower after surgery.
Keywords: angle kappa, trifocal IOL, cataract surgery
Plain Language Summary
Cataract surgery is a common surgical procedure where the clouded natural lens is removed and replaced with an artificial lens. One option for this intraocular lens (IOL) is a trifocal design, which is expected to provide good vision at distance, intermediate and near. Overall results with trifocal IOLs have been very good. One factor that surgeons often think might affect results is the degree of alignment of the different components of the eye. There are several different measures of how the components of the eye are arranged. One such measure is Angle Kappa, the angular difference between the direction one is looking (visual axis) and the center of the pupil. We conducted the current study to determine if differences in Angle Kappa were associated with postoperative results, including visual disturbances, patient satisfaction and the patient’s eyeglass prescription after surgery. We found that Angle Kappa had no association with clinical results. We also found that Angle Kappa changed after cataract surgery.
Introduction
Multifocal intraocular lenses (IOLs) are now in relatively common use after cataract surgery. Patient selection and setting appropriate expectations are two important considerations when implanting these lenses. While near vision is likely to be significantly better with a multifocal IOL, the potential for visual disturbances appears to be higher than for monofocal IOLs.1,2 Minimizing the incidence and severity of visual disturbances such as glare and halos is important to patient satisfaction, as photic phenomena have been demonstrated to be significant factors associated with dissatisfaction after multifocal IOL implantation.3,4
Some studies have suggested that a high angle kappa (AK) may be a contributing factor to optical quality and visual disturbances with diffractive and zonal refractive multifocal IOLs. Angle kappa is defined as the angular difference between the visual axis (determined by patient fixation) and the pupil center. While it is defined as an angle, it cannot be determined without anterior tomography of the eye. As a proxy, it is often measured as a magnitude and direction in front/plan view from an image of the eye when the patient is fixating. Figure 1 shows a cross-sectional view of the eye with AK illustrated, and a front view showing the pupil center and the location of AK on the cornea (the center of fixation on the measuring instrument, shown here as “X”). For the purposes of this study, AK is measured as the vector between the pupil center and “X”. Note that angles have been exaggerated for clarity. There a high correlation between the true angle kappa and this measured vector in front view but it will vary slightly with the internal anatomy of the eye (eg anterior chamber depth).
Figure 2 shows an actual image of the angle kappa calculation from the Nidek OPD-Scan III (Nidek USA, Inc., San Jose, USA), the instrument used to measure AK in this study. The OPD-Scan III uses the eye image from a fixating patient. The center of the pupil is calculated and the position of the corneal reflex indicates the line of sight (the usual proxy for the visual axis). The vector difference between the two points can then be determined. There are separate vectors for the mesopic and photopic pupils, as the pupil center can vary with different light conditions.
Fu et al found correlations between AK and objective visual measures such as the Strehl ratio and Optical Scattering Index in patients implanted with the Tecnis SymfonyTM IOL (Johnson and Johnson Vision, Santa Ana, USA), but the observed correlations were weak.5 Prakash et al found correlations between AK and the severity of glare and halos, but noted that many patients with high AK were also asymptomatic; again, the correlations were significant, but weak.6 All patients in their study had the ReZoom™ zonal refractive IOL implanted (Johnson and Johnson Vision, Santa Ana, USA). Qi et all found no objective differences correlated to AK but reported more visual disturbances with very high AK values (> 0.50 mm); their patients were implanted with a diffractive trifocal IOL.7 Other studies involving trifocal IOLs found no correlations between angle kappa and any measures of vision or visual quality.8,9
The purpose of this study was to determine if angle kappa (measured preoperatively) had any apparent effect on clinical or patient-reported outcomes in patients undergoing cataract surgery with implantation of the AcrySof® IQ PanOptix® IOL (Alcon, Fort Worth, USA) trifocal IOL.
Methods
This study was a prospective single-arm study, approved by an institutional review board (Salus IRB, Austin, TX) and registered with clinicaltrials.gov (NCT04242875). The study was conducted in a manner consistent with good clinical practice and the tenets of the declaration of Helsinki. Subjects were recruited from presenting patients over the age of 40 who were interested in reducing their dependence on spectacles for distance, intermediate and near vision after surgery, and who chose to have the PanOptix trifocal (toric or non-toric version) implanted in both eyes. They had to be eligible for bilateral implantation of this IOL, with potential acuity of 0.2 logMAR (20/32 Snellen) or better in both eyes. Eyes with ocular pathology that would be likely to influence visual outcomes were excluded, as were those with prior refractive or corneal surgery and those with severe dry eye. Subjects with an additional planned surgery (eg, glaucoma device implant) were also excluded. Any subjects with complications at the time of surgery were discontinued from the study and followed for safety reporting but their postoperative data were not included in the reported clinical results. All subjects signed an appropriate informed consent document. Data are not available for sharing.
For each eye, the biometry was measured with the Lenstar® LS900 (Haag-Streit AG, Koeniz, Switzerland). The selected sphere power for all but four lenses was based on the Barrett Universal II formula. If astigmatism correction was necessary, where appropriate, the surgeon used the toric version of the trifocal IOL, or (for lower levels of cornea astigmatism) performed limbal relaxing incisions with a laser (LenSx® Femtosecond Laser System, Alcon, Fort Worth, TX). Toric IOL cylinder power was calculated using the Barrett Toric Calculator, which compensates for posterior corneal astigmatism. Intraoperative aberrometry was not used. Femtosecond laser-assisted arcuate incisions were planned using the Donnenfeld nomogram, with the net astigmatism calculated by Veracity Surgical planning software (Carl Zeiss Meditec, Inc., Dublin, CA).
Angle kappa was measured preoperatively using the OPD-Scan III (Nidek Co., Ltd., Aichi, Japan). As noted above, a proxy for the actual angle was recorded - the magnitude of the difference between the pupil center and the visual axis in photopic conditions as seen in the ocular image (P_dist). This is a linear, rather than angular, measurement but is in common use. The orientation of AK was also recorded. A second measurement of AK was made with the same device at the 3-month visit. Results were categorized for analysis into 3 groups, based on the preoperative AK magnitude: 0 to < 0.3 mm, 0.3 mm to < 0.4 mm, and ≥ 0.4 mm. (In a previous study Qi et al used 0.4 mm as one of their cutoff values to categorize results.7)
All surgeries were performed by the same surgeon (KDS) with the clinic’s usual standard of care. No direct attempts were made to align the center of the implanted IOL to any specific reference points – the IOL was centered on the visual axis.
A quality of vision questionnaire (QUVID)10 was administered to all subjects at the 3-month visit, asking about the frequency, severity, and degree of bother of potential visual disturbances, from double or blurred vision to glare and halos. Satisfaction with vision was also evaluated with a questionnaire (IOLSAT),10 which allowed subjects to indicate their relative need for spectacles at various distances (and overall) and their satisfaction with the surgery. Results were categorized by preoperative angle kappa group based on the eye with the highest angle kappa from each patient.
Data analysis was performed using Statistica data analysis software, version 12 (TIBCO Software Inc., Palo Alto, CA, USA). Parametric comparisons were made using an analysis of variance (ANOVA) while categorical data were analyzed using appropriate non-parametric tests.
Results
Thirty subjects were enrolled, with two discontinued due to surgical complications - one presumed allergic reaction to the prophylactic NSAID, resulting in cancellation of second eye surgery, and one posterior capsule tear. Data from 56 eyes of 28 subjects were available for analysis at the 3-month visit. Relevant demographic, biometric and operative details are summarized in Table 1. There were 26 eyes with an AK < 0.3 mm, 14 with an AK from 0.3 mm to less than 4 mm and 16 with an AK ≥ 0.4 mm. There was no statistically significant difference between the preoperative MRSE, preoperative cylinder or IOL sphere power between the 3 AK classification groups.
 |
Table 1 Demographic, Biometric and Operative Details (28 Subjects, 56 Eyes) |
Table 2 contains summary postoperative refractive and monocular visual acuity data. All but 3 eyes (53/56, 95%) had a postoperative mean spherical equivalent refraction within 0.50 D of plano with ≤ 0.50 D of refractive cylinder. Results were analyzed with respect to AK categorization; there were no statistically significant differences by AK group for any of the listed variables (p values are shown, though the categorized data are not).
 |
Table 2 Summary of Postoperative Refractive and VA Outcomes |
Figure 3 shows the overall reported frequency of the 7 visual disturbances included in the QUVID questionnaire. Glare, halos, and starbursts were the most often reported. Figure 4 shows the reported frequency of glare, halos, and starbursts by AK group. (There were 10 subjects with an AK magnitude < 0.3 mm, 6 with an AK magnitude from 0.3 mm to less than 4 mm and 12 with an AK magnitude ≥ 0.4 mm.) There was a statistically significant difference only in the frequency of starbursts by AK group (Kruskal–Wallis test, p = 0.01). This was driven by the higher frequency of starbursts in the group with the lowest AK. While not shown, there were no statistically significant differences in either the severity or degree of bother for glare, halos, or starbursts by AK group.
 |
Figure 3 Frequency of visual disturbances reported. *Negative dysphotopsia. |
 |
Figure 4 Frequency of starbursts (top), halos (middle) and glare (bottom) by categorical magnitude of angle kappa. Abbreviation: AK, angle kappa (vector magnitude). |
Eighty-two percent of subjects (22/28) reported never needing glasses to see. There was no statistically significant difference in the need for glasses by AK group (p = 0.66). Table 3 summarizes the reported ability to see objects at various distances in varying light conditions. There was no statistically significant difference between the AK groups in the reported ability to see for any distance or light condition; the relevant p-values are shown. The p-values were based on an analysis of variance (ANOVA) of the given variable by AK group. Because they were not statistically significantly different, specific values for each group are not listed. Finally, 25 of 28 subjects (89%) were “satisfied” or “very satisfied” with their vision after surgery. Overall satisfaction was not statistically significantly different by AK group (Kruskal–Wallis test, p = 0.78). Ninety-six percent of subjects (27/28) would have the same lens implanted again and the same percentage would recommend the lens to family or friends. The only subject who would not have the lens implanted again or recommend it to family and friends had a preoperative AK of 0.18 in both eyes and postoperative AKs lower than preoperative.
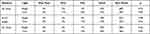 |
Table 3 Reported Ability to See at Various Distances in Dim and Bright Light |
The measurement of AK postoperatively was of interest because planning based on preoperative AK will be less helpful if there are significant changes to AK with surgery. The magnitude of postoperative AK was significantly lower than preoperative (0.24 ± 0.12 mm vs 0.30 ± 0.16 mm, p < 0.01). Table 4 shows the change in categorization after surgery. Only half of the eyes had the same category before and after surgery; 41% of eyes (23/56) had a decrease of 0.1 mm or more and 11% of eyes (6/56) had an increase of 0.1 mm or more.
 |
Table 4 Change in AK Categorization After Surgery |
Note that the values above are the preoperative and postoperative magnitudes of the angle kappa vectors. Figure 5 shows the preoperative and postoperative magnitudes and orientations for the angle kappa vectors in the right and left eyes separately. The mean vector change in angle kappa for all eyes was 0.19 ± 0.14 mm, with a range of 0.03 to 0.79 mm. This includes the effect of a change in orientation as well. Table 5 shows the preoperative and postoperative centroid values of AK by eye. The greatest change was in the “X” component in the right eye.
 |
Table 5 Preoperative and Postoperative AK Centroid Values by Eye |
Discussion
The current study was designed to determine if angle kappa was associated with suboptimal results in terms of refraction, visual acuity or subjective measures of visual quality and satisfaction after implantation of a trifocal IOL.
Overall refractive and visual acuity results obtained here are consistent with prior reports in the literature.10–13 As shown in Table 2, the manifest refraction and visual acuity were not statistically significantly different by AK group. These findings appear to corroborate the results reported by Garzón et al8 and Velasco-Barona et al,9 though the first study related to a different trifocal IOL. The refractive and acuity results also appear consistent with the results from Qi et al,7 where visual disturbances, but not refraction and acuity, appeared related to higher AK values. Again, a different trifocal IOL was evaluated in that study.
The visual disturbances reported in the present study were also not correlated with the measured magnitude of AK. Fu et al reported negative effects of AK on objective visual quality for a diffractive EDOF lens, but no subjective effects.5 Harrer et al reported a wide range of values for AK, but only weak associations between AK and higher order aberrations post-surgery.11 The current study also found no association between AK and subjective satisfaction, using the larger AK value of the two eyes to categorize subjects. It would appear the trifocal studied here is robust to differences in angle kappa in the subject population. Detailed optical simulation by Karhanová et al suggests that the magnitude of AK required to cause visual disturbances with a diffractive bifocal IOL (by interaction with the inmost diffractive ring) was higher than the value found in a normal population.12 They suggested that angle kappa need only be measured in eyes with very shallow anterior chambers, though they did not provide a specific guideline depth. The trifocal studied here has an inmost ring that is further away from the center than the studied bifocal, which would further reduce the likelihood of any issues.
The maximum IOL power implanted in the current study was +26.0 D, so very high hyperopes (who are more likely to have very shallow anterior chambers) may not have been represented in the analysis. However, a review of recent surgery cases in the practice showed that only 33 of the most recent 2000 eyes (1.6%) operated on had an IOL power greater than 26.0D implanted.
The changes in angle kappa reported here have been observed by previous researchers, with mean AK observed to be significantly lower postoperatively.8,13 The findings illustrated in Figure 5 appear consistent with those of Wang et al, as does the mean vector change observed.13 The observed change in AK from preoperative to postoperative in eyes, along with a lack of correlation between AK and either objective or subjective results, calls into question the value of using preoperative angle kappa as a limiting factor in implanting multifocal IOLs. While the specific reason(s) for changes in AK after cataract surgery do not appear to have been researched, the differences in the tilt and decentration of the IOL relative to the original crystalline lens, and the change in effective lens position, are likely factors.
There are limitations to this study. The number of subjects/eyes enrolled was limited. Analysis of the effects of angle kappa were restricted to consideration of the (linear) magnitude, with no sub-analysis related to the orientation of the displacement. The potential confounding effect of other biometric parameters of the eye was also not evaluated; theoretical research suggests that this may be an important consideration.12 Finally, because the proxy value of AK was used, rather than the actual angle (which can only be determined with anterior chamber tomography systems), comparisons with previous findings based on the actual angle were not possible.13
In summary, we found no effect of higher levels of angle kappa on objective (refraction, visual acuity) or subjective (visual disturbances, quality of vision, satisfaction) clinical outcomes with this trifocal IOL. Finally, changes in angle kappa after surgery appear likely.
Funding
This work was supported by an investigator-initiated study grant from Alcon (IIT# 56239531).
Disclosure
Richard Potvin is a consultant to Alcon and Carl Zeiss Meditec. Helga P Sandoval reports grants from Alcon. Kerry D Solomon is a consultant for Alcon Laboratories, Allergan, Aquesys, Bausch and Lomb, Clarvista Medical, Glaukos, Icon Bioscience, Imprimis, Integrity Digital Solutions, Johnson & Johnson Vision, Kala Pharmaceuticals, Lenstec, Mati Therapeutics, Octane Visionary VC Fund, Ocuhub, Omeros Corporation, Pogotec, PRN, Tearlab, Versuant, and RxSight. The authors report no other conflicts of interest in this work.
References
1. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12(12):CD003169. PMID: 27943250; PMCID: PMC6463930. doi:10.1002/14651858.CD003169.pub4
2. Khandelwal SS, Jun JJ, Mak S, Booth MS, Shekelle PG. Effectiveness of multifocal and monofocal intraocular lenses for cataract surgery and lens replacement: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2019;257(5):863–875. PMID: 30627791. doi:10.1007/s00417-018-04218-6
3. Gibbons A, Ali TK, Waren DP, Donaldson KE. Causes and correction of dissatisfaction after implantation of presbyopia-correcting intraocular lenses. Clin Ophthalmol. 2016;10:1965–1970. PMID: 27784985; PMCID: PMC5066995. doi:10.2147/OPTH.S114890
4. de Vries NE, Webers CA, Touwslager WR, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859–865. PMID: 21397457. doi:10.1016/j.jcrs.2010.11.032
5. Fu Y, Kou J, Chen D, et al. Influence of angle kappa and angle alpha on visual quality after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2019;45(9):1258–1264. PMID: 31326223. doi:10.1016/j.jcrs.2019.04.003
6. Prakash G, Prakash DR, Agarwal A, Kumar DA, Agarwal A, Jacob S. Predictive factor and kappa angle analysis for visual satisfactions in patients with multifocal IOL implantation. Eye. 2011;25(9):1187–1193. PMID: 21681216; PMCID: PMC3178249. doi:10.1038/eye.2011.150
7. Qi Y, Lin J, Leng L, et al. Role of angle κ in visual quality in patients with a trifocal diffractive intraocular lens. J Cataract Refract Surg. 2018;44(8):949–954. PMID: 30033112. doi:10.1016/j.jcrs.2018.05.026
8. Garzón N, García-Montero M, López-Artero E, et al. Influence of angle κ on visual and refractive outcomes after implantation of a diffractive trifocal intraocular lens. J Cataract Refract Surg. 2020;46(5):721–727. PMID: 32358267. doi:10.1097/j.jcrs.0000000000000156
9. Velasco-Barona C, Corredor-Ortega C, Mendez-Leon A, et al. Influence of Angle κ and higher-order aberrations on visual quality employing two diffractive trifocal IOLs. J Ophthalmol. 2019;2019:7018937. PMID: 31885892; PMCID: PMC6900936. doi:10.1155/2019/7018937
10. Modi S, Lehmann R, Maxwell A, et al. Visual and patient-reported outcomes of a diffractive trifocal intraocular lens compared with those of a monofocal intraocular lens. Ophthalmology. 2021;128(2):197–207. PMID: 33004211. doi:10.1016/j.ophtha.2020.07.015
11. Harrer A, Hirnschall N, Tabernero J, et al. Variability in angle κ and its influence on higher-order aberrations in pseudophakic eyes. J Cataract Refract Surg. 2017;43(8):1015–1019. PMID: 28917399. doi:10.1016/j.jcrs.2017.05.028
12. Wang R, Long T, Gu X, Ma T. Changes in angle kappa and angle alpha before and after cataract surgery. J Cataract Refract Surg. 2020;46(3):365–371. PMID: 32050219. doi:10.1097/j.jcrs.0000000000000063
13. Karhanová M, Pluháček F, Mlčák P, Vláčil O, Šín M, Marešová K. The importance of angle kappa evaluation for implantation of diffractive multifocal intra-ocular lenses using pseudophakic eye model. Acta Ophthalmol. 2015;93(2):e123–8. PMID: 25160117. doi:10.1111/aos.12521
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Evaluation of Refractive Accuracy of ORA and the Factors Impacting Residual Astigmatism in Patients Implanted with Trifocal IOLs During Cataract Surgery: A Retrospective Observational Study
Watanabe K
Clinical Ophthalmology 2022, 16:2491-2503
Published Date: 10 August 2022
Visual Function After Implantation of Trifocal and Trifocal Toric Intraocular Lenses Using Intraoperative Aberrometry
Brissette A, Cole B, Hall B
Clinical Ophthalmology 2024, 18:1547-1554
Published Date: 30 May 2024



