Back to Journals » Orthopedic Research and Reviews » Volume 14
The Effect of Platelet-Rich Plasma on Type I Collagen Production, VEGF Expression, and Neovascularization after Femoral Bone Implants: A Study on Rat Models
Authors Rahman S, Sutedja E, Ayu O, Amirsyah M
Received 25 January 2022
Accepted for publication 31 May 2022
Published 13 June 2022 Volume 2022:14 Pages 207—214
DOI https://doi.org/10.2147/ORR.S359844
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Safrizal Rahman,1,2 Endang Sutedja,3 Onarisa Ayu,1,2 Mirnasari Amirsyah4,5
1Division of Orthopedics and Traumatology, Department of Surgery, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia; 2Division of Orthopedics and Traumatology, Department of Surgery, School of Medicine, Dr. Zainoel Abidin Hospital, Banda Aceh, Indonesia; 3Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia; 4Division of Plastic and Reconstruction Surgery, Department of Surgery, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia; 5Division of Plastic and Reconstruction Surgery, Department of Surgery, School of Medicine, Dr Zainoel Abidin Hospital, Banda Aceh, Indonesia
Correspondence: Safrizal Rahman, Division of Orthopedics and Traumatology, Department of Surgery, School of Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia, Email [email protected]
Introduction: Platelet-rich plasma (PRP) contains many growth factors, such as FGF, which induces the production of type I collagen, and VEGF, which induces neovascularization, all of which are important in bone healing. This study aimed to evaluate the effect of PRP administration on type I collagen production, VEGF expression, and neovascularization in rat models following femoral bone implants using K-wire.
Methods: An experimental randomized control study was conducted on 24 white male rats (Rattus norvegicus) in the Wistar strain that underwent K-wire implantation, where PRP was administered to the treatment groups. The amount of type I collagen was measured by immunohistochemistry VEGF expression using sandwich ELISA, and neovascularization by histopathological examination.
Results: The amount of type I collagen in the treatment group (50–> 150/field of view) was significantly higher than the control group (0– 99/field of view; p=0.003). VEGF expression in the treatment groups was significantly higher than controls: 10.90± 4.47 and 2.29± 0.92, respectively (p=0.006). Mean number of new vessels formed on fibrotic capsules in the treatment groups was significantly (p=0.007) higher than the control groups (2.69± 1.03 vs 0.67± 0.52).
Conclusion: The use of PRP significantly increased type I collagen production, VEGF expression, and neovascularization in rat models, elucidating the potential of PRP to be used in clinical settings to enhance the bone-healing process.
Keywords: platelet-rich plasma, vascular endothelial growth factor, type I collagen, neovascularization, bone healing, orthopedic implants
Introduction
The use of orthopedic implants, such as artificial joints, intramedullary rods, plates, and screws, has increased rapidly within the last few years. However, the implants used can cause complications, such as scars, infection, and necrosis.1–3 Physiologically, the presence of a foreign body induces inflammatory responses and the wound-healing process and results in the formation of a thick fibrotic capsule around the implants.4,5 The capsule, sometimes referred to as the foreign-body capsule, acts as a biological and structural barrier between the tissue and the implant.4,6,7 In general, this capsule lacks vascularization, and may cause such complications as inflammation, infection, and tissue necrosis, which may lead to implant failure or rejection.5,6,8 Conversely, adequate vascularization around an implant is positively associated with increased bone growth and decreased incidence of infection and implant failure.7,9
Platelet-rich plasma (PRP) is a concentrated platelet product which has five- to ninefold the concentration of platelets of circulating platelet counts.10–12 Investigations on rats support the use of PRP in human clinical settings.11,13,14 Oryan et al14 found that PRP promoted bone healing (microscopic union) better than a control group (p=0.001). PRP contains growth factors that are important in the healing process, such as CTGF, PDGF, TGFβ, FGF, VEGF, and EGF.15–17 It also contains inflammation mediators, such as macrophages, monocyte mediators, and interleukins,10,11,18 as well as important proteins like fibrinogen, albumin, and immunoglobulin,10,19 which are important in bone healing and remodeling.
FGF in PRP induces fibroblast formation, which produces collagen, especially type I collagen.16,18 Collagen is the most abundant protein in the human body, making up to a third of the total protein mass. Among the 28 types of collagen, type I collagen is the most abundant and is usually found in connective tissue, such as skin, bone, and tendons.20 Studies have shown that administration of type I collagen on implant surfaces was positively associated with neovascularization formation on fibrotic capsules.20–22 This shows the potential of type I collagen in quickening the bone-healing process following implant insertion.
VEGF is a proangiogenic substance expressed by macrophages, tumor cells, and osteoblasts that plays an important role in angiogenesis by regulating vascular endothelial cell proliferation, vascular permeability, and antiapoptosis on newly formed vascular endothelial cells.23–25 Release of VEGF enhances bone regeneration and neovascularization.26,27 An in vitro study showed that inhibition of VEGF suppressed vascular invasion and bone formation.28 The administration of VEGF on silicon implants also decreases fibrotic capsule thickness and increased vascularization around implants in rat models.29 Moreover, treatment with exogenous VEGF increases vascularity and mineral density in mouse femur-fracture models.30 Nevertheless, the consequences of exogenous VEGF administration on bone healing might vary to a certain extent.24 Excess VEGF might recruit excess osteoclasts, resulting in resorption and not providing the opportunity for maturation of newly formed bone.31,32 Excess VEGF also inhibits the function of pericytes through PDGF-receptor inhibition, leading to interrupted angiogenesis–osteogenesis coupling and immature blood-vessel formation.33 Moreover, artificial and exogenous VEGF might require further synthetic or rat proteins as carriers and cause rejection.34
Unlike artificial and exogenous growth factors, PRP can serve as a natural carrier, resulting in a lower risk of rejection.13 Moreover, as it is usually drawn from patients’ own blood, PRP is cheaper and easier to prepare.15 This study aimed to evaluate the effect of PRP administration on type I collagen production, VEGF expression, and neovascularization on fibrotic capsules in rat models following femoral bone–implant insertion.
Methods
This was an experimental randomized control study on rat models to examine the effect of PRP on type I collagen production, VEGF expression, and neovascularization on fibrotic capsules after femoral bone–implant surgery (insertion using K-wire). Ethics approval was obtained from the Faculty of Veterinary Medicine, Universitas Syiah Kuala, Aceh, Indonesia (004/KEPH-C/III/2015). The experiment was done in accordance with Universitas Syiah Kuala’s guidelines on laboratory care and use of laboratory rats.
Experimental Rats and Housing
A total of 24 male Wistar strain white rats (Rattus norvegicus) aged 12–16 weeks weighing 200–300 g were obtained from the Pharmacology Laboratory, Faculty of Veterinary Medicine, Universitas Syiah Kuala, Banda Aceh, Indonesia, where all procedures were carried out. Seven days prior to the study, the rats went through an acclimation process under laboratory conditions (70%–80% humidity, temperature around 20°C–25°C, and adequate lighting) were fed and given water ad libitum. They were kept in clean cages, and the husks were replaced every day. After 7 days of acclimation, the rats underwent surgical procedures and were divided into four groups of six: two treatment groups (T1 and T2) with K-wire implant installation on the lateral side of the femur bone with PRP administration, and two control groups (C1 and C2) with K-wire implant installation on the lateral side of the femur bone without PRP administration. One treatment group (T1) and one control group (C1) were culled on the seventh day after surgery to be examined for the amount of type I collagen. The T2 and C2 groups were culled on the 21st day postsurgery to be examined for VEGF expression and vascularization formation around fibrous encapsulations.
Preparation of PRP
Peripheral blood samples were collected from study rats, stored in a tube with anticoagulant (citrate–phosphate dextrose), and then centrifuged at 20°C at 2,400 rpm for 10 minutes. The supernatant (plasma) formed, the buffy-coat layer, and 0.5 mL below the buffy-coat layer were separated into another tube and recentrifuged at 20°C at 3,600 rpm for another 10 minutes. The supernatant formed was then separated, while the buffy-coat layer and 0.5 mL below it was collected as the PRP and stored at −80°C.16 PRP was sprayed on the surface of the prepared K-wire implant.
Surgical Procedures
K-wire implantation comprised an incision in the lateral femoral region (femur), splitting the vastus lateralis muscle, and performing a 1.5 cm–long K-wire insertion on the lateral side of the femur (Figure 1). The PRP (around 3–5 cm3) was dripped on the surface of the wire in the treatment groups. The wound was closed by thoroughly stitching the muscles and the skin. Antibiotic and painkiller injections were later given to each rat.
 |
Figure 1 K-wire implantation in femoral bone. |
Assessment of Type I Collagen
Immunohistochemistry (IHC) examination was conducted based on the avidin–biotin complex.39 The amount of type I collagen produced in both groups was examined using the IHC method and type I collagen monoclonal antibodies. Measurement of type I collagen production was done by counting the number of cells found in every 1.000 immunoreactive cells. The assessment was carried out at the Integrated Research Laboratory, Faculty of Veterinary, Universitas Syiah Kuala, Aceh, Indonesia.
The results of IHC examination of type I collagen expression were explicated using a histoscore, calculated as the product of the intensity and distribution. The color intensity was 0 for negative (yellow), 1 for weak intensity (light brown), 2 for moderate intensity (brown), and 3 for strong intensity (dark brown), while the distribution was measured based on the percentage of cells expressed per field of view with scoring of 1 if the percentage of cells in the field of view was 0–20%, 2 if 20%–50%, 3 if 50%–80%, and 4 if >80%. Histoscores have a range of values of 0–12.
Assessment of VEGF Expression and Vascularization Around Fibrous Encapsulation
VEGF expression was measured using sandwich ELISA. Results were interpreted using a microplate spectrophotometer/ELISA reader at 450 nm wavelengths. VEGF expression was measured using MPM6 software. Histopathology examinations were carried out to measure the formation of vascularization on fibrotic capsules. Both ELISA and histopathology examinations were carried out at the Integrated Research Laboratory, Faculty of Veterinary, Universitas Syiah Kuala, Aceh, Indonesia.
The procedure for histology preparations was the modified Kiernan (1990) method. Organs that had been fixed in a 10% BNF solution were put into a labeled tissue basket. Tissue samples were dehydrated with graded alcohol of 80%, 90%, 95%, and absolute alcohol for 2 hours each. After dehydration, purification was carried out by immersing the tissue in silol I, II, and III for 1 hour each.
The next stage was tissue infiltration in liquid paraffin I, II, and III at a temperature of 60°C for 1 hour each and continued with implanting tissue in paraffin (embedding). The tissue block was sliced with a thickness of 3 mm using a microtome placed on a glass object that had been coated with poly-L-lysine. The tissue blocks were cut into 14 slides (three samples were taken from each group) and two of them were used as controls. The interpretation of the results of the blood vessels in the fibrotic capsule is carried out by counting the blood vessels that appear in 5 large visual fields with 40× magnification.
Statistical Analysis
Independent t-tests with 95% CIs were used to analyze the effect of PRP administration on VEGF expression, while the Mann–Whitney test was used to analyze the effect of PRP administration on type I collagen production and the formation of vascularization around the fibrous encapsulation. Statistical analyses were done using SPSS 18.0, and values were considered significant if p<0.05.
Results
Effect of PRP Administration on Type I Collagen Production
IHC examination showed that all rats in the T1 group had type I collagen counts of 50–>150/field of view, with a majority (66.7%) having 100–149/field of view. On the other hand, most rats in the C1 group (83.3%) had 0–49/field of view. Statistical analysis showed the T1 group had significantly more type I collagen than the C1 group (p=0.003; Table 1, Figure 2).
 |
Table 1 Type I collagen numbers in groups T1 and C1 |
Effect of PRP Administration on VEGF Expression and Vascularization Formation
The mean expression of VEGF in the T2 group was significantly higher than in the C2 group: 10.90±4.47 and 2.29±0.92, respectively (p=0.006). Histological examination with 40× magnification showed that the the average number of vessels formed on fibrotic capsules in the T2 group was significantly (p=0.007) higher than in the C2 group (2.69±1.03 vs 0.67±0.52; Table 2, Figure 3).
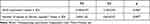 |
Table 2 VEGF expression and vascularization formation in groups T2 and C2 |
 |
Figure 3 Histology of blood vessels in fibrotic capsule in tissue surrounding implants. (A) Implant treatment group+ PRP group (40×); (B) implant treatment group (40×). |
Discussion
This study was conducted to evaluate the effect of PRP administration on type I collagen production, VEGF expression, and vascularization on fibrotic capsules in rat models after femoral bone–implant insertion. We found that the amount of type I collagen in group T1 was significantly higher than in C1 (p=0.003). This finding supports previous studies that showed PRP administration increased collagen production.21,35 Cho et al35 found a significant increase of fibroblasts and collagen production on female rats injected with subcutaneous PRP compared to controls. The study concluded that increased fibroblast proliferation was associated with increased collagen production induced by PRP administration.
PRP is rich in FGF, which is responsible for extracellular matrix and collagen synthesis, important in tissue repair and regeneration. There are 28 types of collagen that have been identified, with type I the most abundant form. Type I collagen can be found in almost every single tissue type in the body, except in cartilage. Synthesis of type I collagen usually occurs in response to trauma,36,37 where it is usually detected on the third day after injury and increases until the third week.20,21 This explains why type I collagen was also found in the C1 group. PRP administration in the T1 group significantly increased the production of type I collagen 7 days after the procedure compared to the natural production of type I collagen in the C1 group.
Increased production of type I collagen helps the bone-healing process. Studies have shown that type I collagen administration on implant surfaces increases the formation of new vessels around fibrotic capsules.20,21 One investigation also reported that type I collagen administration decreased rejection and implant-failure incidence.22 As PRP can induce the production of type I collagen, it has the potential to increase the formation of new vessels around fibrotic capsules, which might reduce implant failure after the implant procedure. New bone formation, bone regeneration, and osseointegration after implant placement requires a blood supply to deliver nutrients, oxygen, and osteoprogenitor cells through the newly formed blood vessels.40
We also found that VEGF expression in the T2 group was significantly higher than in the C2 group. VEGF regulation is a complex mechanism, induced by growth factors, such hormones such as estrogen and parathyroid, inflammatory factors, eg, IL1, IL6, and IL8, and mechanical stress.24 This finding is in accordance with previous studies that showed the administration of PRP increased VEGF expression.15–17 PRP, which is rich in growth factors, produces fibroblasts, which induced VEGF expression in the T2 group.
Furthermore, we found that the number of vessels on fibrotic capsules in the T2 group was significantly higher than C2, indicating better neovascularization on fibrotic capsules in the treatment group. VEGF is pivotal in the proliferation, migration, and activation of vascular endothelial cells, vascular permeability, and antiapoptosis on newly formed vascular endothelial cells.24–26,38 VEGF induced by PRP administration stimulated neovascularization on fibrotic capsules. The formation of microvessels continued with formation of the capsule up to the third week (21st day) after implant insertion, resulting in a higher amount of neovascularization in T2 than C2. This finding supported previous studies that suggested VEGF enhanced neovascularization.24,26
Neovascularization on fibrotic capsules around the implant is important in preventing infection complications and enhancing the bone-healing process.6 The use of modified implants and exogenous type I collagen as well as VEGF enhances vascularization on fibrotic capsules around implants.21,22,29,30 However, these procedures are not without a risk of rejection and failure.31–34 The findings of this study showed that the administration of PRP extracted from a mouse model increased type I collagen production and VEGF expression, which eventually increased neovascularization on fibrotic capsules around implants.
Limitations
The results of this study must be interpreted with caution and limitations borne in mind. First, we focused only on the production of type I collagen and VEGF expression induced by PRP administration. In fact, PRP is rich in other growth factors, such as PDGF and TNFα, which might also influence the angiogenesis process. A study integrating all these growth factor in the future is warranted to explain the role of each factor on osteogenesis and angiogenesis following implant insertion. Second, the results of IHC examinations are presented in the amount of type I collagen found. Measurement of capsule fibrosis using IHC results in the future might enrich the findings of this study. Despite these limitations, we believe that this study has significantly contributed to the current knowledge of PRP potential in bone healing.
Conclusion
The findings of this study showed that the administration of PRP significantly increased type I collagen production, VEGF expression, and neovascularization on fibrotic capsules around implants in rat models postfollowing femoral bone insertion. As PRP is considered cheaper, safer, and easier to prepare, PRP in implant insertions should be considered, since it might reduce complications and enhance the healing process following implant surgeries. Overall, this study proves the impact of PRP on indirect healing following the implant-graft procedure through the role of type I collagen, decreased fibrotic capsules, and increased VEGF expression. As far as we know, the novelty in this study is the assessment of aspects of type I collagen and VEGF, which were assessed using IHC procedures and provided a perspective on the reduction of fibrotic tissue at the implant site.
Acknowledgment
We would like to thank FICTRO Studio for assistance during the study and manuscript preparation.
Author Contributions
All authors made a significant contribution to the work reported, whether in conception, study design, execution, acquisition of data, analysis and interpretation, or all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval to the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. Khan MS, Ur Rehman S, Ali MA, Sultan B, Sultan S. Infection in orthopedic implant surgery, its risk factors and outcome. J Ayub Med Coll Abbottabad. 2008;20(1):23–25.
2. Brady R, Calhoun J, Leid J, Shirtliff M Infections of orthopaedic implants and devices; 1970: 15–55.
3. Shapiro IM, Hickok NJ, Parvizi J, Stewart S, Schaer TP. Molecular engineering of an orthopaedic implant: from bench to bedside. Eur Cell Mater. 2012;23:362–370. doi:10.22203/eCM.v023a28
4. Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008;20(2):86–100. doi:10.1016/j.smim.2007.11.004
5. Major MR, Wong VW, Nelson ER, Longaker MT, Gurtner GC. The foreign body response: at the interface of surgery and bioengineering. Plast Reconstr Surg. 2015;135(5):1489–1498. doi:10.1097/PRS.0000000000001193
6. Bartoli CR, Godleski JJ. Blood flow in the foreign-body capsules surrounding surgically implanted subcutaneous devices. J Surg Res. 2010;158(1):147–154. doi:10.1016/j.jss.2008.07.045
7. Bartoli CR, Nadar MM, Godleski JJ. Capsule thickness correlates with vascular density and blood flow within foreign-body capsules surrounding surgically implanted subcutaneous devices. Artif Organs. 2010;34(10):857–861. doi:10.1111/j.1525-1594.2010.01024.x
8. Bishop JA, Palanca AA, Bellino MJ, Lowenberg DW. Assessment of compromised fracture healing. J Am Acad Orthop Surg. 2012;20(5):273–282. doi:10.5435/JAAOS-20-05-273
9. Dimitriou R, Tsiridis E, Giannoudis PV. Current concepts of molecular aspects of bone healing. Injury. 2005;36(12):1392–1404. doi:10.1016/j.injury.2005.07.019
10. Rodriguez IA, Growney Kalaf EA, Bowlin GL, Sell SA. Platelet-rich plasma in bone regeneration: engineering the delivery for improved clinical efficacy. Biomed Res Int. 2014;2014:392398. doi:10.1155/2014/392398
11. Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009;37(11):2259–2272. doi:10.1177/0363546509349921
12. Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62(4):489–496. doi:10.1016/j.joms.2003.12.003
13. Zhang N, Wu YP, Qian SJ, Teng C, Chen S, Li H. Research progress in the mechanism of effect of PRP in bone deficiency healing. Sci World J. 2013;2013:134582. doi:10.1155/2013/134582
14. Oryan A, Meimandi Parizi A, Shafiei-Sarvestani Z, Bigham AS. Effects of combined hydroxyapatite and human platelet rich plasma on bone healing in rabbit model: radiological, macroscopical, histopathological and biomechanical evaluation. Cell Tissue Bank. 2012;13(4):639–651. doi:10.1007/s10561-011-9285-x
15. Rozman P, Bolta Z. Use of platelet growth factors in treating wounds and soft-tissue injuries. Acta Dermatovenerol Alp Pannonica Adriat. 2007;16(4):156–165.
16. Mehta S, Watson JT. Platelet rich concentrate: basic science and current clinical applications. J Orthop Trauma. 2008;22(6):432–438. doi:10.1097/BOT.0b013e31817e793f
17. Smith RG, Gassman CJ, Campbell MS. Platelet-rich plasma: properties and clinical applications. J Lancaster Gen Hosp. 2007;2(2):73–78.
18. Kruger JP, Freymannx U, Vetterlein S, Neumann K, Endres M, Kaps C. Bioactive factors in platelet-rich plasma obtained by apheresis. Transfus Med Hemother. 2013;40(6):432–440. doi:10.1159/000356329
19. Nurden AT. Platelets, inflammation and tissue regeneration. Thromb Haemost. 2011;105(Suppl 1):S13–33. doi:10.1160/THS10-11-0720
20. Tiedtke J, Marks O, Morel J. Stimulation of collagen production in human fibroblasts. Cosmet Sci Tech. 2007;15:15–18.
21. Ring A, Langer S, Tilkorn D, et al. Induction of angiogenesis and neovascularization in adjacent tissue of plasma-collagen-coated silicone implants. Eplasty. 2010;10:e61.
22. Hsieh CYC, Hu F-W, Chen W-S, Tsai W-B. Reducing the foreign body reaction by surface modification with collagen/hyaluronic acid multilayered films. Int Sch Res Notices. 2014;2014:8.
23. Senger DR. Vascular endothelial growth factor: much more than an angiogenesis factor. Mol Biol Cell. 2010;21(3):377–379. doi:10.1091/mbc.e09-07-0591
24. Hu K, Olsen BR. The roles of vascular endothelial growth factor in bone repair and regeneration. Bone. 2016;91:30–38. doi:10.1016/j.bone.2016.06.013
25. Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003;9(6):669–676. doi:10.1038/nm0603-669
26. Kaigler D, Wang Z, Horger K, Mooney DJ, Krebsbach PH. VEGF scaffolds enhance angiogenesis and bone regeneration in irradiated osseous defects. J Bone Miner Res. 2006;21(5):735–744. doi:10.1359/jbmr.060120
27. Li B, Wang H, Qiu G, Su X, Wu Z. Synergistic effects of vascular endothelial growth factor on bone morphogenetic proteins induced bone formation in vivo: influencing factors and future research directions. Biomed Res Int. 2016;2016:2869572. doi:10.1155/2016/2869572
28. Gerber HP, Vu TH, Ryan AM, Kowalski J, Werb Z, Ferrara N. VEGF couples hypertrophic cartilage remodeling, ossification and angiogenesis during endochondral bone formation. Nat Med. 1999;5(6):623–628. doi:10.1038/9467
29. Kim DH, Song YS, Song SY, Kim CH. The effects of vascular endothelial growth factor on capsule formation around silicone implant in rats. Arch Aesthetic Plast Surg. 2016;22(3):129–134. doi:10.14730/aaps.2016.22.3.129
30. Ueda H, Hong L, Yamamoto M, et al. Use of collagen sponge incorporating transforming growth factor-beta1 to promote bone repair in skull defects in rabbits. Biomaterials. 2002;23(4):1003–1010. doi:10.1016/S0142-9612(01)00211-3
31. Richardson TP, Peters MC, Ennett AB, Mooney DJ. Polymeric system for dual growth factor delivery. Nat Biotechnol. 2001;19(11):1029–1034. doi:10.1038/nbt1101-1029
32. Poldervaart MT, Wang H, van der Stok J, et al. Sustained release of BMP-2 in bioprinted alginate for osteogenicity in mice and rats. PLoS One. 2013;8(8):e72610. doi:10.1371/journal.pone.0072610
33. Engsig MT, Chen QJ, Vu TH, et al. Matrix metalloproteinase 9 and vascular endothelial growth factor are essential for osteoclast recruitment into developing long bones. J Cell Biol. 2000;151(4):879–889. doi:10.1083/jcb.151.4.879
34. Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004;91(1):4–15. doi:10.1160/TH03-07-0440
35. Cho JM, Lee YH, Baek RM, Lee SW. Effect of platelet-rich plasma on ultraviolet b-induced skin wrinkles in nude mice. J Plast Reconstr Aesthet Surg. 2011;64(2):e31–39. doi:10.1016/j.bjps.2010.08.014
36. Baxter LC, Frauchiger V, Textor M, Gwynn I, Richards RG. Fibroblast and osteoblast adhesion and morphology on calcium phosphate surfaces. Eur Cell Mater. 2002;4:1–17. doi:10.22203/eCM.v004a01
37. Tangsadthakun C, Kanokpanont S, Sanchavanakit N, Banaprasert T, Damrongsakkul S. Properties of Collagen/Chitosan Scaffolds for skin tissue engineering. J Met Mater Miner. 2006;16(1):37–44.
38. Donnini S, Ziche M, Morbidelli L, Harmey J Molecular mechanisms of VEGF-induced angiogenesis. 2011: 19–25.
39. Hsu SM, Raine L, Fanger H. The use of antiavidin antibody and avidin-biotin-peroxidase complex in immunoperoxidase technics. Am J Clin Pathol. 1981;75(6):816–821. PMID: 6167159. doi:10.1093/ajcp/75.6.816
40. Saghiri MA, Asatourian A, Garcia-Godoy F, Sheibani N. The role of angiogenesis in implant dentistry part I: review of titanium alloys, surface characteristics and treatments. Med Oral Patol Oral Cir Bucal. 2016;21(4):e514–525. PMID: 27031073; PMCID: PMC4920467. doi:10.4317/medoral.21199
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

