Back to Journals » Clinical Ophthalmology » Volume 17
The Effect of Upper Eyelid Blepharoplasty on Corneal Tomography and Epithelial Profile
Authors Carreira P , Loureiro T , Carreira AR, Gouveia-Moraes F , Cardoso A, Sampaio A, Campos P, Rodrigues-Barros S, Machado I, Campos N
Received 5 September 2023
Accepted for publication 16 October 2023
Published 12 December 2023 Volume 2023:17 Pages 3801—3807
DOI https://doi.org/10.2147/OPTH.S426034
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Pedro Carreira, Tomás Loureiro, Ana Rita Carreira, Filipe Gouveia-Moraes, Ana Cardoso, Audrey Sampaio, Paul Campos, Sandra Rodrigues-Barros, Ines Machado, Nuno Campos
Centro de Responsabilidade Integrada de Oftalmologia, Hospital Garcia de Orta, Almada, Portugal
Correspondence: Tomás Loureiro, Centro de Responsabilidade Integrada de Oftalmologia, Hospital Garcia de Orta, E.P.E, Av. Torrado da Silva, Almada, 2805-267, Portugal, Email [email protected]
Introduction: Upper tarsal mechanical forces influence corneal epithelial thickness profile, which could modulate corneal astigmatism. Upper eyelid blepharoplasty reduces upper tarsal strength and may have an impact on ocular surface. The aim of this study is to evaluate the effect of upper eyelid blepharoplasty on corneal epithelial thickness profile, astigmatism and aberrations.
Methods: Patients with dermatochalasis underwent bilateral upper eyelid blepharoplasty. Anterior segment optical coherence tomography (AS-OCT) (Zeiss Cirrus 5000 HD-OCT) and Pentacam (Oculus, Wetzlar Germany) were performed before surgery and in the 8th postoperative week. Corneal epithelial thickness, keratometry, aberrations and asphericity were considered for statistical purposes. Only right eyes were considered. A p-value lower than 0.05 was considered significant.
Results: Thirty eyes of 30 patients were included. The degree of astigmatism did not change after surgery (0.95D vs 0.83D, p=0.23). The difference between preoperative and postoperative steepest axis was 3.1° (p=0.04) with a tendency to change toward the vertical meridian. Mean epithelial thickness was higher in the inferior region both pre- and postoperatively and did not change. ET in the superior octant was lower (42 μm vs 45 μm, p< 0.01) and the difference between inferior and superior octants (I-S) was higher (7 μm vs 3 μm, p< 0.001) before surgery. There were no statistically significant changes in corneal aberrations (p=0.52) and asphericity (p=0.41) after surgery.
Conclusion: Our results support that upper tarsus pressure influences epithelial thickness profile and, consequently, the corneal steepest keratometry. These results lead us to postulate that upper eyelid blepharoplasty may influence biometric and keratometric measurements.
Keywords: Blepharoplasty, Epithelial Thickness, Corneal Tomography, Anterior-Segment Optical Coherence Tomography
Introduction
The corneal epithelium contributes to the refractive power of the eye and the profile of epithelial thickness (ET) is of increasing interest in many ophthalmologic diseases. ET is not homogeneously distributed and tends to change to compensate for corneal curvatures and stromal irregularities and restore a regular and smooth ocular surface.1
The epithelium is thinner in superior areas of corneas without pathology. Many different theories have been developed to justify this asymmetry, but there is still consensus. However, Dan Reinstein, using very high-frequency ultrasound – a contact method that excludes the influence of the tear film on the measurement of epithelial thickness – has suggested the mechanical effect of the upper tarsus in the superior epithelium as the main reason for this asymmetry, which is the most acceptable theory.2 Dermatochalasis refers to laxity of the eyelid skin with excessive wrinkling and is common in the elderly. Despite the cosmetic problem, dermatochalasis usually results in ocular surface disturbance and patients report dry eye-like symptoms. Previous work has reported an inflammatory state that is accompanied by poor BUT and Schirmer I-test.3 Upper eyelid blepharoplasty is the treatment of choice for dermatochalasis and reduces the strength of the upper eyelid structures that may affect the ocular surface.4–6 However, to the best of our knowledge, the epithelial thickness profile has never been studied in patients undergoing to blepharoplasty.
The purpose of this study is to evaluate the effect of upper eyelid blepharoplasty on corneal epithelial thickness profile, corneal astigmatism, and corneal aberrations in patients undergoing bilateral upper eyelid blepharoplasty.
Methods
This was a prospective study that included patients with dermatochalasis affecting daily activities who underwent bilateral upper eyelid blepharoplasty by the same oculoplastic surgeon between February 2022 and October 2022. The study was conducted according to the tenets of the Declaration of Helsinki. Written informed consent was obtained from each participant, and IRB approval was obtained from the Comissão de Ética para a Saúde do Hospital Garcia de Orta (Almada, Portugal).
Patients with a history of gross eyelid pathology other than dermatochalasis, ocular surface disease such as pterygium or dry eye, defined by a breakup time (BUT) <10 seconds or any positive staining,7 were excluded. The history of corneal refractive surgery, contact lens wear in the past 3 months, best corrected visual acuity (BCVA) <0.4logMar, and a manifest refractive cylinder greater than 2.00 diopters (D) also excluded patients from the study. Eyes with regular topographic patterns and Belin-Ambrosio Deviation Value <1.22 were included in this study.8 Patients were not prescribed artificial tears during the study.
Routine ophthalmologic examination was performed according to the protocol: uncorrected (UCVA) and best-corrected distance visual acuity (BCVA) both in logMAR, spherical equivalent (SE), biomicroscopy of the anterior segment and fundoscopy. Corneal tomography using Pentacam (Oculus, Wetzlar Germany) and Anterior-Segment Optical Coherence Tomography (AS-OCT) using Zeiss Cirrus 5000 HD-OCT were performed and the upper eyelid was lifted with the doctor’s finger without applying pressure to the eye. Patients were evaluated before surgery and at the 8th postoperative week.
Corneal astigmatism, both degree and axis, and asphericity were registered. Corneal aberrations were automatically analyzed and presented as root-mean square (RMS) values at a pupil size of 6 mm.9 Total aberrations, low-order aberrations (LOA) and high order (HOA) were considered. The difference between the baseline and the 8th postoperative week was calculated for corneal astigmatism and steepest axis.
ET was measured automatically by anterior segment spectral-domain Zeiss Cirrus 5000 (Carl Zeiss Meditec, Inc., Dublin, CA, USA). The ET map included eight radial scans (1024 axial scans each) repeated five times. Patients were positioned on the headrest, looking at the fixation light so that the scan was centered on the pupil center. For each eye, the same examiner performed two scans with a one-minute interruption and recorded the average values. The software algorithm measured epithelial thickness as the distance between the center of the first (tear film) and second (anterior surface of Bowman’s layer) hyperreflective lines on the B-scan. Data were exported and processed using Cirrus HD-OCT review software (version 10.0) which provides an average automatic ET of three concentric ring-shaped zones centered on the center of the cornea (central (CET): 0–2 mm, paracentral: 2–5 mm, and midperipheral: 5–7 mm). ET has also been shown for specific octants of the cornea: superior (S), inferior (I), temporal (T), nasal (N), superonasal (SN), superotemporal (ST), inferotemporal (IT), and inferonasal (IN) within the paracentral and midperipheral zones.10 Differences between the corresponding corneal octants were calculated automatically.
Statistical analysis was performed using SPSS statistical software (version 25, SPSS Inc, Chicago, IL). For statistical purpose, only the right eye from each patient was considered. Quantitative variables were presented as mean ± standard deviation (range). Continuous variables were tested for meeting the normality conditions of the Shapiro–Wilk test. The Wilcoxon test was performed to compare ET, keratometry, corneal aberrations and asphericity at baseline and after blepharoplasty. Correlations were tested using Spearman correlation coefficient. Statistical significance was defined as <0.05.
Results
Thirty-five eyes of 35 patients were initially included. Three patients were excluded because of insufficient exam quality, and two were lost to follow-up, so thirty eyes (n=30) were included in this study.
Our population included 23 women (76.6%) and 7 men (30.4%). The mean age was 64.1 ± 9.1 (45–78) years. There were no surgical complications and no patient had lagophthalmos or blink impairment in the postoperative period.
The general ophthalmologic and corneal tomographic data are shown in Table 1. There were no differences in mean UCVA (p=0.66), mean BCVA (p=0.89) and SE (p=0.37) before surgery and at the 8th postoperative week.
 |
Table 1 General Ophthalmological and Corneal Tomographic Data |
Steepest keratometry was lower after surgery (44.31 ± 1.93 vs 44.04 ± 1.63, p=0.04). The degree of astigmatism did not change (0.95D vs 0.83D, p=0.23). The steepest axis changed with a tendency towards the vertical meridian after surgery (74.2 ± 42.51 vs 77.3 ± 39.71, p=0.04). The flattest, mean, and maximum keratometry did not show statistically significant differences after surgery. Corneal aberrations did not change after surgery: total (1.74 ± 1.31 vs 1.65 ± 1.23, p=0.54), LOA (1.23 ± 1.10 vs 1.24 ± 0.93, p=0.89) and HOA (0.67 ± 0.41 vs 0.64 ± 0.32, p=0.77). Corneal asphericity did not change (p=0.72).
The epithelial thickness profiles before and after surgery are shown in Figures 1 and 2, respectively. The respective differences in each area are shown in Table 2. ET was higher in the inferior areas in both pre and postoperatively. Mean epithelial thickness was lower before surgery in both paracentral (45.1 ± 1.2 µm versus 47.8 ± 1.4 µm, p<0.01) and mid-peripheral (41.5 ± 1.6 µm versus 44.7 ± 1.2, p<0.01) in superior area. ET was also lower before surgery at ST (p<0.001) and SN (p<0.001) in both paracentral and midperipheral areas. The difference between inferior and superior meridians was greater after surgery (7 µm versus 3 µm, p<0.001). The minimum ET in the midperipheral area was lower before surgery (41.6 ± 1.9 µm versus 42.9 ± 2.3, p=0.03) and was found in the superior area. The mean (p=0.61) and maximum ET (p=0.77) did not change.
 |
Table 2 Corneal Epithelial Thickness Comparison (Mean ± Standard Deviation, Range, µm), Between Baseline and After Blepharoplasty |
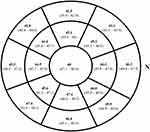 |
Figure 1 Epithelial thickness (mean, range, µm) mapping at the baseline. Abbreviation: N, Nasal. |
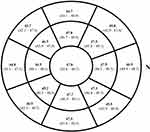 |
Figure 2 Epithelial thickness (mean, range, µm) mapping on the 8th postoperative week. Abbreviation: N, Nasal. |
Discussion
The present study shows that remodeling of the corneal epithelium occurs eight weeks after upper eyelid blepharoplasty: The superior epithelium thickens in both the paracentral and midperipheral areas. Moreover, the steepest keratometry and the corresponding axis changed with a tendency toward the vertical meridian.
The corneal epithelium is a highly active layer. Alfred Vogt was the first to describe, in 1921, the ability of the epithelium to change its thickness to compensate for stromal irregularities and maintain a smooth surface.11 In corneas without pathology, the epithelium is thinner in superior areas. Dan Reinstein was the one who better explained this finding as an effect of eyelid force over superior epithelium during blinking.2 In our opinion, including patients with dermatochalasis before and after upper eyelid blepharoplasty who have normal tomographic corneas may better illustrate the effect of the upper eyelid on the corneal epithelium. We prefer to evaluate the patients 8 weeks after surgery because it was the average time for resolution of rigid gas-permeable contact-lens corneal warpage and may be the best timing to have the epithelium re-established.12
Upper blepharoplasty is the treatment of choice for dermatochalasis and is one of the most commonly performed procedures in ophthalmology.13 It typically weakens the upper eyelid structures and its effect on the ocular surface.4–6 Previous studies have shown that upper eyelid blepharoplasty could change corneal topography, but none have studied its effect on the ET profile.3,5,9
Anterior segment optical coherence tomography (AS-OCT) provides high resolution images of the corneal epithelium without the need for contact as with the gold-standard very high-frequency ultrasound.
Although previous studies have found the same ET profile,14,15 we found statistically significant differences after surgery in the ET profile.14,15 The superior epithelium thickened eight weeks after upper eyelid blepharoplasty and the difference between inferior and superior areas (I-S) was lower, which may reflect the effect of the upper eyelid on the superior epithelium and confirm Reinstein’s theory.
Previous studies have found differences in corneal tomography data in patients with dermatochalasis who underwent upper eyelid blepharoplasty.16,17 Ekin et al found an average change of 0.22D and Brown et al found up to 0.57D. In our study, the steepest keratometry and the degree of astigmatism decreased after surgery, which is consistent with previous studies. The mean difference between the preoperative and postoperative astigmatism was lower than other groups (0.12D) but could only reflect a less invasive technique from our team. In fact, Zinkernagel et al found differences in astigmatism changes when fat was removed or not and we do not routinely remove it.
We also found a change in the astigmatism axis with a tendency towards with-the-rule astigmatism. These findings, together with epithelial thickness analyses, lead us to suggest that dermatochalasis may exert more pressure on the superior epithelium, which in turn contributes to against-the-rule astigmatism.
In this study, we found no differences in corneal aberrations. Although Ekin et al and Kim et al found a reduction in HOA after surgery, we do not expect this because we had strict inclusion criteria based on the tomographic data. The cut-off value of 1.22 for BAD-D increases the specificity to select corneas without ectasia, even fruste forms.
Our study has some limitations, particularly the small sample and device-related limitations. Cirrus OCT measures ET 5–6 µm thinner than the other devices. Rather than considering absolute thickness values as accurate, the main findings of this study relate to the change in epithelial thickness due to upper eyelid blepharoplasty, so these differences can be applied to epithelial measurements with other devices.
Nevertheless, our study clearly illustrates the change in epithelial thickness profile after blepharoplasty in patients with dermatochalasis and supports the theory that upper eyelid pressure has an impact ocular surface. Our results also lead us to consider whether patients considering crystalline lens exchange (CLE), particularly those who will have a toric lens implanted, should be evaluated by an oculoplastic surgeon prior to phacoemulsification, as the profiles of patients seeking CLE and blepharoplasty often overlap.
Conclusion
Optical coherence tomography analysis shows that upper eyelid blepharoplasty affects the corneal epithelial thickness profile and may alter corneal steepest axis. This procedure should be considered before cataract surgery in patients with dermatochalasis, in particular, those who are considered for toric intraocular lens implantation.
Confidentiality of Data
The authors declare that they have followed the protocols of their work center on the publication of data from patients.
Funding
This work has not received any contribution, grant or scholarship.
Disclosure
The authors have no financial or proprietary interest in the materials presented herein.
References
1. Reinstein DZ, Archer TJ, Gobbe M. Corneal epithelial thickness profile in the diagnosis of keratoconus. J Refract Surg. 2009;25(7):604–610. doi:10.3928/1081597X-20090610-06
2. Reinstein DZ, Archer TJ, Vida RS. Applications of epithelial thickness mapping in corneal refractive surgery. Saudi J Ophthalmol. 2022;36(1):25–35. doi:10.4103/sjopt.sjopt_227_21
3. Floegel I, Horwath-Winter J, Muellner K, Haller-Schober E-M. A conservative blepharoplasty may be a means of alleviating dry eye symptoms. Acta Ophthalmologica Scandinavica. 2003;81(3):230–232. doi:10.1034/j.1600-0420.2003.00064.x
4. Simsek IB, Yilmaz B, Yildiz S, Artunay O. Effect of upper eyelid blepharoplasty on vision and corneal tomographic changes measured by pentacam. Orbit. 2015;34(5):263–267. doi:10.3109/01676830.2015.1057292
5. Hahn S, Holds JB, Couch SM. Upper Lid Blepharoplasty. Facial Plast Surg Clin North Am. 2016;24(2):119–127. doi:10.1016/j.fsc.2016.01.002
6. Brown MS, Siegel Irwin M, Lisman RD. Prospective analysis of changes in corneal topography after upper eyelid surgery. Ophthal Plast Recont Surg. 1999;15:1
7. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocular Sur. 2017;15(3):276–283. doi:10.1016/j.jtos.2017.05.008
8. Ambrósio R, Ramos I, Lopes B, et al. Assessing ectasia susceptibility prior to LASIK: the role of age and residual stromal bed (RSB) in conjunction to Belin-Ambrósio deviation index (BAD-D). Rev Bras Oftalmol. 2014;73(2):75–80. doi:10.5935/0034-7280.20140018
9. Paryani MJ, Kharbanda V, Kummelil MK, Wadia K, Darak AB. Pupillodynamics and corneal spherical aberrations in a set of Indian cataract patients and its implications for aberrometric customisation of intraocular lenses. Indian J Ophthalmol. 2020;68(12):3012–3015. doi:10.4103/ijo.IJO_218_20
10. Loureiro TD, Rodrigues-Barros S, Lopes D, et al. Corneal epithelial thickness profile in healthy Portuguese children by high-definition optical coherence tomography. Clinical Ophthalmol. 2021;15:735–743. doi:10.2147/OPTH.S293695
11. Hwang ES, Schallhorn JM, Randleman JB. Utility of regional epithelial thickness measurements in corneal evaluations. Sur Ophthalmol. 2020;65(2):187–204. doi:10.1016/j.survophthal.2019.09.003
12. Wang X, McCulley JP, Bowman RW, Cavanagh HD. Contact lens-induced corneal warpage in patients scheduled for photorefractive surgery. Invest Ophthalmol Vis Sci. 2002;43:3103
13. Yang P, Ko AC, Kikkawa DO, Korn BS. Upper eyelid blepharoplasty: evaluation, treatment, and complication minimization. Semin Plast Surg. 2017;31(01):51–57. doi:10.1055/s-0037-1598628
14. Reinstein DZ, Archer TJ, Gobbe M, Silverman RH, Coleman DJ. Epithelial thickness in the normal cornea: three-dimensional display with very high frequency ultrasound. J Refract Surg. 2008;24:571.
15. Abusamak M. Corneal epithelial mapping characteristics in normal eyes using anterior segment spectral domain optical coherence tomography. Transl Vis Sci Technol. 2022;11(3):6. doi:10.1167/tvst.11.3.6
16. Sommer F, Untch E, Spoerl E, et al. Effect of upper eyelid blepharoplasty on corneal biomechanical, topographic and tomographic parameters 4 weeks after surgery. Int Ophthalmol. 2022;42:113–121. doi:10.1007/s10792-021-02006-6
17. Altin Ekin M, Karadeniz Ugurlu S. Prospective analysis of visual function changes in patients with dermatochalasis after upper eyelid blepharoplasty. Eur J Ophthalmol. 2020;30(5):978–984. doi:10.1177/1120672119857501
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
