Back to Journals » Clinical Epidemiology » Volume 14
The Effect of Prucalopride on the Completion Rate and Polyp Detection Rate of Colon Capsule Endoscopies
Authors Deding U , Kaalby L , Baatrup G , Kobaek-Larsen M, Thygesen MK , Epstein O , Bjørsum-Meyer T
Received 16 December 2021
Accepted for publication 12 March 2022
Published 2 April 2022 Volume 2022:14 Pages 437—444
DOI https://doi.org/10.2147/CLEP.S353527
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Vera Ehrenstein
Ulrik Deding,1,2 Lasse Kaalby,1,2 Gunnar Baatrup,1,2 Morten Kobaek-Larsen,1,2 Marianne Kirstine Thygesen,1,2 Owen Epstein,3 Thomas Bjørsum-Meyer1,2
1Department of Surgery, Odense University Hospital, Svendborg, Denmark; 2Department of Clinical Research, University of Southern Denmark, Odense, Denmark; 3Institute for Minimally Invasive Gastroenterology, Royal Free London NHS Foundation Trust, London, UK
Correspondence: Ulrik Deding, Department of Surgery, Odense University Hospital, Baagøes Allé 15, SVB Bygning 13.02, Svendborg, 5700, Denmark, Tel +45 42574243, Email [email protected]; [email protected]
Purpose: To investigate whether the prokinetic prucalopride increases the completion rate of colon capsule endoscopy (CCE). Secondary outcomes included demographic distribution, polyp detection rate (PDR), distribution of Leighton–Rex grade, and adverse events.
Patients and Methods: In a nested cohort within the CareForColon2015 trial, a subgroup of 406 individuals underwent CCE in 2021. The first half (control) received the standard bowel preparation and the second half (prucalopride) was supplemented with 2 mg of prucalopride. Transit times and bowel preparations were analyzed and completion rates calculated as those having timely transit and acceptable bowel cleanliness. Major adverse events were recorded continuously and minor adverse events were quantified from questionnaires.
Results: The group demographics were homogenous. The prevalence ratio for complete CCE was 1.32 (CI 95% 1.15; 1.53) in the prucalopride group compared to the control group. Completion rate was 74.9% in the prucalopride group and 56.7% in the control group. The proportions of acceptable bowel preparation and complete transits were higher in the prucalopride group. The mean CCE transit time was 2 hours and 8 minutes faster in the prucalopride group. The PDR was higher in the intervention group with 55.7% compared to 36.0% in the control group for polyps greater than 9 mm, whereas the groups’ PDRs were similar for small and diminutive polyps. In all, 589 polyps (mean 2.9) were found in the prucalopride group compared to 522 polyps (mean 2.6) in the control group.
Conclusion: Prucalopride led to an increase in CCE completion rates. The proportions of complete transits and acceptable bowel preparations were higher in the prucalopride group. The PDR was higher in the prucalopride group compared to the control group. No major adverse events were identified. Nausea, diarrhea, headache and fatigue were more commonly reported in the prucalopride group.
Keywords: Resolor, prokinetic, polyps, bowel preparation, Leighton–Rex, video capsule endoscopy
Introduction
The use of colon capsule endoscopy (CCE) to detect colorectal polyps has been reported in numerous studies.1–6 In complete CCE investigations, polyp detection rates (PDR) for large polyps and complications appear to be equivalent or better than those reported from conventional optical colonoscopy.1,7,8 One of the drawbacks in CCE is the high proportion of incomplete examinations9 leading to patients needing additional investigations. Incomplete CCE investigations can be caused by inadequate bowel cleansing or a transit time exceeding the battery lifetime.
We have been evaluating CCE in the Danish National Colorectal Cancer screening program in an ongoing trial (CareForColon2015) launched in 2020.10 The interim analysis from this trial was published in the summer of 2021, revealing a CCE completion rate of 67.9%, which was lower than expected.7 This elicited an examination of how to improve the completion rate by adjusting the bowel preparation regimen.10 Adding prucalopride (Resolor®) to the regimen prior to capsule ingestion seemed a logical adjustment. Prucalopride is a serotonin receptor antagonist that accelerates colonic transit time by increasing peristaltic activity.11 This prokinetic has been reported to decrease transit time in patients undergoing small bowel capsule endoscopy.12
The aim of this study was to determine whether the introduction of prucalopride significantly increases the completion rate of CCE compared to the standard bowel preparation without decreasing the PDR and increasing the number of adverse events.
Materials and Methods
CareForColon2015 is an ongoing randomized controlled trial nested in the Danish Colorectal Cancer Screening Program. The control group undergoes fecal immunochemical test (FIT) followed by colonoscopy if positive. The intervention group is offered the choice of CCE or colonoscopy if the FIT is positive (For details, see protocol10). Prucalopride was added to the bowel preparation regimen nine months after trial launch and we conducted this interim analysis after 203 individuals had undergone the new regimen. They were compared to the last 203 individuals undergoing CCE with the standard bowel preparation. The standard bowel preparation is defined in Table 1. Individuals were invited for the trial in a random order. The current study is a nested cohort within the CareForColon2015 trial.
 |
Table 1 Bowel Preparation Regimens |
Outcomes
The main outcome of the study was the completion rate of CCE. Secondary outcomes included conclusive investigation rate, bowel preparation quality, transit time, PDR, adverse events and demographic distribution.
A CCE investigation was defined as complete when the hemorrhoidal plexus had been visualized by the capsule while bowel preparation was rated fair or better on the Leighton–Rex scale13 for all colonic segments (cecum, right, transverse, left and rectum).
Conclusive investigation rate was defined as investigations that were complete or had positive findings resulting in referral for colonoscopy, ie a) one polyp larger than nine mm or b) more than two polyps of any size. The proportions of Leighton–Rex grades for each colonic segment was used to describe the quality of the bowel preparations. The transit time was defined as the total time in minutes from capsule ingestion until excretion or visualization of hemorrhoidal plexus, ie the transit time of the entire GI tract. The PDR was defined as the proportion of individuals with at least one polyp. PDR was stratified as follows: 1) polyps of any size, 2) at least one polyp greater than 5 mm and 3) at least one polyp greater than nine mm. Total number and mean number of polyps per individual was derived for each group. Demographics included age and sex. Adverse events were described using self-reported data from the participants. An electronic questionnaire distributed three days after CCE registered adverse events during bowel preparation, CCE and the three days thereafter. Minor adverse events recorded from these questionnaires included bloating, abdominal pain, minor or moderate rectal bleeding and free text to describe other adverse events. The nurses and doctors on call would record major adverse events continuously.
Colon Capsule Endoscopy
The colon capsule endoscopies (PillCamTM COLON 2 capsules (Medtronic, Massachusetts, MA, US)) were delivered by an external private contractor, who delivered the capsules in four locations in the Region of Southern Denmark. The bowel cleansing regimen was initiated at home and on the day of CCE, a 2 mg prucalopride tablet was administered to the patients by the nurses, thereby ensuring compliance. Following capsule ingestion, participants left the facility, but stayed in contact with the nurses by phone for each CCE signal. The following day, participants returned the CCE receiver. The videos were uploaded to a cloud-based platform from which experienced readers could access and analyze the videos. At the time of reporting the videos, readers were unaware of the change in the study regimen. The readers uploaded a report describing bowel cleanliness for each segment as well as pictures and timestamps of each polyp, colonic landmarks and the hemorrhoidal plexus. This report was then reviewed by a doctor responsible for directing the patient’s ongoing clinical journey. The CCE outcome data for this study was extracted from these reports.
Power
Power calculations were performed prior to the study launch. Based on a previous interim analysis we expected a 67.9% completion rate in the control group. The expected completion rate of the prucalopride group had been set at 80%. With a significance level of 0.05 and detection power of 0.8, an increase from 67.9% to 80.0% would require a minimum of 203 individuals in each group. The study sample was therefore determined to be 406 individuals.
Statistical Analysis
The control and prucalopride groups were compared for demographic characteristics, as well as CCE outcomes and adverse events. A multivariate log binomial regression model was performed in order to determine the prevalence ratio of complete CCE investigation in the prucalopride group compared to the control group adjusted for sex and age. Data management and statistical analysis was conducted in SAS 9.4 (SAS, Cary, North Carolina).
Ethics
The randomized controlled trial was approved by the Southern Denmark Regional Health Research Ethics Committee (ID S-20190100). Following the interim analysis from the trial, an additional approval from the Committee was obtained in order to change the bowel preparation procedure (ID S-20190100, addition 78592). The current study was a nested cohort within the randomized clinical trial conducted as an interim following the ethical approval of the change in bowel preparation. All participants received oral and written information and signed informed consent forms prior to participation. All data is stored in accordance with both the General Data Protection Regulation and Danish law on data handling and security. The trial was registered with ClinicalTrials.gov (NCT04049357) and approved by the Danish data protection agency by registration in the Regional records of handling personal information in research (journal no. 19/29,858) prior to patient enrollment. The study was conducted in accordance with the Declaration of Helsinki.
Results
Between February 24 and July 27, 2021, 406 individuals underwent CCE. The first prucalopride tablet was administered on May 10, 2021. Prior to this period, 478 individuals had undergone CCE in the clinical trial. The two groups expressed similar demographic distributions. The female proportions were 48.8% in the control group and 47.3% in the prucalopride group. Mean age was 62.3 years in both groups (Table 2).
 |
Table 2 Group Comparison |
CCE completion rates were higher in the prucalopride group with 74.9% complete investigations compared to 56.7% in the control group. Bowel preparation quality was acceptable in 75.9% of the prucalopride group and better than the 57.1% reported in the control group. Conclusive investigation rates were also higher in the prucalopride group at 89.7%, compared to 75.4% in the control group. The proportion of CCE with complete transit was higher at 95.1% in the prucalopride group compared to 88.2% in the control group. Average CCE transit time was 2 hours and 8 minutes faster in the prucalopride group, ie 5h 38min and 3h 30min. The PDR for polyps any size were similar in the control and prucalopride groups (80.3% and 78.8%) and for polyps greater than 5 mm, (64.5% and 72.9%). The PDR for polyps greater than nine mm was higher in the prucalopride group (36% and 55.7%) (Table 3). The total polyp count was higher in the prucalopride group with 589 polyps compared to 522 in the control group. The mean polyp count per individual was similar in both the prucalopride and control groups (2.6 and 2.9).
 |
Table 3 Colon Capsule Endoscopy Outcomes |
The bowel preparation grade followed a trend for all segments where the majority of investigations had a fair or good preparation. For all five colonic segments, the proportion of unacceptable bowel preparation was higher in the control group, especially in the cecum and the rectum (Table 4). The prevalence ratio for complete examination was 1.32 (CI 95% 1.15; 1.53) in the prucalopride group compared to the control group, while it did not differ based on age or gender (Table 5).
 |
Table 4 Leighton–Rex Bowel Preparation Grade Proportions per Colonic Segment |
 |
Table 5 Multivariate Log Binomial Regression Model Estimating the Prevalence Ratio for Complete Colon Capsule Endoscopy |
Adverse Events
We recorded no major adverse events in either of the groups. Due to a technical error in the distribution of electronic questionnaires, 31 participants in the control group did not receive a questionnaire. There were seven non-responders in each group. Therefore, 165 individuals from the control group and 196 from the prucalopride group responded to the electronic questionnaire. This gave a response rate of 95.9% in the control group and 96.6% in the prucalopride group. There was no differences for adverse events in the predefined categories of bloating, abdominal pain and minor or moderate rectal bleeding between the two groups. From the free text entries, more patients reported nausea, diarrhea, headache and fatigue in the prucalopride group (Table 6).
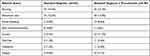 |
Table 6 Self-Reported Minor Adverse Events |
In addition to the more commonly reported adverse events (Table 6), there were additional reports. In the control group, one participant reported fluid retention, one reported a hemorrhoid, one worsening of a preexisting condition, three felt anxious, one reported elevated heart rate and two felt a change in body temperature. In the prucalopride group, one participant reported worsening of a preexisting condition, one felt anxious, two felt an affected body temperature and three felt dizzy. Some participants in both groups also reported hunger or distaste for the sulfate-based solution.
Discussion
In this study, we sought to investigate the effect of a single prucalopride tablet on CCE completion rate. The trial indicated that adding a single 2 mg dose of prucalopride to the bowel cleansing regimen increased the completion rates by inducing an increase in both capsule transit times and bowel cleanliness. The rate of conclusive investigations was 89.7%. The PDR was higher in the prucalopride group, although only for polyps over 9 mm. The explanation why the PDR was limited remains unknown, but the group demographics did not suggest any selection problems. The prucalopride group reported more minor adverse events (nausea, diarrhea, headache and fatigue). Adequate bowel cleanliness is of uttermost importance because cancer and polyp miss rates are increased with inadequate visualization of the colonic mucosa.14
We observed improved rates of acceptable bowel preparation and complete capsule transit to 76% and 95%, respectively, with the addition of prucalopride to the regimen. According to international guidelines for flexible colonoscopy, rates of adequate cleanliness and complete examination should reach 90% as a minimum standard.15 The same standards should be applied to CCE. In a recent meta-analysis, most studies on CCE failed to comply with recommendations with an overall adequate bowel cleanliness and completion rate of 77% and 80%, respectively.16
In a pilot study, Hookey et al assessed the efficacy of two CCE booster regimens. Their regimen included a 4 mg prucalopride booster compared to a booster regimen with a sodium picosulfate + magnesium citrate. This intervention failed to improve the quality of CCE.17 The study was small with mixed indications for colonic imaging and included only 13 patients in the prucalopride booster group. Alsahafi et al reported a significantly shorter small bowel transit time in hospitalized patients receiving prucalopride before small bowel capsule endoscopy.18 They did not report a significant effect on completion rate.
There were no major adverse events reported in our trial. This is consistent with the findings of a recent meta-analysis.19 The low risk of severe complications is one of the advantages of CCE compared to colonoscopy. There were minor adverse events in the prucalopride group and future studies might consider a lower dose of prucalopride, combination with an antiemetic, or use of a booster other than the sulfate-based solution.
This study has inherent weaknesses. As this was not a randomized trial, there was no concurrent control group but it is unlikely that increased completion rates occurred by chance. The completion rate of the control group was low and the reason for this is unknown. The participants completed the bowel preparation as well as booster regimen in their own homes. No professional evaluation of the compliance could therefore be made, but for it to bias the improvement, the compliance would need to differ between groups.
This is the first large sample trial to address the potential advantage of adding the prokinetic prucalopride to a bowel preparation regimen for video colon capsule imaging. The sample size was based on a power calculation performed prior to the study and we observed an even higher effect on completion rate than expected. Completion rates in the control group were surprisingly low and below earlier reports of the regimen. Investigations are underway to explore underlying causes for this.
Conclusion
In this trial, the addition of 2 mg prucalopride increased the CCE completion rate. The proportion of individuals with a complete CCE in patients who received prucalopride in the bowel preparation regimen were 1.32 fold that of those receiving our standard bowel preparation. Completion rate of CCE was 74.9% in the prucalopride group compared to 56.7% in the control group. Both proportion of complete transits within battery lifetime of the capsule, and the proportion of acceptable bowel preparations were higher in the prucalopride group. The PDR were equal to or higher in the prucalopride group compared with the control group. No major adverse events were identified in either group. Nausea, diarrhea, headache and fatigue were more common in the prucalopride group. Therefore, it seems evident that prucalopride can increase completion rates without affecting the quality of CCE, although there does appear to be a slight increase in minor side effects. The results of this study recommends future investigation to determine dose response and the interaction of prucalopride with other bowel cleansing and booster regimens.
Data Sharing Statement
The data analysed in the current study will not be made publicly available, as it is an interim analysis of an ongoing clinical trial (ClinicalTrials.gov NCT04049357) that have not yet finalized inclusion.
Funding
The clinical trial was funded by Odense University Hospital’s innovation fund (grant R75-A3392), Aage and Johanne Louis-Hansen’s Fond (grant 17–2B-1409), the Danish Cancer Society (grant R100-A6747), Medtronic Research Foundation (grant ERP 2018–11151), and the Excellence Centre in the Region of Southern Denmark (grant 18/48426). Medtronic VR (Minneapolis, Minnesota, United States) provided the capsules, but had no influence on study protocol, analysis, or interpretation of the results.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kobaek-Larsen M, Kroijer R, Dyrvig AK, et al. Back-to-back colon capsule endoscopy and optical colonoscopy in colorectal cancer screening individuals. Colorectal Dis. 2018;20(6):479–485. doi:10.1111/codi.13965
2. Deding U, Herp J, Havshoei AL, et al. Colon capsule endoscopy versus CT colonography after incomplete colonoscopy. Application of artificial intelligence algorithms to identify complete colonic investigations. United Eur Gastroenterol J. 2020;8(7):782–789. doi:10.1177/2050640620937593
3. Hussey M, Holleran G, Stack R, Moran N, Tersaruolo C, McNamara D. Same-day colon capsule endoscopy is a viable means to assess unexplored colonic segments after incomplete colonoscopy in selected patients. United Eur Gastroenterol J. 2018;6(10):1556–1562. doi:10.1177/2050640618800629
4. Baltes P, Bota M, Albert J, et al. PillCamColon2 after incomplete colonoscopy - A prospective multicenter study. World J Gastroenterol. 2018;24(31):3556–3566. doi:10.3748/wjg.v24.i31.3556
5. Spada C, De Vincentis F, Cesaro P, et al. Accuracy and safety of second-generation PillCam COLON capsule for colorectal polyp detection. Therap Adv Gastroenterol. 2012;5(3):173–178. doi:10.1177/1756283X12438054
6. Spada C, Pasha SF, Gross SA, et al. Accuracy of first- and second-generation colon capsules in endoscopic detection of colorectal polyps: a systematic review and meta-analysis. Clinical Gastroenterol Hepatol. 2016;14(11):1533–1543.e1538. doi:10.1016/j.cgh.2016.04.038
7. Deding U, Bjørsum-Meyer T, Kaalby L, et al. Colon capsule endoscopy in colorectal cancer screening: interim analyses of randomised controlled trial CareForColon2015. Endoscopy International Open. 2021;13(13):2302–2304.
8. Spada C, Hassan C, Munoz-Navas M, et al. Second-generation colon capsule endoscopy compared with colonoscopy. Gastrointest Endosc. 2011;74(3):581–589. doi:10.1016/j.gie.2011.03.1125
9. Deding U, Kaalby L, Bøggild H, et al. Colon capsule endoscopy vs. CT colonography following incomplete colonoscopy: a systematic review with meta-analysis. Cancers. 2020;12(11):11. doi:10.3390/cancers12113367
10. Kaalby L, Deding U, Kobaek-Larsen M, et al. Colon capsule endoscopy in colorectal cancer screening: a randomised controlled trial. BMJ Open Gastroenterol. 2020;7(1):e000411. doi:10.1136/bmjgast-2020-000411
11. Sepe A, Grossi L, Ciccaglione AF, et al. Tu1148 role of prucalopride (Resolor®) in the setting-up of PillCam Colon-Capsule Endoscopy (CCE). Experience from a single centre. Gastroenterology. 2014;146(5):S766–S766. doi:10.1016/S0016-5085(14)62769-4
12. Sepe A, Vecchione V, Di Berardino M, et al. Prucalopride accelerates gastric and small bowel transit times of videocapsule endoscopy. Gastroenterology. 2017;152(5):S1033–S1034. doi:10.1016/S0016-5085(17)33493-5
13. Leighton JA, Rex DK. A grading scale to evaluate colon cleansing for the PillCam COLON capsule: a reliability study. Endoscopy. 2011;43(2):123–127. doi:10.1055/s-0030-1255916
14. Zhao S, Wang S, Pan P, et al. Magnitude, risk factors, and factors associated with adenoma miss rate of tandem colonoscopy: a systematic review and meta-analysis. Gastroenterology. 2019;156(6):1661–1674.e1611. doi:10.1053/j.gastro.2019.01.260
15. Kaminski MF, Thomas-Gibson S, Bugajski M, et al. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy. 2017;49(4):378–397. doi:10.1055/s-0043-103411
16. Bjørsum-Meyer T, Skonieczna-Zydecka K, Cortegoso Valdivia P, et al. Efficacy of bowel preparation regimens for colon capsule endoscopy: a systematic review and meta-analysis. Endoscopy International Open. 2021;9:E1–E16.
17. Hookey L, Kelley M, Marchut K, Green J, Bechara R. Colon capsule visualization is not enhanced with prucalopride: a randomized controlled trial. J Can Assoc Gastroenterol. 2018;1(1):20–25. doi:10.1093/jcag/gwy005
18. Alsahafi M, Cramer P, Chatur N, Donnellan F. The effect of prucalopride on small bowel transit time in hospitalized patients undergoing capsule endoscopy. Can J Gastroenterol Hepatol. 2017;2017:2696947. doi:10.1155/2017/2696947
19. Deding U, Cortegoso Valdivia P, Koulaouzidis A, et al. Patient-reported outcomes and preferences for colon capsule endoscopy and colonoscopy: a systematic review with meta-analysis. Diagnostics. 2021;11(9):1730. doi:10.3390/diagnostics11091730
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
