Back to Journals » Clinical Ophthalmology » Volume 16
The Cost-Effectiveness of a Telemedicine Screening Program for Diabetic Retinopathy in New York City
Authors Muqri H, Shrivastava A, Muhtadi R, Chuck RS, Mian UK
Received 10 January 2022
Accepted for publication 11 April 2022
Published 17 May 2022 Volume 2022:16 Pages 1505—1512
DOI https://doi.org/10.2147/OPTH.S357766
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Hasan Muqri,1 Anurag Shrivastava,2 Rakin Muhtadi,2 Roy S Chuck,2 Umar K Mian2
1Department of Ophthalmology, The University of Texas Health Sciences Center at Houston, Houston, TX, USA; 2Department of Ophthalmology and Visual Sciences, Montefiore Medical Center, Bronx, NY, USA
Correspondence: Umar K Mian, Department of Ophthalmology and Visual Sciences, Montefiore Medical Center, 3332 Rochambeau Avenue, Bronx, NY, 10467, USA, Tel +1 718-920-2020, Fax +1 718-920-4791, Email [email protected]
Background: A telemedicine screening initiative was implemented by the Montefiore Health System to improve access to eyecare for a multi-ethnic, at-risk population of diabetic patients in a largely underserved urban community in the Bronx, New York. This retrospective, cross-sectional analysis evaluates the societal benefit and financial sustainability of this program by analyzing both cost and revenue generation based on current standard Medicare reimbursement rates.
Methods: Non-mydriatic fundus cameras were placed in collaboration with a vendor in eight outpatient primary care sites throughout the Montefiore Health Care System, and data was collected between June 2014 and July 2016. Fundus photos were electronically transmitted to a central reading center to be systematically reviewed and coded by faculty ophthalmologists, and patients were subsequently scheduled for ophthalmic evaluation based upon a predetermined treatment algorithm. A retrospective chart review of 2251 patients was performed utilizing our electronic medical record system (Epic Systems, Verona WI). Revenue was projected utilizing standard Medicare rates for our region while societal benefit was calculated using quality adjusted life years (QALY).
Results: Of the 2251 patient charts reviewed, 791 patients (35.1%) were seen by Montefiore ophthalmologists within a year of the original screening date. Estimated revenue generated by these visits was $276,800, with the majority from the treatment of retinal disease ($208,535), and the remainder from other ophthalmic conditions detected in the fundus photos ($68,265). There was a societal benefit of 14.66 quality adjusted life years (QALYs) with an estimated value of $35,471/QALY.
Conclusion: This telemedicine initiative was successful in identifying many patients with diabetic retinopathy and other ophthalmic conditions who may otherwise not have been formally evaluated. Our analysis demonstrates the program to generate a downstream revenue of nearly $280K with a cost benefit below < 50% of the threshold of $100,000/QALY, and therefore cost-effective in marginalized communities.
Keywords: cost-effectiveness, diabetic retinopathy, telemedicine, screening, utility
Introduction
Diabetic retinopathy (DR) is one of the top five leading causes of blindness worldwide,1 and is characterized by small vessel damage with subsequent exudation and ischemic injury.2 Currently, the American Diabetes Association (ADA) recommends persons living with diabetes to have a dilated ophthalmologic examination at least once a year.3 Adherence to this recommendation however is poor (<50–60%), and can be attributed to a multitude of logistical issues that are exacerbated by the initial asymptomatic nature of DR.4–8
Telemedicine can help address this inequity-related gap with comparable sensitivity and specificity to the standard dilated fundus examination, and has been recommended by the ADA in the absence of in-person screening.3,9 Social determinants of health contribute to 50–60% of health outcomes with disproportionate effects on racial and ethnic minorities.10–12 Compared to their Caucasian counterparts, African American and Hispanic patients are less likely to have adequate glycemic control and less likely to be screened, leading to worse health outcomes and increased rates of cataract, DR, glaucoma, and other eye diseases.13 The Bronx, the most ethnically diverse and lowest-income borough of New York City, has a particularly underserved population with high rates of poorly controlled diabetes.14,15 As such, telemedicine can improve diabetes-related vision care and help decrease disparities in diabetic eye disease among marginalized patients. This benefit is of even greater importance amidst the COVID-19 pandemic, which has disproportionately affected Hispanic and African American communities in New York City.16,17
Despite improvements in technology, telemedicine screening programs have been difficult to implement amongst underserved populations given limited experience with financial sustainability models and cost-effectiveness.18–20 If ophthalmic screening programs were shown to be cost-effective or profitable, they would be easier to implement, as has been successfully done with cholesterol and hypertension screening.21,22 To date, there are few studies looking at the cost-effectiveness of DR screening in the United States and the rest of North America.21 Cost-effectiveness studies use utility values for standardization which can be difficult to determine as a function of vision loss, and often rely on interview data from large populations.23–25 As a result, quantification of vision saved due to telemedicine screening often relies on theoretical assumptions that make it difficult to precisely estimate cost-effectiveness.26 Maberley et al’s DR screening study in James Bay Ontario was one of the earliest studies to analyze cost-effectiveness of a camera-based DR screening program, but relied mostly on simulation data.27 On the other hand, Garoon et al’s study on the urban population of Houston was one of the most recent and largest on cost-savings from camera-based DR screening, but did not utilize utility values and excluded DME.26,28
The aim of this study was to establish patient benefit and cost-effectiveness of a diabetic telemedicine screening program in an underserved population in the Bronx, New York. The study also assessed potential profitability in the screening and treatment of DR and non-DR eye disease.
Materials and Methods
This is a single institution, retrospective chart review study of a diabetic retinopathy screening program implemented by the Montefiore Health System between June 2014 and July 2016. The study was approved by the Einstein-Montefiore Institutional Review Board (IRB) and the study complied with the tenets of the Declaration of Helsinki and the Health Insurance Portability and Accountability Act (HIPAA). Informed consent was formally waived given the nature of the analysis, and data was de-identified to comply with all regulations. Fundus photography and image transmission was outsourced to HealPros LLC (Atlanta, GA), who furthermore provided $20,000 per month in support to help cover capital expenditures (hardware, software licensing fees, personnel, etc.). During a patient’s primary care physician visit, a trained technician took two to four 45-degree macula-centered (one-field) photos of both eyes using a non-mydriatic camera (Nidek AFC-230 or Ioptics Easyscan SLO). These images were uploaded to the hospital electronic medical record system (Epic Systems, Verona WI), and remotely interpreted by one of five trained Montefiore ophthalmologists utilizing the UK National Screening Committee (NSC) criteria. A grade of R0 – R3 was given correlating to the severity of the retinopathy seen.29 A grading of R0 corresponds to “no retinopathy”, R1 to “background retinopathy”, R2 to “pre-proliferative retinopathy”, and R3 to “proliferative retinopathy”. Hard exudates were used as surrogates for the detection of diabetic macular edema (DME). Ungradable images were classified as “Indeterminate” at the discretion of the trained reader. In cases where only one eye was considered “Indeterminate”, the fellow eye could still be assigned a grade of R1-R3 depending on the findings and clarity of the image. Although all patients were recommended to follow-up with an ophthalmologist within one year of being screened, patients with more severe forms of retinopathy (R2-R3) were scheduled appointments with urgency commensurate to the level of their disease by a centralized patient access center. If a patient did not answer, the call center would make two more attempts to contact the patient.
The inclusion criteria for the study required at least one recorded screening visit. For patients with multiple screenings in a primary care setting, only the first screening and subsequent clinical follow-up visits were taken into consideration for the purposes of this analysis. Demographic data was self-reported and documented as “N/A” when not specified. Age, race/ethnicity, HbA1c level (at the time of the screening visit), presence and severity of retinopathy, and other ocular comorbidities were captured from the electronic medical record. We furthermore collected revenue generating codes, including both common procedural terminology (CPT) and evaluation and management (E+M) codes for all testing, imaging, procedures, and visits for patients that followed up with Montefiore ophthalmologists within one year of their screening visit. Insurance status was not collected.
In order to provide a standardized estimate for the reimbursement of each CPT code, we used the Centers for Medicare and Medicaid Service (CMS) current rate at time of screening for the Bronx locality code 1320202. Revenue generated was estimated separately for DR (including DME) and non-DR ocular morbidities to more accurately account for multiple diseases that were being screened for with the fundus photos. For patients receiving a series of anti-vascular endothelial growth factor (VEGF) injections for more than a year, we estimated the revenue generated from an average of 5.8 injections based on standard treatment regimens in the literature.30
To evaluate societal cost and cost-effectiveness of the intervention, two different approaches were instituted. The first was to evaluate “sight-years saved” based on the treatment of four diseases: cataract, proliferative diabetic retinopathy (PDR), DME, and glaucoma. The cost of blindness was set at $15,900 per year based on the 2013 per person economic burden of the visually impaired.31 Treatment of proliferative DR and DME was assumed to save 0.065 and 0.06 sight years, respectively.32,33 Treatment of glaucoma was set at 0.011 sight years saved (based on the assumption of a 1.1% conversion to blindness per year).34 Treatment of cataract was set at 0.17 sight years saved (assumption of 17% rate of pre-operative blindness or visual impairment with reversal after surgery).35
The second approach was to calculate the number of Quality Adjusted Life Years (QALYs) saved.36 The incremental QALYs saved by treatments were obtained from the literature in order to standardize the results and avoid potential bias from non-ophthalmologic comorbidities. The QALYs saved are shown in Table 1 with corresponding references in parentheses.25,37,38 Note that the value of 0.18 for DME and PDR was obtained by using an estimate of 0.77 QALY for persons living with diabetes without any DR or DME and 0.59 for patients with PDR or DME.23
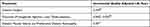 |
Table 1 Incremental Quality Adjusted Life Years Saved by Treatment |
Results
A total of 2251 patients met inclusion criteria including a documented screening visit. Of these screened patients, 35.1% (791 patients) followed up with a Montefiore ophthalmologist within one year. Demographic data from the EMR demonstrated that 287 of these patients (36.2%) self-identified as non-Hispanic Black, and 346 (43.7%) as Hispanic. The gender ratio (male: female) was calculated to be 0.60, with a mean age of 61 years (range 21–96 years), and a mean A1c of 8.2% (range 3.9–17.4%).
As shown in Table 2, 519 patients were found to screen positive for DR by fundus photography, of which 227 (43.7%) followed up with an ophthalmologist within one year. 152 (67.0%) of these patients were found to have retinopathy on this follow-up examination (‘true positives’). Of the 1607 patients who screened negative for DR by fundus photography, 513 (31.9%) followed up within one year, of which 468 (91.2%) had no retinopathy on clinical exam (“true negatives’). The screening program had a sensitivity of 77.2% and specificity of 86.2% in the detection of DR. Subgroup analysis of patient’s subsequent follow-up demonstrated that of the 162 patients who screened positive for DME, 71 (43.8%) followed up within one year with 20 (28.2%) showing clinical signs of DME on exam. Of the 2089 patients without DME on fundus photography, 720 (34.5%) patients followed up within a year, of which 688 (95.6%) had no DME on exam, giving the program a sensitivity and specificity of 38.5% and 93.1%, respectively, for DME detection from this perspective.
 |
Table 2 Rates of Diabetic Retinopathy (DR) and Diabetic Macular Edema (DME) Seen on Fundoscopic Image Screening and Clinical Exam |
Table 3 shows the breakdown of QALYs saved, sight years saved, and cost-saving to society. The operating cost of the program was approximately $520,000 based on budgeted expenditures of approximately $20,000/month. The Cost/QALY (lower number indicating better cost-effectiveness) for treating diabetic eye disease was $57,778/QALY, with an overall estimate of $35,471/QALY when including treatment for all ophthalmic diseases detected. The total cost saving to society (using $15,900 for 1 sight year saved) was $124,736, with 39.3% from treating diabetic eye disease and 61.7% from treating non-retinal disease.31
 |
Table 3 Overview of Sight Years and Quality Adjusted Life Years Saved |
Potential procedural revenue generated from standard treatment regimens was estimated (using CMS reimbursement for individual CPT codes) to be $276,800, with 75.3% coming from treating DR and 24.7% from the treatment of non-retinal disease (Table 4).
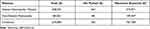 |
Table 4 Estimate of Revenue Generated |
Discussion
Given rapidly increasing rates of diabetes in the US and the substantial burden of diabetic eye disease,1 it has become increasingly imperative that we implement large scale diabetic retinopathy screening programs to adequately screen and treat patients who have poor access to healthcare. To date, there are few studies looking at the cost-effectiveness of DR screening, particularly in urban and underserved communities who are often the most vulnerable.21 Study populations may have disparities in the social determinants of health, making many of these comparisons difficult. The study of this screening program implemented by the Montefiore Health System was similar to other studies26,39,40 in terms of DR prevalence, “indeterminate” image rates, and proportion of patients treated. Although it had a lower sensitivity for DR compared to Lee et al’s study of 1-field non-mydriatic color photography despite a similar study population, the sensitivity for DME was comparable to other studies that had variable rates as low as <30%.41,42
Our study found similar societal benefit compared to other ophthalmic27,43 and non-ophthalmic22 screening programs. Maberley et al’s study model found that they saved more than two times the number of sight years and almost twice the number of QALYs in the treatment of DR and DME, likely from having a greater proportion of patients with DME and PDR requiring treatment.27 Thomas et al’s simulation analysis of a telemedicine-based glaucoma screening program also saved a similar number of QALYs.43 Finally, as health systems have limited resources, they have to prioritize screening programs for both ophthalmologic and non-ophthalmologic disease. Our DR screening program’s benefit (from a QALY/patient per year perspective) was comparable to programs for hypertension and hypercholesterolemia.22
This analysis found that our DR screening program was not only cost-effective but furthermore has the potential for significant profitability, particularly if follow-up visit compliance could be improved. A cost/QALY threshold of $50,000 is frequently cited in the literature, although Neumann et al have argued that this is too low of a threshold in the United States, with $100,000 or $150,000 as more reasonable estimates.36,44 From a DR and DME treatment perspective, the program met Neumann et al’s cost/QALY threshold of $100,000, while the $50,000 threshold was met when treatment for non-retinal disease was included.44 While Maberley et al’s study had one fourth the cost/QALY as compared to our study, they had a greater proportion of patients treated and half the screening cost.27 Furthermore, Kirkizlar et al DR screening model showed that a DR screening program of 3000 patients in the United States should have an average cost/QALY of $53,556, making our $57,778/QALY for 2251 patients reasonably viable.45
Our estimates show that this program would be cost-neutral when compliance with follow-up appointments approaches approximately 70%. If also including the cost-saving to society, the program becomes cost-neutral at a much lower threshold of approximately 50%. It is important to note that as hardware costs decline, the initial barriers to entry do so as well. Furthermore, newer cameras do not require specialized training to operate, and as a result, program costs could have decreased by nearly 30% with the requirement of a photographer eliminated.46 In current dollars, the cost of the screening program would have decreased to $364,000, and the program would only require approximately 16% more follow-up than what we found to become cost-neutral. The cost/QALY for DR and DME screening and treatment would have decreased to $40,444, well below a more stringent $50,000 threshold. In addition, the use of older technology for the study makes the QALY gains more applicable to international populations where access to cutting edge technology may be more limited.
Unfortunately, there is a paucity of data on revenue generated from increased access to care due to screening programs. If we view Garoon et al’s estimated costs for clinic visits and treatment of DR as a proxy for revenue of their health system, we find that our study had comparable revenue generation.26 The majority of their “revenue” came from treatment of DR with PRP or surgery, while a bulk of our revenue was from the treatment and testing of DME. Our adherence rate was notably lower, however, and this fact could be due to exclusion of non-Montefiore ophthalmology visits and less stringent criteria for follow-up.
There are some limitations to this study. Revenue was estimated using Medicare rates instead of actual collections. It is likely we underestimated the revenue projections given that operating room, anesthesia, and reading costs were not included. Our calculations for “QALYs gained” were calculated under the assumption that we had perfect treatment efficacy, and did not account for patients who were lost to follow-up that potentially cost the system resources. We also did not make a distinction for QALYs calculated depending on if patients were type 1 or type 2 diabetics. In addition, as this was a retrospective chart analysis, we used estimated QALYs from the literature instead of obtaining them from our patient population through direct interview. Finally, our revenue generation and societal benefit have an underlying assumption that patients follow-up in clinic once their issues are highlighted by the screening program.
Conclusions
The Montefiore Health System telemedicine screening initiative is cost-effective and has particularly significant societal benefit in underserved populations. Screening programs should be adopted to facilitate cost-effective care and equilibrate health-care access throughout our health-care system. Societal, community, and patient benefits, in addition to improved access for vulnerable patients, can provide long-standing and sustainable benefit. Further reductions in hardware costs and improved ease of use will continue to improve our ability to screen and treat these patients.
Abbreviations
DR, Diabetic Retinopathy Screening; MHS, Montefiore Health System; QALY, Quality Adjusted Life Year; DME, Diabetic Macular Edema; PDR, Proliferative Diabetic Retinopathy; PPDR, Pre-proliferative Diabetic Retinopathy; VEGF, Vascular endothelial growth factor.
Ethics Approval and Informed Consent to Participate
The study was approved by the Einstein/Montefiore Medical Center Institutional Review Board (IRB)/Ethics Committee and conducted in accordance with the tenets of the Declaration of Helsinki. Informed consent for this retrospective analysis was waived by the Einstein/Montefiore Medical Center Institutional Review Board (IRB)/Ethics Committee.
Data Sharing Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The abstract of this paper was presented at the ARVO 2019 Annual meeting as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Investigative Ophthalmology and Visual Science:https://iovs.arvojournals.org/article.aspx?articleid=2744766. The authors acknowledge Jim Sullivan, Dr. Joel Zonszein, Kripali Gautam, Michelle Goodman for their contributions in this study.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis. 2015;2:1–25.
2. Wong TY, Sun J, Kawasaki R, et al. Guidelines on diabetic eye care: the international council of ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125:1608–1622. doi:10.1016/j.ophtha.2018.04.007
3. Solomon SD, Chew E, Duh EJ, et al. Diabetic retinopathy: a position statement by the American Diabetes Association. Diabetes Care. 2017;40:412–418. doi:10.2337/dc16-2641
4. Liu Y,Zupan NJ, Shiyanbola OO, et al. Factors influencing patient adherence with diabetic eye screening in rural communities: a qualitative study. PLoS One. 2018;13:e0206742.
5. Murchison AP, Hark L, Pizzi LT, et al. Non-adherence to eye care in people with diabetes. BMJ Open Diabetes Res Care. 2017;5:e000333. doi:10.1136/bmjdrc-2016-000333
6. Keenum Z, McGwin G, Witherspoon CD, et al. Patients’ adherence to recommended follow-up eye care after diabetic retinopathy screening in a publicly funded county clinic and factors associated with follow-up eye care use. JAMA Ophthalmol. 2016;134:1221–1228. doi:10.1001/jamaophthalmol.2016.3081
7. Thompson AC, Thompson MO, Young DL, et al. Barriers to follow-up and strategies to improve adherence to appointments for care of chronic eye diseases. Invest Ophthalmol Vis Sci. 2015;56:4324–4331. doi:10.1167/iovs.15-16444
8. Adriono G, Wang D, Octavianus C, Congdon N. Use of eye care services among diabetic patients in urban Indonesia. Arch Ophthalmol. 2011;129:930–935. doi:10.1001/archophthalmol.2011.147
9. Ahmed J, Ward TP, Bursell S-E, et al. The sensitivity and specificity of nonmydriatic digital stereoscopic retinal imaging in detecting diabetic retinopathy. Diabetes Care. 2006;29:2205–2209. doi:10.2337/dc06-0295
10. Ogunwole SM, Golden SH. Social determinants of health and structural inequities—root causes of diabetes disparities. Diabetes Care. 2021;44:11–13. doi:10.2337/dci20-0060
11. Kulshreshtha A, Goyal A, Dabhadkar K, Veledar E, Vaccarino V. Urban-rural differences in coronary heart disease mortality in the United States: 1999–2009. Public Health Rep. 2014;129:19–29. doi:10.1177/003335491412900105
12. Hamedani AG, VanderBeek BL, Willis AW. Blindness and visual impairment in the medicare population: disparities and association with hip fracture and neuropsychiatric outcomes. Ophthalmic Epidemiol. 2019;26:279–285. doi:10.1080/09286586.2019.1611879
13. Zambelli-Weiner A, Crews JE, Friedman DS. Disparities in adult vision health in the United States. Am J Ophthalmol. 2012;154:S23–S30.e1. doi:10.1016/j.ajo.2012.03.018
14. Wu WY, Jiang Q, Di Lonardo SS. Poorly controlled diabetes in New York city: mapping high-density neighborhoods. J Public Health Manag Pract JPHMP. 2018;24:69–74. doi:10.1097/PHH.0000000000000544
15. Farrell P, Barnaby S, Galarza T, et al. Population management of diabetes in a high-need urban community in the Bronx: the experience of Montefiore Medical Center. Diabetes Educ. 2013;39:515–522. doi:10.1177/0145721713487259
16. Mike EV, Laroche D. Preserving vision in the COVID-19 pandemic: focus on health equity. Clin Ophthalmol Auckl NZ. 2020;14:2073–2077. doi:10.2147/OPTH.S262586
17. Alroy KA, Crossa A, Dominianni C, et al. Population-based estimates of coronavirus disease 2019 (COVID-19)–like illness, COVID-19 illness, and rates of case ascertainment, hospitalizations, and deaths—noninstitutionalized New York city residents, March–April 2020. Clin. Infect. Dis. 2021;73:1707–1710. doi:10.1093/cid/ciab038
18. Byrne MM, Parker DF, Tannenbaum SL, et al. Cost of a community-based diabetic retinopathy screening program. Diabetes Care. 2014;37:e236–e237. doi:10.2337/dc14-0834
19. James M, Turner DA, Broadbent DM, Vora J, Harding SP. Cost effectiveness analysis of screening for sight threatening diabetic eye disease. BMJ. 2000;320:1627–1631. doi:10.1136/bmj.320.7250.1627
20. Silva PS, Cavallerano JD, Aiello LM, Aiello LP. Telemedicine and diabetic retinopathy: moving beyond retinal screening. Arch Ophthalmol. 2011;129:236–242. doi:10.1001/archophthalmol.2010.365
21. Avidor D, Loewenstein A, Waisbourd M, Nutman A. Cost-effectiveness of diabetic retinopathy screening programs using telemedicine: a systematic review. Cost Eff Resour Alloc CE. 2020;18:1–9.
22. Dehmer SP, Maciosek MV, LaFrance AB, Flottemesch TJ. Health benefits and cost-effectiveness of asymptomatic screening for hypertension and high cholesterol and aspirin counseling for primary prevention. Ann Fam Med. 2017;15:23–36. doi:10.1370/afm.2015
23. Brown MM, Brown GC, Sharma S, Shah G. Utility values and diabetic retinopathy. Am J Ophthalmol. 1999;128:324–330. doi:10.1016/S0002-9394(99)00146-4
24. Prieto L, Sacristán JA. Problems and solutions in calculating quality-adjusted life years (QALYs). Health Qual Life Outcomes. 2003;1(80):1–8.
25. Brown GC, Brown MM, Chaudhry I, Stein JD. Opportunities to reduce potential bias in ophthalmic cost-utility analysis. JAMA Ophthalmol. 2021;139:389–397. doi:10.1001/jamaophthalmol.2020.6591
26. Garoon RB, Lin WV, Young AK, et al. Cost savings analysis for a diabetic retinopathy teleretinal screening program using an activity-based costing approach. Ophthalmol Retina. 2018;2:906–913. doi:10.1016/j.oret.2018.01.020
27. Maberley D, Walker H, Koushik A, Cruess A. Screening for diabetic retinopathy in James Bay, Ontario: a cost-effectiveness analysis. CMAJ Can Med Assoc J. 2003;168:160–164.
28. Weinstein MC, Stason WB. Foundations of cost-effectiveness analysis for health and medical practices. N Engl J Med. 1977;296:716–721. doi:10.1056/NEJM197703312961304
29. Shotliff K, Duncan G. Diabetic retinopathy: summary of grading and management criteria. Pract Diabetes Int. 2006;23:418–420. doi:10.1002/pdi.1029
30. Arevalo JF, Sanchez JG, Wu L, et al. Primary intravitreal bevacizumab for diffuse diabetic macular edema: the pan-american collaborative retina study group at 24 months. Ophthalmology. 2009;116:1488–1497.e1. doi:10.1016/j.ophtha.2009.03.016
31. Wittenborn J, Rein D, Feagan CW, NORC at the University of Chicago. The economic burden of vision loss and eye disorders in the United States. Ophthalmology. 2013;120(9):1728–1735. doi:10.1016/j.ophtha.2013.01.068
32. ETDRS Research Group. Photocoagulation for diabetic macular edema: early treatment diabetic retinopathy study report number 1 early treatment diabetic retinopathy study research group. Arch Ophthalmol. 1985;103:1796–1806. doi:10.1001/archopht.1985.01050120030015
33. The Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy. clinical application of Diabetic Retinopathy Study (DRS) findings, DRS report number 8. Ophthalmology. 1981;88:583–600.
34. Rossetti L, Digiuni M, Giovanni M, et al. Blindness and glaucoma: a multicenter data review from 7 academic eye clinics. PLoS One. 2015;10(8):e0136632. doi:10.1371/journal.pone.0136632
35. Shah SP, Gilbert CE, Razavi H, Turner EL, Lindfield RJ. Preoperative visual acuity among cataract surgery patients and countries’ state of development: a global study. Bull World Health Organ. 2011;89:749–756. doi:10.2471/BLT.10.080366
36. Firth SJ. The quality adjusted life year: a total-utility perspective. Camb Q Healthc Ethics CQ Int J Healthc Ethics Comm. 2018;27:284–294. doi:10.1017/S0963180117000615
37. Real FJ, Brown GC, Brown HC, Brown MM. The effect of comorbidities upon ocular and systemic health-related quality of life. Br J Ophthalmol. 2008;92:770–774. doi:10.1136/bjo.2007.127407
38. Brown MM, Brown GC, Sharma S, Hollands H, Landy J. Quality of life and systemic comorbidities in patients with ophthalmic disease. Br J Ophthalmol. 2002;86:8–11. doi:10.1136/bjo.86.1.8
39. Jani PD, Forbes L, Choudhury A, et al. Evaluation of diabetic retinal screening and factors for ophthalmology referral in a telemedicine network. JAMA Ophthalmol. 2017;135:706–714. doi:10.1001/jamaophthalmol.2017.1150
40. Mansberger SL, Gleitsmann K, Gardiner S, et al. comparing the effectiveness of telemedicine and traditional surveillance in providing diabetic retinopathy screening examinations: a randomized controlled trial. Telemed J E Health. 2013;19:942–948. doi:10.1089/tmj.2012.0313
41. Lee JC, Nguyen L, Hynan LS, Blomquist PH. Comparison of 1-field, 2-fields, and 3-fields fundus photography for detection and grading of diabetic retinopathy. J Diabetes Complications. 2019;33:107441. doi:10.1016/j.jdiacomp.2019.107441
42. Ullah W, Pathan SK, Panchal A, et al. Cost-effectiveness and diagnostic accuracy of telemedicine in macular disease and diabetic retinopathy. Medicine. 2020;99:e20306. doi:10.1097/MD.0000000000020306
43. Thomas S, Hodge W, Malvankar-Mehta M. The cost-effectiveness analysis of teleglaucoma screening device. PLoS One. 2015;10:e0137913. doi:10.1371/journal.pone.0137913
44. Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness — the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371:796–797. doi:10.1056/NEJMp1405158
45. Kirkizlar E, Serban N, Sisson JA, et al. Evaluation of telemedicine for screening of diabetic retinopathy in the veterans health administration. Ophthalmol. 2013;120:2604–2610. doi:10.1016/j.ophtha.2013.06.029
46. DeBuc DC. The role of retinal imaging and portable screening devices in tele-ophthalmology applications for diabetic retinopathy management. Curr Diab Rep. 2016;16(132). doi:10.1007/s11892-016-0827-2
47. Brown GC, Brown MM, Busbee BG. Cost-utility analysis of cataract surgery in the United States for the year 2018. J Cataract Refract Surg. 2019;45:927–938. doi:10.1016/j.jcrs.2019.02.006
48. Stein JD, Kim DD, Peck WW, Giannetti SM, Hutton DW. Cost-effectiveness of medications compared with laser trabeculoplasty in patients with newly diagnosed open-angle glaucoma. Arch Ophthalmol Chic Ill 1960. 2012;130:497–505.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
