Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
The Dermoscopic Features of Photoaging and Its Association with Sun Index Score in the Coastal Population at Cilincing, Jakarta: A Cross-Sectional Study
Authors Respati RA, Yusharyahya SN , Wibawa LP , Widaty S
Received 10 January 2022
Accepted for publication 21 April 2022
Published 25 May 2022 Volume 2022:15 Pages 939—946
DOI https://doi.org/10.2147/CCID.S355260
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Riris Asti Respati, Shannaz Nadia Yusharyahya, Larisa Paramitha Wibawa, Sandra Widaty
Department of Dermatology and Venereology, Faculty of Medicine Universitas Indonesia – Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia
Correspondence: Shannaz Nadia Yusharyahya, Department of Dermatology and Venereology, Faculty of Medicine Universitas Indonesia – Dr. Cipto Mangunkusumo Hospital, 71 Diponegoro, Jakarta, Indonesia, 10430, Tel +62 131935383, Email [email protected]
Purpose: Repeated exposure to ultraviolet light is the most significant factor that contributes to photoaging. Dermoscopy photoaging scale (DPAS) is a noninvasive examination utilized for the diagnosis of photoaging. However, there has been no study analyzing the correlation between DPAS and sun index. Hence, this study aims to find out the dermoscopic features of photoaging and its association with sun index score in the coastal population.
Patients and Methods: This was a descriptive cross-sectional study on individuals living in Cilincing, a coastal area, at North Jakarta. Healthy male or female subjects aged over 18 years old with sun exposure equal or more than 2 hours daily were recruited consecutively. History taking was performed to document the sociodemographic characteristics (age, gender, skin type, smoking habit) and sun index score. Physical examination and dermoscopic examination were conducted to determine DPAS score. Associations of DPAS and photoaging profiles were analyzed with Chi-squared test while correlation between DPAS score and sun index was analyzed with Pearson correlation test.
Results: A total of 100 subjects were included in this study. The median DPAS of the subjects was 9 (1– 21). Right cheek had the highest median DPAS of 3 (0– 6), followed by the left cheek with median DPAS of 3 (0– 7). Men had a higher median DPAS score than women (9 vs 8). There was a significant difference between DPAS score and age (p< 0.001). There was no significant correlation between DPAS score and sun index (r = − 0.005; p = 0.957).
Conclusion: Factors associated with high DPAS score were cheek predilection, male, actively smoking, Fitzpatrick skin type IV, and increasing age. DPAS score has no correlation with sun index.
Keywords: dermoscopy, photoaging, sun index, coastal area
Introduction
Extrinsic aging is induced primarily by chronic ultraviolet (UV) exposure, which is also known as photoaging.1 Photoaging is marked by an acceleration in the appearance of coarse wrinkling, mottled pigmentation, lentigines, telangiectasis, and precancerous lesions.2 The first qualitative assessment scale for skin photoaging was based on the clinical judgment, developed by Glogau. This scale was classified into four categories, namely type I, II, III, and IV.3,4 There is no literature on the validity and reliability of the Glogau scale, especially in skin of color population.
Along with the evolving era of medical technology, a study using the dermoscopy photoaging scale (DPAS) as a photoaging evaluation instrument using a dermoscopy was conducted in Istanbul in 2013 with the majority of subjects having Fitzpatrick skin type II and III. The score is calculated based on specific dermoscopic findings in 4 facial areas ie, forehead, chin, and both cheeks which are then summed up to a maximum score of 44.5 Evaluation with a dermoscopy as a simple and non-invasive diagnostic tool can give more precise results compared to clinical assessment.5,6 DPAS assessment is easy-to-use, quick, and can be used in a variety of circumstances.5.
The frequency, length, and intensity of sun exposure are all factors that might accelerate the aging process caused by UV radiation.7 Individuals who live in an area with great sun exposure (eg, coastal area) are more susceptible to photoaging.8,9 Other influencing factors of photoaging are age, sex, and smoking habits. In addition, smoking disrupts skin’s ability to regenerate and accelerates skin aging.10,11
Cilincing district is a coastal area in the North Jakarta Administrative City. Based on the population employment data of DKI Jakarta Province in 2018, there were 2999 people (30%) of the population working as fishermen in this District, which are considered to be at high risk of photoaging.12 The residents in this area are mostly have Fitzpatrick skin type III–IV. To date, there has been no study regarding photoaging in the population living at a coastal area. As this unique population is prone to photoaging, the factors associated with photoaging should be further addressed. In addition, there has been no study on the correlation between DPAS and sun index score. Therefore, this study aims to analyze the dermoscopic features of photoaging and its association with sun index score in the coastal population.
Materials and Methods
This was a descriptive cross-sectional study. The study was conducted at the Cilincing District Health Center, North Jakarta Administrative City, DKI Jakarta in November 2020. This study was conducted in accordance with the Declaration of Helsinki. This study was approved by the ethics committee of Faculty of Medicine Universitas Indonesia. Subjects were asked for informed consent prior to the study.
The sample size was calculated based on sample size estimation for correlation study with power 80% and accuracy 95%. The estimation of sample size was 100 subjects. Subjects were recruited consecutively according to inclusion and exclusion criteria.
Inclusion criteria included healthy male or female subjects with age ≥ 18 years who live in coastal areas with minimal average duration of sun exposure of 2 hours per day. Exclusion criteria were subjects with genodermatoses; received drugs known to affect skin aging or dyschromia (eg, topical and systemic retinoids or steroids, topical or systemic antiaging pharmaceuticals, such as topical vitamin C preparations or systemic hormone replacement therapy); had undergone any medical aesthetic procedures (eg, chemical peeling, botulinum toxic injection, dermal fillers, laser resurfacing, electrosurgery, etc.) at least 1 year prior to the study entry; taking drugs with photosensitizing effects such as non-steroidal anti-inflammatory drugs, diuretics, sulfonylurea, antibiotics (eg tetracycline, doxycycline, sulfonamide), antifungal agents (eg, itraconazole); and had a drug-induced photosensitivity reaction in the past 3 months prior to the study.
History taking was performed to collect the data: age, gender, occupation, smoking habits, sunburn history, amount of sun exposure on weekdays and weekends, type of clothing on weekdays and weekends to calculate the sun index.13,14 All subjects were photo-documented in 3 positions (front view, lateral 45° right, and lateral 45° left) with a digital camera Fujifilm X-T10 (Fujifilm, Japan). The face was divided into 4 areas, namely the forehead, right cheek, left cheek, and chin. Each area was examined using Heine Delta 20 Dermoscopy (Heine Optotechnic, Germany) to calculate the DPAS score according to the criteria by Isik et al. These criteria included yellowish discoloration, yellowish papules, white linear scarring areas, hypo-hyperpigmented macules, solar lentigo, telangiectasia, actinic keratosis, senile comedones, superficial wrinkles, deep wrinkles, and criss-cross wrinkles. The final DPAS score were assessed by calculating scores from 4 facial areas. The evaluation was made by the yes (1 point) or no (0 point) policy. For example, if the criterion was positive on one facial region and negative on the remaining areas that means the sum is 1 point for the criterion.5,15
Data were presented in narratives, tables, and graphs. Statistical analysis was performed using Statistical Package for Social Science (SPSS) version 20.0. Numerical data were expressed as mean ± standard deviation (SD) or median (minimum – maximum value) depending on the data distribution, while categorical data were expressed as frequency and percentage. Association between influencing factors and photoaging were analyzed with Chi-square test. Pearson correlation test was used to analyze correlation between DPAS and sun index, duration of sun exposure, as well as age P-value < 0.05 was considered significant.
Results
A total of 100 subjects were included in this study. Sociodemographic characteristics of the subjects are listed in Table 1. The median fraction of body surface area (BSA) exposed to sunlight was 21% (7% – 60%). The median sun exposure per week was 50.75 hours (11–91 hours). The median sun index was 6.22 (0.98–54.60). Proportion of dermoscopic features based on gender, smoking habits, and Fitzpatrick skin phototype in Cilincing District, North Jakarta in 2020 are listed in Table 2–4.
 |
Table 1 Sociodemographic Characteristics of Subjects |
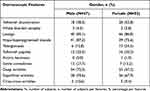 |
Table 2 Proportion of Dermoscopic Features Based on Gender |
 |
Table 3 Proportion of Dermoscopic Features Based on Smoking Habits |
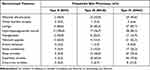 |
Table 4 Proportion of Dermoscopic Features Based on Fitzpatrick Skin Phototype |
The mean DPAS score increased with age. The mean total DPAS scores among the age groups of 18–29 years, 30–39 years, 40–49 years, 50–59 years, and ≥ 60 years were 5; 7; 9.5; 13; and 16, respectively. In women aged 30–39 years, lentigo was the most common finding, followed by superficial wrinkles and hypo-hyperpigmented macules. It was also found that there was an increase in the proportion of deep wrinkles (21.4% vs 85.7%), superficial wrinkles (71.4% vs 100%), and criss-cross wrinkles (0% vs 57.1%) in the age group of 30–39 years and ≥ 60 years, respectively. In men aged 30–39 years up to the age group of ≥ 60 years, lentigo and hypo-hyperpigmented macules were the most common DPAS findings, but in the age groups of 50–59 years and ≥ 60 years, deep wrinkles (100%) and superficial wrinkles (100%) were also frequent. The DPAS criteria are shown in Figure 1.
The highest mean total DPAS score was identified in the active smoker group (11), compared to the former smoker group (9.5), passive smoker group (7), and non-smoker group (8). There was an increase in the mean total DPAS score parallel with the increase in Fitzpatrick skin type, which was 6, 7, and 10 in group Fitzpatrick skin type II, III, and IV, respectively. The median total DPAS score of active male smoker group was higher than that of the active female smoker group (13 vs 10).
Within the group with high intensity sun exposure, the median total DPAS score in male subjects was greater than that in female subjects (9 vs 7). Both male and female subjects with Fitzpatrick skin type IV had the highest median total DPAS scores, which were 10 (3–19) and 13 (2–12). The median total DPAS scores in the Fitzpatrick skin type IV group was higher than the Fitzpatrick skin type III group both in low, medium, and high intensity sun exposure.
The DPAS score was significantly associated with age (p < 0.001) with a very strong positive correlation (r = 0.780), indicating that older subjects had higher DPAS scores. There was no significant association between sex (p = 0.711) and smoking habits (p = 0.411) with photoaging appearance based on DPAS. There was a significant association between Fitzpatrick’s skin type and DPAS. The higher the Fitzpatrick skin type, the higher the DPAS score (p < 0.001). However, DPAS score was not associated with the sun index (p = 0.957) with a very weak negative correlation (r = −0.005). The DPAS score was also not associated with the total duration of sun exposure (p = 0.345), with a very weak negative correlation (r = −0.095).
Discussion
The most common Fitzpatrick skin type among the subjects was type IV (65%), with hypo-hyperpigmented macules (89.2%) being the most common dermoscopic feature. These results were different from study by Isik et al which found type III as the most common Fitzpatrick skin type (47%) with solar lentigo being the most common dermoscopic feature. This might be due to differences in ethnicity and skin type in most of the subjects.5 Another study by El-Sayed et al in Egypt reported that most of their subjects have the Fitzpatrick skin type III, IV, and V, but there was no information about the proportion.15
The median sun index was 6.22. This is six times higher compared to another study conducted in Indonesia in 2019.13 Another study conducted in Malaysian urban and rural populations by Nurbazlin et al reported a lower median value of sun index compared to this study. The difference might be due to the fact that the coastal population is more intensely exposed to sunlight than the urban population.14 The median BSA exposed to the sun in this study is similar to that in Malaysian urban populations. However, the median BSA is lower in Malaysian rural populations.
The median total DPAS score was 9. It was highest on the right and left cheeks, followed by the forehead and chin. Similar results were also reported in a study by Magdy et al, in which cheek had that the highest score followed by the forehead and chin. This finding was presumably caused by use of head scarf by most subjects.3
There has been no research on the DPAS profile mapping for each facial region.1,5,8 A study in Medan, Indonesia with similar skin type, revealed that yellowish discoloration, lentigo, and superficial wrinkles were the most common DPAS finding on the facial skin.16 Our observation found lentigo (76%) was the most common DPAS finding on the right and left cheeks. Hypo-hyperpigmented macules were the most common finding on the chin. However, deep wrinkles were the least common finding on the chin (23%) compared to the forehead, right cheek, and left cheek (47%). This finding might be due to the fact that facial wrinkles usually begin on the area around the eyes, followed by the forehead, and finally on the chin, in accordance with the aging process.11
There was no significant association between gender and photoaging findings based on DPAS. Several factors were considered to have an impact in this study, including those men who were far more likely to be active smokers or have a history of active smoking. In addition, men experienced more severe sun exposure. El-Sayed et al reported that DPAS characteristics were more common in men compared to women within the same age group. It was suspected that the propensity of men to smoke more, spend more time outdoor, and thus are more likely to be exposed to the sun; and the tendency of women to use sunscreen when doing outdoors activities, contributed to such findings.15
In this study, the hypo-hyperpigmented macules, deep wrinkles, superficial wrinkles, and criss-cross wrinkles were more common in male subjects. In contrast, Chung et al found that hyperpigmented macules were more common in women.17 These difference findings were thought to be caused by higher sun exposure in our male subjects. In addition, the median DPAS score in male active smokers was higher than that in female active smokers.
DPAS scores had a very strong positive correlation with age. This shows that the older the age, the higher the DPAS score, and this association was statistically significant. A study by El-Sayed et al in Egypt reported that a higher mean DPAS score was found in people aged older than 60 years compared to those under 60 years.15 This is supported by Isik et al that reported significant changes in photoaging based on DPAS score at the fifth decade of life.5
In women aged 30–39 years, lentigo was the most common DPAS finding followed by superficial wrinkles and hypo-hyperpigmented macules. A similar result was found in a study by El-Sayed et al, which reported that lentigo, superficial wrinkles, and hypo-hyperpigmented macules were also the three most common DPAS findings.15 This result is in accordance with references stating that most people with skin of color (Fitzpatrick skin type III and IV) living in coastal area tend to have earlier and more rapid pigmentation changes (dyschromia) since the most common forms of photoaging in skin of color are lentigo and mottled pigmentation.18,19
In men aged 30–39 years up to ≥ 60 years, lentigo and hypo-hyperpigmented macules were the most common findings; however, in the age groups of 50–59 years and ≥ 60 years, deep wrinkles and superficial wrinkles were also frequent. This is thought to be caused by the role of melanin as a determining factor for skin color. Overall, the subjects in this study were skin of color population with larger melanosome size and have more melanin than lighter skin. Melanin produced by melanocytes can absorb UV radiation; therefore, reducing its penetration into deeper dermis and connective tissue. This process occurs more intensely in skin of color. Therefore, the manifestations of photoaging on this population tend to be preceded by changes in pigmentation. However, the number of melanocytes decreases by 20% every decade after the age of 30 years. This condition may influence dermoscopic findings at the later age.20
The highest DPAS score was found in the active smoker group, despite no significant association. In contrast to our study, El-Sayed et al reported statistically significant higher DPAS scores in the active smoker group.15 In this study, deep wrinkles, superficial wrinkles, and criss-cross wrinkles were more common in the active smoker and former smoker groups. Chung et al reported a significant association between the higher number of cigarettes consumed and more wrinkles.17 Similar results were also reported by another study by Yin et al in Japan. The study reported that individuals who smoked > 35 packs per year had a 7.8 times higher risk to develop more severe wrinkles than individuals who had never smoked.21
There was a significant association between Fitzpatrick skin type III and IV with DPAS. The higher the Fitzpatrick skin type, the higher the DPAS score. These results are different from previous studies. The difference in this study is thought to be caused by the higher median total DPAS score in the Fitzpatrick skin type IV group with lower intensity of sun exposure compared to the Fitzpatrick skin type III group.
The DPAS score was not correlated with the sun index and hours of sun exposure. With sole consideration of photoaging, we hypothesize that the DPAS score is implicated in both chronological aging and photoaging, but future studies are recommended. There was no correlation between the DPAS score and the sun index, which presumably occurred regarding the limitations of this study. The DPAS score was assessed only on the facial region, while the sun index is supposed to be calculated based on the BSA of the entire body parts exposed to the sun. In addition, the sun index questionnaire was completed based on the subjects’ habits during the previous week, while the photoaging process occurred due to structural and functional skin changes since the fourth decade of life.15 We did not find any previous studies on the association between the sun index and DPAS score. A particularly important feature of this study was the sun index is considered a reliable and feasible method for measuring sun exposure;14 thus, it was used in this study. The sun index calculates sun exposure based on hours and is not categorized into scores like in the Sun Exposure Score questionnaire. In addition, the sun index collects more detailed data than the Sun Exposure Score, such as the type of activity, use of sunscreen, and the use of other personal protective equipment such as umbrellas.14,22 Objective measurement of sun exposure can be performed using a dosimeter, an electronic device worn on the wrist for a period of time. However, it is not suitable and feasible in this facial aging study.23
The limitation of this study was no analysis on the association between dermoscopic findings and the factors associated with photoaging. In addition, this study did not analyze the clinical classification of photoaging. This study results only applied for populations living in coastal area; hence, future study should be performed in other populations to generalize the findings. Furthermore, future studies which analyze the photoaging profile based on instrument, such as Glogau scale, and its factors in skin of color are warranted.
Conclusion
Factors associated with high DPAS score were cheek predilection, male, actively smoking, Fitzpatrick skin type IV, and increasing age. DPAS score has no correlation with sun index.
Acknowledgment
This research has been funded by PUTI Q3 2020 Universitas Indonesia Grant, Contract Number NKB-1890/UN2.RST/HKP.05.00/2020.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. Kerns ML, Chien AL, Kang S. Skin aging. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, editors. Fitzpatrick’s Dermatology.
2. Yusharyahya SN. Mekanisme penuaan kulit sebagai dasar pencegahan dan pengobatan kulit menua [Skin aging mechanism as a basic prevention and treatment of skin aging]. eJKI Jakarta. 2021;1:150–159. Indonesian.
3. Magdy R, Sadek A. Dermoscopic findings of photo-ageing in Egyptian patients. Egypt Dermatol Online J. 2015;11(1):1–7.
4. Glogau RG. Aesthetic and anatomic analysis of the aging skin. Semin Cutan Med Surg. 1996;15(3):134–138.
5. Isik B, Gurel MS, Erdemir AT, Kesmezacar O. Development of skin aging scale by using dermoscopy. Skin Res Technol. 2013;19(2):69–74.
6. Hu SC, Yu HS. Dermoscopic assessment of xerosis severity, pigmentation pattern and vascular morphology in subjects with physiological aging and photoaging. Eur J Dermatol. 2019;29(3):274–280.
7. Taylor SC. Photoaging and pigmentary changes of the skin. In: Burgess CM, editor. Cosmetic Dermatology. Berlin: Springer; 2005:29–51.
8. Helfrich YR, Sachs DL, Voorhees JJ. Overview of skin aging and photoaging. Dermatol Nurs. 2008;20(3):177–183.
9. Chung JH, Hanft VN, Kang S. Aging and photoaging. J Am Acad Dermatol. 2003;49(4):690–697.
10. Vashi NA, Maymone MB, Kundu RV. Aging differences in ethnic skin. J Clin Aesthet Dermatol. 2016;9(1):3–8.
11. Mesa-Arango AC, Florez-Munoz SV. Mechanism of skin aging. Latreia. 2017;30(2):160–170.
12. Jakarta Open Data [homepage on the Internet]. DKI Jakarta Population Data; 2018. Available from: https://data.jakarta.go.id/dataset.
13. Putri AK, Bramono K, Wibawa LP. Correlation of Serum Levels of 25-Hydroxyvitamin D and Sun Index (Sun Exposure Index) with the Number and Size of Seborrheic Keratosis Lesions on the Face at Dermatology and Venereology Polyclinic, Dr. Cipto Mangunkusumo [Thesis]. Jakarta: Universitas Indonesia; 2019. Indonesian.
14. Nurbazlin M, Chee WS, Rokiah P, et al. Effects of sun exposure on 25(OH) vitamin D concentration in urban and rural women in Malaysia. Asia Pac J Clin Nutr. 2013;22(3):391–399.
15. El-Sayed MH, Saleh HM, El Zawahry KMA, Mostafa AE. The dermoscopic features of facial aging among Egyptians: a comparative study between males and females. J Cosmet Dermatol. 2019;1:1–11.
16. Muslim M, Jusuf NK, Putra IB. Dermoscopic Features of Facial Aging Among Diverse Ethnicity in Medan [Thesis]. Medan: University of Sumatera Utara; 2021. Indonesian.
17. Chung JH, Youn SH, Park BJ, et al. Cutaneous photodamage in Koreans influence of sex, sun exposure, smoking, and skin color. Arch Dermatol. 2001;137(8):1043–1051.
18. Knaggs H. Skin aging in the Asian population. In: Dayan N, editor. Skin Aging Handbook.
19. Lym CI, Azeveo CM, Cohen S, Cunha MG. Characteristics of asian skin–revision. J Dermatol Cosmetol. 2018;2(6):121–133.
20. Ling LC. Aging in Asian Skin. In: Farage MA, Miller KW, Maibach HI, editors. Textbook of Aging Skin.
21. Yin L, Morita A, Tsuji T. Skin aging induced by ultraviolet exposure and tobacco smoking- evidence from epidemiological and molecular studies. Photodermatol Photoimmunol Photomed. 2001;17(4):178–183.
22. Barger-Lux MJ, Heaney RP. Effects of above average summer sun exposure on serum 25-hydroxyvitamin D and calcium absorption. J Clin Endocrinol Metab. 2002;87(11):4952–4956.
23. Holm-Schou AS, Philipsen PA, Idorn LW, Thieden E, Wulf HC. Lifetime UVR dose and skin cancer risk, determined by their common relation to solar lentigo. Anticancer Res. 2020;40(1):557–564.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

