Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
The Distribution of Alpha-1 Antitrypsin Genotypes Between Patients with COPD/Emphysema, Asthma and Bronchiectasis
Authors Veith M, Tüffers J , Peychev E, Klemmer A, Kotke V, Janciauskiene S , Wilhelm S, Bals R, Koczulla AR , Vogelmeier CF, Greulich T
Received 11 July 2020
Accepted for publication 14 October 2020
Published 6 November 2020 Volume 2020:15 Pages 2827—2836
DOI https://doi.org/10.2147/COPD.S271810
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Martina Veith,1 Julia Tüffers,1 Erika Peychev,1 Andreas Klemmer,1 Viktor Kotke,1 Sabina Janciauskiene,2 Susanne Wilhelm,1 Robert Bals,3 Andreas Rembert Koczulla,4 Claus Franz Vogelmeier,1 Timm Greulich1
1Department of Medicine, Pulmonary and Critical Care Medicine, University Medical Center Giessen and Marburg, Member of the German Center for Lung Research, Marburg, Germany; 2Clinic for Pneumology, German Center for Lung Research (DZL), Medical University Hannover, Hannover, Germany; 3Department of Internal Medicine V, Pulmonology, Allergology, Respiratory and Intensive Care Medicine, Saarland Hospital, Homburg/Saar, Germany; 4Institute for Pulmonary Rehabilitation Research, Schoen Klinik Berchtesgadener Land, Teaching Hospital of Philipps-University of Marburg, Marburg, Germany
Correspondence: Martina Veith
Department of Medicine, Pulmonary and Critical Care Medicine, University Medical Center Giessen and Marburg, Member of the German Center for Lung Research, Marburg, Germany
Tel +4964215864723
Fax +496421586370
Email [email protected]
Purpose: Alpha-1-antitrypsin deficiency (AATD) is a rare hereditary condition characterized by low circulating levels of alpha-1antitrypsin (AAT). While the association between AATD and COPD/emphysema is undisputed, the association between AATD and asthma or bronchiectasis is still a matter of debate.
Aims and Objectives: Our study aimed to investigate the distribution of AAT genotypes between patients with COPD/emphysema, asthma and bronchiectasis. To back up the diagnostic labels, we described symptoms associated with the diagnosis.
Methods: Between September 2003 and March 2020, 29,465 testing kits (AlphaKit®) were analyzed in the AAT laboratory, University of Marburg, Germany. The diagnosis of AATD has been made based on the measurements of AAT serum levels, followed by genotyping, phenotyping or whole gene sequencing depending on the availability and/or the need for more detailed interpretation of the results. The respiratory symptoms were recorded as well.
Results: Regarding the distribution of the wild type allele M and the most frequent mutations S (E264V) and Z (E342K), no significant differences could be found between COPD/emphysema [Pi*MM (58.24%); Pi*SZ (2.49%); Pi*ZZ (9.12%)] and bronchiectasis [Pi*MM (59.30%) Pi*SZ (2.81%); Pi*ZZ (7.02%)]. When COPD/emphysema and bronchiectasis were recorded in the same patient, the rate of Pi* ZZ (14.78%) mutations was even higher. Asthma patients exhibited significantly less deficient genotypes [Pi*MM (54.81%); Pi*SZ (2%); Pi*ZZ (2.77%)] than two other groups. Associated respiratory symptoms confirmed the diagnosis.
Conclusion: COPD/emphysema and bronchiectasis, but not asthma patients, exhibit higher frequency of AATD genotypes. Our data suggest that AATD testing should be offered to patients with COPD/emphysema and bronchiectasis.
Keywords: SERPINA1, alpha-1-antitrypsin deficiency, bronchiectasis, asthma, diagnosis
Introduction
Alpha-1 antitrypsin deficiency (AATD) is an autosomal codominant condition caused by mutations of the SERPINA1 gene characterized by low serum level of AAT.1 Since the discovery of AATD in early 1960s has become apparent that the emphysematous form of chronic obstructive pulmonary disease (COPD) is the most frequent clinical manifestation in individuals with AATD. Other common clinical manifestations of AATD include hepatic diseases, and less frequently panniculitis and other skin diseases.2 Despite of being one of the most common inherited conditions worldwide (AATD occurs in approximately 1:3,000–5,000 people), it remains significantly under-diagnosed. Data show that less than 10% of individuals with AATD identified and with delays of more than 5 years between initial symptoms and diagnosis.3–5 This is also in part related to the fact that many people with AATD are asymptomatic during the life time.
The clinical spectrum of AATD-related lung diseases is variable. AATD pulmonary involvement might include emphysema with variable functional and radiological impairments,6 asthma7 and bronchiectasis.8 In addition, the unusual associations between AATD and idiopathic pulmonary fibrosis have also been reported.9 Therefore, an early detection of AATD is a crucial to define indicator diseases that should prompt physicians to screen for AATD. While according to recent guidelines-all patients with COPD and/or emphysema recommended for AATD screening, the importance of routinely screening of patients with asthma and bronchiectasis remains controversial. This is due to the conflicting epidemiological results concerning the association between AATD and those diseases. Regarding asthma, several investigators have suggested an increased risk of asthma among certain genotypes of AATD whereas others did not find an association.10–13 Nevertheless, few studies suggested that AATD patients with concomitant asthma have a worse prognosis.14,15 The recent ERS Statement of few years ago refer to the WHO recommendation to test all patients with COPD and all patients with adult-onset asthma. Thus also asthma patients (at least those with adult onset) should be tested.16 Likewise, the causal relationship between AATD and bronchiectasis is controversial. Some studies have found a high prevalence of bronchiectasis among AATD patients while others found no association.17–19 Although data document the role of AATD as an underlying etiology of bronchiectasis, the majority of patients are not tested for AATD. It is likely that the estimation of AATD prevalence in bronchiectasis population remains poor. Because of the high prevalence of COPD/emphysema, asthma, and bronchiectasis and the common pathophysiological pathways, some AATD patients with different diseases may present with similar symptoms.20 For example, common pathophysiological features of AATD-related bronchiectasis and emphysema include elevated elastin degradation as an indicator of elevated levels of desmosine and isodesmosine in both diseases.21,22 Considering latter, the investigations for the presence of chronic respiratory conditions, as asthma or bronchiectasis, in AATD are of great clinical importance. Hence, to elucidate the importance of COPD/emphysema, asthma, and bronchiectasis as indicator diseases for AATD, we compared the frequency and distribution of the different AAT alleles in patients with each of those three conditions.
Materials and Methods
Patients and Methods
Between September 2003 and March 2020, 29,465 testing kits (AlphaKit®) were analyzed in the AAT laboratory, University of Marburg, Germany. The diagnosis of AATD was made through a measurement of AAT serum levels, followed by genotyping, phenotyping or whole gene sequencing depending on availability and/or the need for more detailed interpretation of the AAT results.23 Respiratory symptoms were recorded.
Clinical Samples
We used serum samples and dried blood spot (DBS) samples (AlphaKits® GE Healthcare Ltd, Cardiff, CF147YT, UK) for screening and testing for AATD. The AlphaKits® consists of an instruction manual that outlines the purpose of the testing and the procedure how to obtain a blood specimen. Blood is applied to a filter paper, dried and shipped to our laboratory at the University of Marburg for the routine diagnosis of AATD. The AlphaKits® includes a text field for patient and physician’s identification. Clinical characteristics are recorded on the AlphaKit® (acute bronchitis, asthma, bronchiectasis, COPD, dyspnoea on exertion, dyspnea attacks, emphysema, chronic bronchitis, cough, sputum, wheezing), and also the smoking history and substitution therapy for AAT are asked for. The physician’s signature on the AlphaKit® confirms that patients approved and signed informed consent for the samples shipped to our laboratory for genetic analysis. Because our study reflects a retrospective analysis of those routine data, a formal ethics approval for this summary statistics of anonymized data was not necessary.
Nephelometry was used for the semi-quantitative determination of the plasma AAT levels and polymerase chain reaction (PCR) for genotyping, which was eventually followed by isoelectric focusing (IEF) (phenotype) and gene sequencing. Two independent readers validated the results of PCR and IEF. For the sequencing, the DBS samples were shipped to a reference laboratory (Eurofins Genomics Germany GmbH or Progenika Biopharma, S.A. A Grifols Company). Details regarding the laboratory methods have been described before.23,24
Clinical characteristics were recorded on the AlphaKit® (acute bronchitis, asthma, bronchiectasis, COPD, dyspnea on exertion, dyspnea attacks, emphysema, chronic bronchitis, cough, sputum, wheezing) and were documented in a database.
Statistical Analysis
For the comparison of continuous variables Kruskal–Wallis test with Dunn’s test was applied (data were not normally distributed). For the comparison of categorical variables, chi-square test was applied. Microsoft Excel 2010 (Microsoft Corporation, Redmond, Washington, USA), IBM SPSS statistics version 24 (IBM, Armonk, New York, USA) and GraphPad version 7 (GraphPad, San Diego, CA, USA) were used for all calculation, graphs were constructed using Microsoft Excel and BioVenn.25
Results
Study Population
In total 29,465 AlphaKits® were analyzed between September 2003 and March 2020. According to the transferred information, 18,736 patients had been diagnosed with COPD/emphysema, asthma, bronchiectasis or for the combination of these diseases. Further analysis was restricted to this population. Baseline characteristics are presented in Table 1.
 |
Table 1 Baseline Characteristics of Probands |
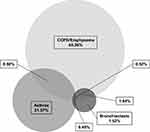
We identified patient having only COPD/Emphysema 12,283 (65.56%), asthma 4,041 (21.57%) or bronchiectasis 285 (1.52%). Additionally, we found 1,592 (8.50%) cases with combined COPD/emphysema and asthma, 345 (1.84%) COPD/emphysema and bronchiectasis, 92 (0.49%) asthma and bronchiectasis, and 98 (0.52%) COPD/emphysema, asthma and bronchiectasis (Figure 1). The baseline characteristics of the respective groups well reflect reports in the literature. Patients with COPD/emphysema were older and smoked more often as compared to patients with asthma or bronchiectasis. Asthmatic patients were younger than in the other two groups (Table 1).
Symptoms
Based on the AlphaKit® recordings, the frequency of clinical symptoms such as dyspnea, dyspnea attacks, cough, phlegm, wheezing, acute bronchitis and chronic bronchitis, supported the recorded diagnosis: dyspnea was most often recorded in COPD/emphysema, wheezing was most often recorded in asthma, and productive cough (cough, phlegm, chronic bronchitis) were the leading symptoms in bronchiectasis (Figure 2).
Distribution of Genotypes
The distribution of the AAT alleles of the 18,736 individuals is illustrated in Figure 3. In total 10,829 (57.80%) Pi*MM, 944 (5.04%) Pi*MS, 4,437 (23.68%) Pi*MZ, 49 (0.26%) Pi*SS, 432 (2.31%) Pi*SZ, 1,432 (7.64%) Pi*ZZ, 253 (1.35%) Pi*M and rare, 47 (0.25%) Pi*S and rare, 268 (1.43%) Pi*Z and rare, 45 (0.24%) Pi*rare and rare have been identified.
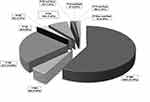 |
Figure 3 Distribution of the AAT alleles. |
The distribution of the AAT alleles among patients with COPD/emphysema or asthma, or bronchiectasis yielded the following results (illustrated in Figure 4 and Table 2): Regarding the distribution of the wild type allele M and the most frequent mutations S (E264V) and Z (E342K), no significant differences could be found between COPD/emphysema [Pi*MM (58.24%); Pi*SZ (2.49%); Pi*ZZ (9.12%)] and bronchiectasis [Pi*MM (59.30%) Pi*SZ (2.81%), Pi*ZZ (7.02%)]. In contrast, asthma patients exhibited significantly less deficient genotypes [Pi*MM (54.81%); Pi*SZ (2%); Pi*ZZ (2.77%)] than two other groups.
 |
Table 2 Distribution of the AAT Alleles Among Patients with COPD/Emphysema or Asthma, or Bronchiectasis |
We also analyzed the distribution of these genotypes in a number of combinations of the three diagnostic groups (Table 3). Adding patients with the diagnostic label COPD/emphysema or bronchiectasis to any other group increases the frequency of Pi*ZZ samples while the addition of the diagnostic label asthma decreases the detection rate.
 |
Table 3 Distribution of AAT Alleles Among Different Combinations of the Three Diagnostic Groups |
In Figure 5 the detection rate is shown over a period of 17 years of normal genotype, intermediate genotype and severe genotype of patients with COPD/emphysema, bronchiectasis, asthma. The genotypes have been grouped in: normal genotype (Pi*MM); intermediate genotype (Pi*MS, Pi*MZ, Pi*M/Rare) and severe genotype (Pi*ZZ, Pi*SS, Pi*SZ, Pi*Z/Rare, Pi*S/Rare, Pi*Rare/Rare). A decline of the detection rate of the normal genotype can be seen in Figure 5. The detection rate of the intermediate genotype however increases. Over the 17 years, the detection rate of the severe genotypes remained unchanged.
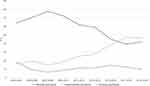 |
Figure 5 Detection rate of patients with COPD/emphysema, bronchiectasis, asthma. |
Ten thousand seven hundred and twenty-nine samples were analyzed out of which none of the three indications (COPD/emphysema, bronchiectasis, asthma) were ticked off on the AlphaKit®. Dividing those samples into a group of samples with at least one symptoms and a second group without symptoms, the symptomatic patients exhibited a lower percentage of at least one mutation (43.44% vs 56.83%) and also a lower percentage of Pi*ZZ samples (4.87% vs 6.37%). We assume that the AlphaKits® have not been ticked off correctly. For this reason, we omitted further analyses of those samples.
Discussion
In our database of almost 30,000 samples, which had been tested for AATD for different reasons, we analyzed the distribution of three important respiratory diseases, namely COPD/emphysema, asthma, and bronchiectasis. Furthermore, we described the distribution of different AAT genotypes in this cohort. To the best of our knowledge, this is one of the largest cohorts comparing the distribution of AAT genotypes among different respiratory diseases. We found COPD/emphysema to be the most frequent reason for testing, followed by asthma and bronchiectasis. Remarkably, COPD/emphysema and bronchiectasis exhibited very similar distribution of the AAT genotypes. Both diseases exhibited higher percentages of severe deficient AAT genotypes as compared to asthma.
The COPD/emphysema was by far the most prevalent disease entity in our study population (65.56%), followed by asthma (21.57%) and bronchiectasis (1.52%). This is likely relates to the facts that: i) early onset emphysema known as a typical manifestation of AATD26 and ii) COPD is a highly prevalent internationally and nationally.27–29 The bronchiectasis is gaining importance and awareness, however, it still remains a rare and underdiagnosed disease. Therefore, the low prevalence of samples in which bronchiectasis was the reason for testing, was expected.30,31 Furthermore, our analysis records 2.78% of all 29,465 subjects to be bronchiectatic (out of which 0.97% with bronchiectasis and absence of asthma or COPD/emphysema), and is in line with what has been reported by the NHLBI registry (2% of 1,129 participants).
By analyzing the association between recorded symptoms and the leading diagnosis, we gained confirming findings. While in COPD/emphysema was most often recorded dyspnea, wheezing was most often in asthma, and productive cough (cough, phlegm, chronic bronchitis) was most often in bronchiectasis. The combination of symptoms and the main diagnosis made us confident that the reported diagnoses were correct, even though lung function data and/or CT data are not part of the information that is transferred with the AlphaKit®.
Most interesting in our analysis is that we found a similar distribution of AAT genotypes between bronchiectasis and COPD/emphysema. The Pi*ZZ genotype was found significantly more often in patients with COPD/emphysema or bronchiectasis (9.12% in COPD/emphysema, 7.02% in bronchiectasis) than in patients with asthma (2.77%). The literature on AAT genotypes in patients with bronchiectasis is scarce. In a case-control study of 2000, Cuvelier and colleagues recorded no difference in the distribution of AAT alleles between bronchiectatic patients and 1,030 control subjects (unrelated healthy blood donors).19 Very recently, investigators from two hospitals in the UK screened 1600 patients with bronchiectasis, which resulted in the detection of only eight individuals (0.5%) with AATD. The authors concluded that routine screening for AATD in bronchiectasis in the UK has a low rate of detection.32 One can agree that 0.5% is certainly a low number; however, it is in the same range as the percentage of AATD patients within the overall COPD population, in which screening for AATD is accepted.27,33 Furthermore, these numbers come from rather unselected disease populations, while our results are from a pre-filtered population. Nevertheless, it is reassuring that in our as well as in UK study the frequency of severe AATD in bronchiectasis was comparable to that in COPD.
The recommendation of the WHO, the ERS and the ATS about the need to test all COPD patients (and all patients with adult-onset asthma) have been emphasized repeatedly. Despite this, the recommendation is clearly not followed by any health-care system throughout the world. One could argue that adding bronchiectasis as another rare (or believed to be rare) condition to the reasons for AATD screening could “dilute” the message of testing for AATD in routine screening. In our opinion, the recommendations depend on the clinical setting: While COPD should be a reason for AATD screening in every clinical setting, screening for AATD in bronchiectasis should be implemented in the workup of bronchiectasis patients in specialist centers.
One could argue that COPD and emphysema we need to analyz separately. In a subgroup analysis, we looked at the symptom and genotype distribution in patients with “COPD only” patients and compared them to “emphysema only”. In general, COPD patients were more symptomatic (supplement Figure 1) while emphysema patients more often exhibited a genotype compatible with severe deficiency (supplement Figure 2), both confirming earlier findings.26,34
Discussing the limitations of our analysis, we have to acknowledge that targeting preselected individuals (which is the basis for the vast majority of our analyses) might result in missing asymptomatic subjects with severe AATD, because a significant proportion of severe AATD patients do not develop pulmonary diseases.35,36 Secondly, our laboratory population only reflects a small and preselected part of the overall populations of the three diseases that we looked at. Thirdly, the retrospective nature of our analysis resulted in a high number of samples in which the reason for the analysis was not recorded. The reasons for that remain speculative. Finally, only limited information about the clinical characteristics was available, and the diagnostic accuracy of the disease entity remains unknown. Nevertheless, our analysis provides important insights into the distribution of ATTD among diseases, which are regularly screened for AAT genotypes.
Overall, in our population the COPD/emphysema and bronchiectasis exhibited very similar distributions of AAT genotypes. Hence, screening of patients with bronchiectasis for the presence of AATD is of importance.
Abbreviations
AAT, alpha 1 antitrypsin; AATD, alpha 1 antitrypsin deficiency; COPD, chronic obstructive pulmonary disease; DBS, dried blood spot; IEF, isoelectric focussing; PCR, polymerase chain reaction.
Ethics Approval and Informed Consent
Because our study reflects a retrospective analysis of those routine data, an ethics approval is not necessary.
Acknowledgments
We thank all employees of the alpha-1 antitrypsin laboratory at the University of Marburg for their continuous effort they put into this project. The alpha-1 antitrypsin laboratory at the University of Marburg has been supported by Grifols and Progenika Biopharma (A Grifols Company).
Disclosure
Martina Veith reports grants from Grifols. Prof. Dr. Robert Bals reports grants from BMBF, during the conduct of the study; grants from Schwiete Stiftung, Novartis, and Mukoviszidose e.V. and personal fees from AstraZeneca and CSL Behring, outside the submitted work. Prof. Dr. Claus Franz Vogelmeier reports grants, personal fees from AstraZeneca, Boehringer Ingelheim, Grifols, GlaxoSmithKline, and Novartis; personal fees from CSL Behring, Chiesi, Menarini, Nuvaira, MedUpdate, outside the submitted work. Dr Timm Greulich reports grants from Grifols, during the conduct of the study; personal fees from AstraZeneca, serves as a lecturer and part of the advisory board for Berlin Chemie, Boehringer Ingelheim, Chiesi, CSL Behring, Grifols, GSK, Novartis, received grants from German Centre for Lung Research, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Janciauskiene SM, Bals R, Koczulla R, Vogelmeier C, Kohnlein T, Welte T. The discovery of alpha1-antitrypsin and its role in health and disease. Respir Med. 2011;105(8):1129–1139.
2. European RS, American Thoracic Society. American thoracic society/European respiratory society statement: standards for the diagnosis and management of individuals with alpha-1 antitrypsin deficiency. Am J Respir Crit Care Med. 2003;168(7):818–900.
3. Brantly ML, Paul LD, Miller BH, Falk RT, Wu M, Crystal RG. Clinical features and history of the destructive lung disease associated with alpha-1-antitrypsin deficiency of adults with pulmonary symptoms. Am Rev Respir Dis. 1988;138(2):327–336. doi:10.1164/ajrccm/138.2.327
4. Stoller JK, Brantly M. The challenge of detecting alpha-1 antitrypsin deficiency. Copd. 2013;10(Suppl 1):26–34.
5. Stoller JK, Smith P, Yang P, Spray J. Physical and social impact of alpha 1-antitrypsin deficiency: results of a survey. Cleve Clin J Med. 1994;61(6):461–467. doi:10.3949/ccjm.61.6.461
6. Silverman EK, Sandhaus RA. Alpha1-antitrypsin deficiency. N Engl J Med. 2009;360(26):2749–2757. doi:10.1056/NEJMcp0900449
7. Siri D, Farah H, Hogarth DK. Distinguishing alpha1-antitrypsin deficiency from asthma. Ann Allergy Asthma Immunol. 2013;111(6):458–464.
8. Stockley RA. The multiple facets of alpha-1-antitrypsin. Ann Transl Med. 2015;3(10):130.
9. Cottin V, Nunes H, Brillet PY, et al. Combined pulmonary fibrosis and emphysema: a distinct underrecognised entity. Eur Respir J. 2005;26(4):586–593. doi:10.1183/09031936.05.00021005
10. Eden E. Asthma and COPD in alpha-1 antitrypsin deficiency. Evidence for the Dutch hypothesis. COPD. 2010;7(5):366–374. doi:10.3109/15412555.2010.510159
11. McGee D, Schwarz L, McClure R, et al. Is PiSS alpha-1 antitrypsin deficiency associated with disease? Pulm Med. 2010;2010:570679. doi:10.1155/2010/570679
12. van Veen IH, Ten Brinke A, van der Linden AC, Rabe KF, Bel EH. Deficient alpha-1-antitrypsin phenotypes and persistent airflow limitation in severe asthma. Respir Med. 2006;100(9):1534–1539.
13. Davila I, Valero A, Entrenas LM, Valveny N, Herraez L. Relationship between serum total IgE and disease severity in patients with allergic asthma in Spain. J Investig Allergol Clin Immunol. 2015;25(2):120–127.
14. Demeo DL, Sandhaus RA, Barker AF, et al. Determinants of airflow obstruction in severe alpha-1-antitrypsin deficiency. Thorax. 2007;62(9):806–813. doi:10.1136/thx.2006.075846
15. Dowson LJ, Guest PJ, Stockley RA. Longitudinal changes in physiological, radiological, and health status measurements in alpha(1)-antitrypsin deficiency and factors associated with decline. Am J Respir Crit Care Med. 2001;164(10 Pt 1):1805–1809. doi:10.1164/ajrccm.164.10.2106036
16. Miravitlles M, Dirksen A, Ferrarotti I, et al. European respiratory society statement: diagnosis and treatment of pulmonary disease in α1-antitrypsin deficiency. Eur Respir J. 2017;50(5):1700610. doi:10.1183/13993003.00610-2017
17. Parr DG, Guest PG, Reynolds JH, Dowson LJ, Stockley RA. Prevalence and impact of bronchiectasis in alpha1-antitrypsin deficiency. Am J Respir Crit Care Med. 2007;176(12):1215–1221.
18. Guest PJ, Hansell DM. High resolution computed tomography (HRCT) in emphysema associated with alpha-1-antitrypsin deficiency. Clin Radiol. 1992;45(4):260–266. doi:10.1016/S0009-9260(05)80011-X
19. Cuvelier A, Muir JF, Hellot MF, et al. Distribution of α1-antitrypsin alleles in patients with bronchiectasis. Chest. 2000;117(2):415–419. doi:10.1378/chest.117.2.415
20. Barnes PJ. Immunology of asthma and chronic obstructive pulmonary disease. Nat Rev Immunol. 2008;8(3):183–192. doi:10.1038/nri2254
21. Chalmers JD, Moffitt KL, Suarez-Cuartin G, et al. Neutrophil elastase activity is associated with exacerbations and lung function decline in bronchiectasis. Am J Respir Crit Care Med. 2017;195(10):1384–1393. doi:10.1164/rccm.201605-1027OC
22. Turino GM, Ma S, Cantor JO, Lin YY. Biomarkers in alpha-1 antitrypsin deficiency chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2016;13(Suppl 4):S336–340. doi:10.1513/AnnalsATS.201509-574KV
23. Greulich T, Nell C, Herr C, et al. Results from a large targeted screening program for alpha-1-antitrypsin deficiency: 2003–2015. Orphanet J Rare Dis. 2016;11(1):75. doi:10.1186/s13023-016-0453-8
24. Veith M, Klemmer A, Anton I, et al. Diagnosing alpha-1-antitrypsin deficiency using A PCR/luminescence-based technology. Int J Chron Obstruct Pulmon Dis. 2019;14:2535–2542. doi:10.2147/COPD.S224221
25. Hulsen T, de Vlieg J, Alkema W. BioVenn – a web application for the comparison and visualization of biological lists using area-proportional Venn diagrams. BMC Genomics. 2008;9(1):488. doi:10.1186/1471-2164-9-488
26. Strnad P, McElvaney NG, Lomas DA. Alpha1-antitrypsin deficiency. N Engl J Med. 2020;382(15):1443–1455. doi:10.1056/NEJMra1910234
27. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Am J Respir Crit Care Med. 2017;195:557–582.
28. Geldmacher H, Biller H, Herbst A, et al. [The prevalence of chronic obstructive pulmonary disease (COPD) in Germany. Results of the BOLD study]. Dtsch Med Wochenschr. 2008;133(50):2609–2614. doi:10.1055/s-0028-1105858
29. Buist AS, McBurnie MA, Vollmer WM, et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007;370(9589):741–750. doi:10.1016/S0140-6736(07)61377-4
30. Ringshausen FC, de Roux A, Diel R, Hohmann D, Welte T, Rademacher J. Bronchiectasis in Germany: a population-based estimation of disease prevalence. Eur Respir J. 2015;46(6):1805–1807. doi:10.1183/13993003.00954-2015
31. Chalmers JD, Aliberti S, Polverino E, et al. The EMBARC European bronchiectasis registry: protocol for an international observational study. ERJ Open Res. 2016;2(1):00081–2015. doi:10.1183/23120541.00081-2015
32. Carreto L, Morrison M, Donovan J, et al. Utility of routine screening for alpha-1 antitrypsin deficiency in patients with bronchiectasis. Thorax. 2020. doi:10.1136/thoraxjnl-2019-214195
33. Rahaghi FF, Sandhaus RA, Brantly ML, et al. The prevalence of alpha-1 antitrypsin deficiency among patients found to have airflow obstruction. COPD. 2012;9(4):352–358. doi:10.3109/15412555.2012.669433
34. Chai CS, Liam CK, Pang YK, et al. Clinical phenotypes of COPD and health-related quality of life: a cross-sectional study. Int J Chron Obstruct Pulmon Dis. 2019;14:565–573. doi:10.2147/COPD.S196109
35. Eriksson S. A 30-year perspective on α1-antitrypsin deficiency. Chest. 1996;110(6 Suppl):237S–242S. doi:10.1378/chest.110.6_Supplement.237S
36. Parr DG, Stoel BC, Stolk J, Stockley RA. Pattern of emphysema distribution in α1-antitrypsin deficiency influences lung function impairment. Am J Respir Crit Care Med. 2004;170(11):1172–1178. doi:10.1164/rccm.200406-761OC
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.