Back to Journals » Patient Preference and Adherence » Volume 17
The Effect of Clinical Pharmacist Intervention on Renal Function Impairment in Patients with Antimicrobial-Induced Acute Kidney Injury in ICU
Authors Hou J, Li JF, Yan XJ, Zhang YL, Zhang MY, Zhang Y
Received 16 November 2022
Accepted for publication 28 February 2023
Published 16 March 2023 Volume 2023:17 Pages 711—718
DOI https://doi.org/10.2147/PPA.S397873
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Qizhi (Cathy) Yao
Jia Hou, Jin-Feng Li, Xiu-Juan Yan, Yong-Liang Zhang, Meng-Yu Zhang, Yuan Zhang
Department of Pharmacy, Weihai Municipal Hospital, Cheeloo College of Medicine, Shandong University, Weihai, People’s Republic of China
Correspondence: Yuan Zhang, Department of Pharmacy, Weihai Municipal Hospital, Cheeloo College of Medicine, Shandong University, No. 70 Heping Road, Huancui District, Weihai City, Shandong Province, 264200, People’s Republic of China, Tel +86-18660377685, Email [email protected]
Objective: The purpose of this study was to analyze the improvement effect of clinical pharmacist intervention on renal function impairment in patients with antimicrobial-induced acute kidney injury (AKI).
Methods: A total of 145 patients with AKI caused by antibiotics admitted to the ICU department were selected as the research subjects. The patients were divided into the control group (n=57) and the intervention group (n=88) according to whether there were ICU specialist clinical pharmacists involved in clinical treatment. The renal function outcome and infection control were evaluated in the two groups.
Results: The proportion of renal function outcome in the intervention group was 88.6%, which was significantly higher than that in the control group. However, there was no statistically significant difference in infection control between the two groups. For the intervention group, the clinical pharmacists adopted three intervention methods: dose adjustment, drug replacement and CRRT treatment, respectively, according to the disease conditions of AKI patients. Among them, dose adjustment and drug replacement were the most frequently used intervention methods. In addition, the proportion of renal function outcome was higher in the group of patients who changed antibiotics and underwent CRRT, which were 93.1% and 100%, respectively. The adjusted-dose group had the highest infection control rate at 82.1%. However, there were no statistically significant differences in renal function outcomes and infection control among the three interventions.
Conclusion: Clinical pharmacists participating in the clinical treatment of patients with antimicrobial-induced AKI in ICU can effectively improve the renal function of patients.
Keywords: clinical pharmacists, acute kidney injury, antimicrobial, renal function
Introduction
Acute kidney injury (AKI) is a common multidisciplinary clinical critical illness, and its incidence is increasing year by year.1,2 Globally, there are approximately 13.3 million new cases of AKI each year, and nearly 1.7 million deaths due to AKI and its complications.3 In the intensive care unit (ICU), patients often have multiple risk factors, including sepsis, surgery, shock, advanced age, heart failure, use of contrast agents and nephrotoxic drugs, and have a higher incidence and mortality of AKI.4 Drugs have been reported to be the third leading cause of AKI with poor prognosis, especially in critically ill patients.5 With the increasing number of new antibacterial drugs and their wide clinical application, antibacterial drug-related AKI is increasing. Antibiotic-related AKI refers to new kidney injury or exacerbation of existing kidney disease after the use of antibiotics.6 It has been reported that about 40% of AKI in China is caused by drugs, of which antibiotics are the most common type of drugs.6 A systematic review of drug-induced AKI in the Chinese population showed that among drug-related AKI, 47.5% of the drugs were antimicrobials.7 Misuse or irrational use of antimicrobials increases the risk of bacterial resistance and/or adverse drug reactions.8 It is particularly important to implement therapeutic drug monitoring and individualized medication according to the patient’s clinical situation.
Pharmaceutical services led by clinical pharmacists play an important role in the prevention and treatment of nosocomial infections. As a member of the medical team, clinical pharmacists play an important role in drug use, especially in drug concentration monitoring and drug monitoring.9 During the treatment of AKI patients, clinical pharmacists assist physicians in formulating treatment plans, strengthen pharmaceutical care for anti-infective treatment, and provide targeted suggestions and improvement measures, including adjustment of concomitant drugs and drug doses.10 The purpose of this study was to analyze the improvement effect of clinical pharmacist intervention on renal function impairment in patients with antimicrobial-induced AKI. We hope to provide reference and thinking for clinical pharmacists to carry out antimicrobial pharmaceutical services in ICU.
Materials and Methods
Objects
Patients with AKI caused by antibiotics admitted to the ICU department from 2016 to 2018 (control group) and 2019 to 2021 (intervention group) were selected as the research subjects. Among them, there were 57 cases in the control group and 88 cases in the intervention group. The control group was given routine treatment by clinicians. In the intervention group, in addition to routine treatment given by clinicians, ICU specialist clinical pharmacists participated in clinical treatment. The basic conditions of the two groups of patients are shown in Table 1. This study obtained written informed consent from all participants before participating in the study, which also was approved by Medical Ethics Committee of Weihai Municipal Hospital [2020048].
 |
Table 1 Comparison of the General Situation of AKI Patients in the Intervention Group and the Control Group |
According to the AKI diagnostic criteria,11 AKI was determined by the presence of one of the following: (1) an increase in serum creatinine of 26.5 μmol·L−1 at 48 hours or more than 50% from baseline at 7 days according to Kidney Disease Improvement Global Organization; (2) serum cystatin C (>1.1 mg·L−1); (3) urine output (<0.5mL· (kg·h)−1 for >6 hours or more). Inclusion criteria: patients using antimicrobial drugs before the onset of AKI, using Excel software and applying computerized C# language to prepare a graph of the relationship between serum creatinine, cystatin C changes and medication use, based on the Naranjo assessment scale,12 and the criteria for association evaluation were: certain: ≥9 points, very likely: 5–8 points, probable: 1–4 points, and unlikely: ≤0 points. The patients were included in the study if the association between antibiotics and AKI was ≥1. Exclusion criteria: (1) AKI was diagnosed at admission; (2) glomerular filtration rate ≤ 15 mL·min-1 at admission; (3) those with a history of systemic diseases leading to renal injury; (4) history of kidney or urinary calculi; (5) higher body fat ratio, septic shock and surgery; (6) combined use of other drugs that can significantly cause renal injury (such as imidazole sedatives, glucocorticoids, opioids, angiotensin II receptor blockers, angiotensin converting enzyme inhibitors and non-steroidal anti-inflammatory drugs); (7) Severe heart failure (LVEF<35% or NYHA grade IV); (8) diabetes; (9) abnormal liver function (alanine aminotransferase (ALT) or aspartate aminotransferase (AST) ≥ 3 times the upper limit of normal value; (10) incomplete and untraceable medical records.
Intervention Methods
The study flow chart was detailed in Figure 1.
 |
Figure 1 Flow chart of the trial. ICU, intensive care unit; AKI, acute kidney injury; CRRT, continuous renal replacement therapy. |
The ICU specialist clinical pharmacist provides pharmaceutical care of the patient and offers three interventions to the clinician: adjustment of antimicrobial drug dose (Dose adjustment group), change of antimicrobial drug species (Drug change group), and use of continuous renal replacement therapy (CRRT) (CRRT group), taking into account the actual condition of the patient. The specific operations include (1) clinical pharmacists calculate Ccr based on serum creatinine values using the Cockcroft-Gault (C-G) formula,13 and make dose adjustment for antimicrobial drugs used in patients with Ccr <50 mL-min-1; (2) carry out vancomycin blood concentration monitoring according to existing conditions, and adjust vancomycin dose according to the trough concentration value; (3) change the dose of vancomycin according to the (3) replace the antimicrobial drug species with low nephrotoxicity according to the results of drug sensitivity experiments; (4) treat with CRRT if necessary, and clinical pharmacists provide the dose adjustment plan of antimicrobial drugs during CRRT.
C-G formula: Ccr = [(140 - age) × body weight (kg)] / [0.818 × serum creatinine (μmol-L −1)]; for women, the calculation was based on the result × 0.85.
Evaluation Indicators
A gradual decrease in blood creatinine and cystatin C levels to baseline levels or normal levels, an increase in the patient’s urine output, and a normal nature of urine were used as evaluation criteria for the regression of renal function.14 A significant decrease in inflammatory indicators, clearance or partial clearance of infection foci, and improvement in imaging were used as criteria for infection control.15
Statistical Analysis
Statistical analysis of the results was performed using SPSS 16. All continuous measurements are expressed as mean ± standard deviation. Student’s t-test was used for comparisons between two groups, and analysis of variance was used for comparisons among three groups. The count data are expressed as percentages. The comparisons were performed with the chi square test or Fisher’s exact test. The p-value <0.05 was considered statistically significant.
Results
General Situation And Antibiotic Categories of Patients
There were no significant differences between the intervention group and the control group in terms of age, gender, reason for admission, disease history, clinical manifestations, length of hospital stay, and duration of medication at the time of AKI (Table 1). In addition, there was no significant difference in serum creatinine and cystatin C levels between the two groups of AKI patients (Table 1). Analyzing the use of antibiotics in the two groups of patients, it was found that the top 4 types of antibiotics causing AKI cases were carbapenems, β-lactams, glycopeptides and aminoglycosides (Table 2). There was no significant difference between the two groups in terms of drug varieties and usage and dosage (Table 2).
 |
Table 2 Comparison of Antibiotic Categories, Drugs, Usage and Dosage Between the Intervention Group and the Control Group (n, %) |
Prognosis of AKI Patients in the Intervention and Control Groups
Subsequently, we assessed the prognosis of patients with AKI in the control and intervention groups by analyzing renal function outcomes and infection control. The results showed that the renal function outcome rate of AKI patients in the intervention group was 88.6%, which was significantly higher than that in the control group (Table 3). There was no difference in SOFA and APACHE scores between the two groups, indicating that there is no difference in the prognosis of the two groups (Table 3). However, there was no statistically significant difference in infection control between the two groups (Table 4).
 |
Table 3 The Improvement of Renal Function in the Intervention Group and the Control Group (n, %) |
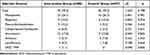 |
Table 4 Infection Control of Patients in the Intervention Group and Control Group (n, %) |
The Effect of Different Intervention Methods on the Prognosis of AKI in the Intervention Group
For the intervention group, the clinical pharmacists adopted three intervention methods: adjusting the dose, changing the drug and CRRT treatment according to the disease conditions of the AKI patients. Among them, dose adjustment and drug replacement are the most frequently used intervention methods by clinical pharmacists. Moreover, we analyzed the improvement of the prognosis of patients with AKI in the intervention group by different intervention methods (Table 5). The proportion of renal function outcome in the patients who changed antibiotics and underwent CRRT was higher, which were 93.1% and 100%, respectively. Furthermore, the adjusted-dose group had the highest infection control rate at 82.1%. However, there were no statistically significant differences in renal function outcomes and infection control among the three interventions (Table 5).
 |
Table 5 The Effect of Different Intervention Methods on the Renal Function and Infection Control of AKI in the Intervention Group (n, %) |
Discussion
AKI has become one of the common clinical critical illnesses ICU patients are critically ill, have more underlying diseases, and some of them are accompanied by organ insufficiency, so AKI occurs more frequently. Studies have found that the incidence of AKI in critically ill patients ranges from 10% to 60%,16 and it is one of the diseases that affects the mortality and mortality of critically ill patients. Jiang et al17 reported a mortality rate of 27.7% for AKI in ICU patients during hospitalization. Drugs are one of the important factors that cause AKI in hospitalized patients.18 The widespread use of antibiotics has led to an increase in clinical adverse reactions year by year, which has become the main cause of drug-related renal damage. A retrospective study found that the rate of AKI caused by antibiotics was 63%. The medication structure varies by region and department, and the results of studies vary.19 In the current study, the top 4 classes of antibacterial drugs that cause AKI are carbapenems, β-lactams, glycopeptides, and aminoglycosides. Amikacin and vancomycin caused the highest rates of AKI compared with the number of antimicrobials used in ICU wards during the same period.
Effective antimicrobial stewardship (AMS) produces positive clinical outcomes.20 The goal of AMS in the ICU is to optimize antimicrobial use.21 Clinical pharmacists are an important part of AMS. Clinical pharmacists have professional knowledge in pharmacokinetics and pharmacodynamics, which is beneficial for adjusting the dose of antibiotics used in critically ill patients.22 An AMS team including clinical pharmacists can shorten the duration of antibacterial treatment and reduce the occurrence of infectious complications.23,24 Absence of clinical pharmacists results in increased use of restricted antibiotics and prolonged duration of antibiotic therapy.25 In ICU management without clinical pharmacist participation, patients with community-acquired infections, hospital-acquired infections, and sepsis had increased mortality.24,26 In the current study, we found that clinical pharmacist intervention can significantly improve renal function in patients with antimicrobial-induced AKI. CRRT is the mainstay of treatment for AKI.27 The choice of drug dose and dosing interval is a complex issue due to the large variability in the pharmacokinetic parameters of antimicrobials among patients undergoing CRRT. Underdose directly leads to treatment failure and bacterial resistance, while overdose leads to increased drug toxicity.28 Zarbock et al29 proposed that early initiation of CRRT could help reduce 90-day mortality in patients with severe AKI. Dose adjustment and changing the variety of antimicrobial drugs are the most commonly used intervention methods for clinical pharmacists in the current study, and the infection control rate is the highest in the dose adjustment group. What is more, changing the type of drugs and using CRRT is more conducive to the improvement of renal function in patients. In this study, the clinical pharmacists adopted three intervention methods: adjusting the dose, changing the drug and CRRT treatment according to the disease conditions of the AKI patients. The intervention of pharmacists plays an important role in improving renal injury.
There are still many deficiencies in this study. Firstly, there is a lack of long-term mechanism analysis for the rational application of antibiotics, such as the detection rate, drug resistance rate and economy of pathogenic bacteria. Secondly, the data of this study is a single center, and the time and space span is relatively limited. And the sample size of this study is not large enough. Nonetheless, this study explored the mode of antimicrobial management of clinical pharmacists in ICU, which provided reference and thinking for further optimizing clinical pharmacy services.
In conclusion, clinical pharmacists participating in the clinical treatment of patients with antimicrobial-induced AKI in ICU can effectively improve the renal function of patients. Among the commonly used intervention methods, comparing with adjusting drug dose choosing to change the variety of drugs and use CRRT is more conducive to the improvement of the renal function of AKI patients.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Weihai Municipal Hospital, Cheeloo College of Medicine, Shandong University . All participants signed an informed consent form for inclusion in the study.
Acknowledgments
Shandong University Health Care Big Data Research Institute, Shandong University Specialized Disease Cohort Big Data Research Center.
Funding
Clinical Pharmaceutical Research Fund of Shandong Medical Association (YXH2021ZX021).
Disclosure
All of the authors had no any personal, financial, commercial or academic conflicts of interest separately in this work.
References
1. Yang CW, Li S, Dong Y, Paliwal N, Wang Y. Epidemiology and the Impact of acute kidney injury on outcomes in patients with rhabdomyolysis. J Clin Med. 2021;10(9):1950. doi:10.3390/jcm10091950
2. Hoste EAJ, Kellum JA, Selby NM. Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol. 2018;14(10):607–625. doi:10.1038/s41581-018-0052-0
3. Mehta RL, Cerdá J, Burdmann EA, et al. International Society of Nephrology’s 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet. 2015;385(9987):2616–2643. doi:10.1016/S0140-6736(15)60126-X
4. Jiang F, Su L, Xiang H, et al. Incidence, risk factors, and biomarkers predicting ischemic or hemorrhagic stroke associated acute kidney injury and outcome: a retrospective study in a general intensive care unit. Blood Purif. 2019;47(4):317–326. doi:10.1159/000499029
5. Uchino S. The epidemiology of acute renal failure in the world. Curr Opin Crit Care. 2006;12(6):538–543. doi:10.1097/01.ccx.0000247448.94252.5a
6. Xu X, Nie S, Liu Z, et al. Epidemiology and clinical correlates of aki in Chinese hospitalized adults. Clin J Am Soc Nephrol. 2015;10(9):1510–1518. doi:10.2215/CJN.02140215
7. Pan K, Chen C, Jiang Y, et al. Systematic review of drug-induced acute kidney injury in Chinese population. China Pharm. 2021;32(9):8.
8. Sierra MA, Casarrubios L, de la Torre MC. Bio-organometallic derivatives of antibacterial drugs. Chemistry. 2019;25(30):7232–7242. doi:10.1002/chem.201805985
9. Niznik JD, He H, Kane-Gill SL. Impact of clinical pharmacist services delivered via telemedicine in the outpatient or ambulatory care setting: a systematic review. Res Social Adm Pharm. 2018;14(8):707–717. doi:10.1016/j.sapharm.2017.10.011
10. Goswami EAS, Sexton E, Fadrowski JJ. Pediatric nurse and pharmacist knowledge of acute kidney injury. Hosp Pediatr. 2021;11(8):871–877. doi:10.1542/hpeds.2020-005773
11. Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–184. doi:10.1159/000339789
12. Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239–245. doi:10.1038/clpt.1981.154
13. Zhou T. Accuracy comparison of creatinine clearance rate predicted by Cockcroft-Gault formula with the actual body weight or the ideal body weight. Pharm Care Res. 2017;17(6):3.
14. Chawla LS, Eggers PW, Star, RA et al. Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med. 2014;371(1):58–66. doi:10.1056/NEJMra1214243
15. Cui N, Zhang H, Chen Z, Yu Z. Prognostic significance of PCT and CRP evaluation for adult ICU patients with sepsis and septic shock: retrospective analysis of 59 cases. J Int Med Res. 2019;47(4):1573–1579. doi:10.1177/0300060518822404
16. Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394(10212):1949–1964. doi:10.1016/S0140-6736(19)32563-2
17. Jiang L, Zhu Y, Luo X, et al. Epidemiology of acute kidney injury in intensive care units in Beijing: the multi-center BAKIT study. BMC Nephrol. 2019;20(1):468. doi:10.1186/s12882-019-1660-z
18. Zarb P, Coignard B, Griskeviciene J, et al. The European Centre for Disease Prevention and Control (ECDC) pilot point prevalence survey of healthcare-associated infections and antimicrobial use. Euro Surveill. 2012;17(46). doi:10.2807/ese.17.46.20316-en
19. Cheng J, Jiang H, Liu X, Lei Q, Wu Q, Ma T. Clinical analysis of 38 cases of acute kidney injury caused by antibiotics. Chin J Pharmacoepidemiol. 2007;16(3):2.
20. Dyar OJ, Huttner B, Schouten J, Pulcini C. What is antimicrobial stewardship? Clin Microbiol Infect. 2017;23(11):793–798. doi:10.1016/j.cmi.2017.08.026
21. Pickens CI, Wunderink RG. Principles and Practice of Antibiotic Stewardship in the ICU. Chest. 2019;156(1):163–171. doi:10.1016/j.chest.2019.01.013
22. Pulia M, Redwood R, May L. Antimicrobial Stewardship in the Emergency Department. Emerg Med Clin North Am. 2018;36(4):853–872. doi:10.1016/j.emc.2018.06.012
23. Carver PL, Lin SW, DePestel DD, Newton DW. Impact of mecA gene testing and intervention by infectious disease clinical pharmacists on time to optimal antimicrobial therapy for Staphylococcus aureus bacteremia at a University Hospital. J Clin Microbiol. 2008;46(7):2381–2383. doi:10.1128/JCM.00801-08
24. Gentry CA, Greenfield RA, Slater LN, Wack M, Huycke MM. Outcomes of an antimicrobial control program in a teaching hospital. Am J Health Syst Pharm. 2000;57(3):268–274. doi:10.1093/ajhp/57.3.268
25. Cappelletty D, Jacobs D. Evaluating the impact of a pharmacist’s absence from an antimicrobial stewardship team. Am J Health Syst Pharm. 2013;70(12):1065–1069. doi:10.2146/ajhp120482
26. MacLaren R, Bond CA, Martin SJ, Fike D. Clinical and economic outcomes of involving pharmacists in the direct care of critically ill patients with infections. Crit Care Med. 2008;36(12):3184–3189. doi:10.1097/CCM.0b013e31818f2269
27. Karkar A, Ronco C. Prescription of CRRT: a pathway to optimize therapy. Ann Intensive Care. 2020;10(1):32. doi:10.1186/s13613-020-0648-y
28. Roberts JA, Kruger P, Paterson DL, Lipman J. Antibiotic resistance--what’s dosing got to do with it? Crit Care Med. 2008;36(8):2433–2440. doi:10.1097/CCM.0b013e318180fe62
29. Zarbock A, Kellum JA, Schmidt C, et al. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically ill patients with acute kidney injury: the ELAIN randomized clinical trial. JAMA. 2016;315(20):2190–2199. doi:10.1001/jama.2016.5828
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
