Back to Journals » Journal of Blood Medicine » Volume 12
The Correlation Between Iron Overload and Endocrine Function in Adult Transfusion-Dependent Beta-Thalassemia Patients with Growth Retardation
Authors Atmakusuma TD , Hasibuan FD, Purnamasari D
Received 18 June 2021
Accepted for publication 31 July 2021
Published 17 August 2021 Volume 2021:12 Pages 749—753
DOI https://doi.org/10.2147/JBM.S325096
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Tubagus Djumhana Atmakusuma,1 Faizal Drissa Hasibuan,2 Dyah Purnamasari3
1Division of Hematology-Medical Oncology, Department of Internal Medicine, Dr. Cipto Mangunkusumo General Hospital/Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia; 2Division of Hematology-Medical Oncology, Department of Internal Medicine, Yarsi Hospital, Jakarta, Indonesia; 3Endocrine and Metabolic Division, Department of Internal Medicine, Dr. Cipto Mangunkusumo General Hospital/Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia
Correspondence: Tubagus Djumhana Atmakusuma
Division of Hematology-Medical Oncology, Department of Internal Medicine, Dr. Cipto Mangunkusumo General Hospital/Faculty of Medicine Universitas Indonesia, Jalan Diponegoro No. 71, Jakarta Pusat, DKI Jakarta, Indonesia
Tel +6221-3162497
Email [email protected]
Background: Iron overload is a major problem in patients with transfusion-dependent beta-thalassemia (TDT). Reports on the correlation between iron overload and endocrine function with growth retardation in such a population in Indonesia have not been established. Therefore, this study aims to obtain a profile of iron load and endocrine function of adult transfusion dependent beta-thalassemia patients and their correlation with growth retardation.
Methods: A cross-sectional study was performed, involving adult homozygous and HbE beta-thalassemia patients receiving blood transfusions at the Cipto Mangunkusumo Hospital, Jakarta. Iron overload was represented by serum ferritin (FS) and transferrin saturation (TS), while the endocrine function was examined by the Thyroid Stimulating Hormone-sensitive (TSHs), free T4 (fT4), and insulin-like growth factor-1 (IGF-1). The results were analyzed using bivariate analysis plus Pearson and Spearman correlation tests.
Results: In general, 58 subjects were selected from 224 adult transfusion dependent beta- thalassemia patients, consisting of 31 males (53.4%) and 27 females (46.6%). Furthermore, their median age was 21 (18– 24) years, while the subclinical hypothyroid proportion was 32.7% and low IGF-1 levels were detected in 79.3% of the total population. There was a weak negative correlation between FS and fT4 (Spearman rho=− 0.361; p=0.003), as well as IGF-1 (Spearman rho=− 0.313; p=0.008), but FS and TSHs had no correlation (Spearman rho=0.074; p=0.29). Also, there was no correlation between ST with TSHs (Spearman rho=0.003; p=0.492), fT4 (Spearman rho=0.018; p=0.448), and IGF-1 (Spearman rho=− 0.142; p=0.143).
Conclusion: Based on serum ferritin, iron overload is discovered to have a negative correlation with free T4 and insulin-like growth factor-1.
Keywords: IGF-1, TSHs, fT4, serum ferritin, transferrin saturation, transfusion-dependent thalassemia
Background
Thalassemia is a hereditary disease caused by a defect in the synthesis of globin. Moreover, beta-thalassemia is the commonest type, affecting about 80–90 million people or 1.5% of the global population. Indonesia is one of the countries with a high thalassemia prevalence of the disease, where the beta-thalassemia trait carrier is estimated as about 3–10%.1,2 With a population of approximately 250 million and a 20% birth rate, about 5000 babies are predicted to be born with beta-thalassemia. Based on the data from Cipto Mangunkusumo Hospital (RSCM) in 2016, 9031 people were suffering from thalassemia major in Indonesia. Also, up to 441 adult patients (age over 18 years) were recorded in Kiara thalassemia and Hematology-oncology department of Internal Medicine clinics.3
Thalassemia major (TM) is one of the thalassemia phenotypes characterized by severe anemia. Patients with TM require regular red blood cell transfusions, which are mandatory for their survival, therefore this condition is called TDT. Repeated red blood cell transfusions lead to iron overload in tissues or organs, thereby causing an impairment called iron toxicity which has several targets including the endocrine system. In addition, endocrine disorders are often detected in those suffering from TDT. Some studies indicated approximately 40–50% of thalassemia patients that received adequate transfusion therapy remained to have endocrine disorders such as a decrease in hormone levels or substances produced by the endocrine organs.4–8
Many of the thalassemia patients in Cipto Mangunkusumo Hospital experience growth retardation which has an impact on their psychosocial development. Several factors contribute to the development of growth retardation such as inadequate transfusion causing chronic anemia, iron overload, malnutrition, and desferrioxamine toxicity. Iron overload in endocrine organs leads to hypogonadism, disorders of growth hormone-insulin-like growth factor 1 (GH-IGF-1) axis, and hypothyroidism.9–12
Iron toxicity is caused by an overload of the respective element, a condition related to non-transferrin-bound iron (NTBI). Furthermore, NTBI examination has not been standardized and is not available in Indonesia, but TS is used as a surrogate marker of this process.13–15
T2* MRI is the gold standard for assessing iron overload and toxicity.16,17 However, in centers with limited resources, serum ferritin (SF) is often used to assess iron overload. Besides, the pancreas is an endocrine organ routinely measured using MRI T2*. The examination has become a standard procedure in developed countries, but it is still only used for study purposes in Indonesia. Since this sophisticated modality is not available nationwide, TS and SF are targeted to be used as surrogate markers of iron overload.
Soesanti et al18 conducted a study on 67 children with thalassemia in 2012. The result showed the prevalence of endocrine disorders as follows: 64% growth retardation, 41% hypothyroidism, and 20% late puberty. There is no publication of endocrine function in adult TDT beta patients with growth retardation in Indonesia yet. Therefore, this study aims to determine the correlation between iron overload and endocrine function.
Methods
This was a cross-sectional study that obtained a profile of iron load and endocrine function correlation in adult beta TDT patients with growth retardation in Cipto Mangunkusumo Hospital in December 2017. The endocrine function was observed by the thyroid hormone levels (Thyroid Stimulating Hormone-sensitive/TSHs and free T4/fT4) and insulin-like growth factor-1 (IGF-1).
Patients diagnosed with beta-thalassemia and beta-HbE (with high-performance liquid chromatography/HPLC or microcapillary) aged 18 years with growth retardation were included as subjects. The exclusion criteria were HbsAg or anti-HCV positive patients or when the subject did not agree to participate. This study was approved by the Ethical Committee of the Faculty of Medicine, Universitas Indonesia, as listed on the Ethical Approval Letter number 1133/UN.2.F1/ETIK/2017. All patients provided appropriate informed consent and were treated in accordance with the Declaration of Helsinki.
The subjects were recruited consecutively from Kiara thalassemia Polyclinic and Hematology-oncology department of Internal Medicine clinic. Each of them passed through venous blood sampling prior to the transfusion process. The blood samples collected were up to two tubes, namely 7 mL and 3 mL in size. The TSHs, FT4, Ferritin, SF, and TS examinations were performed at the clinical pathology laboratory of Cipto Mangunkusumo Hospital Jakarta, using chemiluminescence immunoassay (CMIA) method by Abbott™ Architect® i1000/i2000 device. Levels of SI and TIBC were measured using the direct colorimetric method by Abbott™ Architect® c4000/8000 device. Meanwhile, IGF-1 level was measured using the Solid-Phase method Electro-Chemiluminescence Immunoassay (ECLIA) by Siemens™ Immulite® 1000.
The data obtained were analyzed using Pearson’s correlation test for those with normal distribution or Spearman correlation test for the ones with an abnormal (non-parametric) distribution. Since data distribution was abnormal, the nonparametric Spearman correlation was used.
Results
In December 2017, 68 people were diagnosed with growth retardation among 224 adult TDT beta patients in Kiara thalassemia Polyclinic and Hematology-oncology department of Internal Medicine clinic. Then, 10 of the 68 that met the inclusion criteria were not willing to continue, therefore only 58 completed the study.
The subjects were 27 (46.6%) females and 31 (53.4%) males (Table 1). Furthermore, their median age was 21 years, with a range of 18 to 24 years. The number of homozygous beta-thalassemia patients was 31 (53.4%) and those with HbE beta-thalassemia were 27 (46.6%). The Mid Parental Height as a benchmark target for the patient’s height was 161.25 cm. Meanwhile, the average height of the subjects was 149.05 cm.
 |
Table 1 Baseline Characteristics of Research Subject |
The Proportion of Endocrine Disorders on Study Subjects
Table 2 shows the proportion of low IGF-1 was 79.3%, and subclinical hypothyroidism was 32.7%. The subclinical hypothyroidism was characterized by elevated TSHs (≥5 mu/L) with normal fT4 levels, and most patients had no complaints.
 |
Table 2 Proportion of Endocrine Function in Adult Beta TDT Patients with Growth Retardation |
The Correlation Between Iron Overload and Endocrine Function in Adult TDT Beta Patients
The results from Spearman’s test showed no significant correlation between transferrin saturation with TSHs, fT4, and IGF-1 (Table 3).
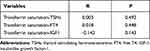 |
Table 3 Correlation Between Transferrin Saturation with TSH, fT4 and IGF-1 |
Meanwhile, there was a weak significant correlation between serum ferritin with fT4 and IGF-1 (r = −0.361; p = 0.003 and r = −0.313; p = 0.008), but FS and TSHs had no correlation (Table 4)
 |
Table 4 The Correlation Between Serum Ferritin with TSH, fT4 and IGF-1 |
It can be concluded that there is a negative correlation between serum ferritin with fT4 and IGF-1. However, FS and TSHs have no correlation, hence transferrin saturation does not correlate with TSHs, fT4, and IGF-1.
Discussion
This study is the first to report the proportion of endocrine function disorders in adult TDT patients with growth retardation and its correlation with iron overload in the Indonesian population, particularly in the RSCM Jakarta.
The average values of the subjects’ TSHs and fT4 were in the normal range. But, there were 32.7% of patients with subclinical hypothyroidism, a condition that has an unclear mechanism in TDT beta occurrence. This is probably due to thyroid tissue damage causing iron overload which releases free radicals, while the pituitary has not been damaged. Low TSHs and fT4 levels were not detected, indicating there was no serious damage to the pituitary and thyroid glands due to iron overload.
In this study, the proportion of low IGF-1 was 79.3% with an average median value of 60.5 ng/mL. Poggi et al8 did not report the proportion of low IGF-1, but only a mean value of 88.2±39.9 ng/mL. However, Rashid et al20 obtained 51.43%, and Soliman et al5 obtained 67%. Also, Scacchi et al22 reported 46.8% and Moayeri, and Oolomi25 discovered 42% in the group that was growth retarded. From the description above, the proportion of low IGF-1 in this study was greater than in previous ones possibly due to the higher iron overload.
Iron overload on the pituitary, thyroid, and liver causes iron toxicity that damages the cells playing a role in the synthesis of TSH, fT4, and IGF-1. Consequently, the levels of these hormones are reduced, leading to hypothyroidism or growth retardation.
In the test conducted, transferrin saturation had no significant correlation with TSH, fT4, and IGF-1. Supposedly as a surrogate marker of iron overload, TS correlated with endocrine variables. This was probably because transferrin saturation measurements were performed only once. Hence, the effect of iron overload for a long time was not envisaged. Similarly, Al-Hakeim et al24 reported there was no transferrin saturation correlation with TSH and T4.
There was a weak negative correlation between serum ferritin with fT4 and IGF-1 (r = −0.361; p = 0.003 and r = −0.313; p = 0.008), but serum ferritin and TSHs had no significant correlation (r = 0.074; p = 0.29). The correlation between FS with fT4 and IGF-1 showed a decreased fT4 and low IGF-1 due to iron overload in the thyroid gland and liver. In contrast to Soliman et al19 there is no significant correlation between FS and IGF-1. This is related to Eshragi et al21 that did not obtain any correlation between FS and hypothyroidism as well as Zervas et al23 that obtained no correlation between FS and thyroid disorders. In other Soliman et al19 studies, a negative correlation was obtained between FS and fT4, however, FS and TSH had no correlation, which is similar to this current study.
Conclusions
In general, the proportion of IGF-1 is quite high, namely 79.3%, while that of subclinical hypothyroidism is 32.7% and MRI T2* pancreas is 87.5% in the group of adult TDT beta patients that experienced growth retardation. Proportions of with low value of in adult patients who experienced a beta TDT beta growth retardation. As assessed by serum ferritin, there is a negative correlation between iron overload with fT4 and IGF-1. However, there is no correlation between FS and TSHs, hence transferrin saturation does not correlate with TSHs, fT4, and IGF-1.
Data Sharing Statement
Additional data can be requested by contacting the corresponding author on the email address provided.
Acknowledgments
This paper is based on a thesis written in 2018 by Hasibuan FD, Atmakusuma TD, Purnamasari D, and Rumende CM. The title is Korelasi antara muatan besi berlebih dengan fungsi endokrin pada pasien dewasa thalassemia beta bergantung transfusi yang mengalami retardasi pertumbuhan [The correlation between iron overload and endocrine function in adult transfusion-dependent beta-thalassemia patients with growth retardation].26
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wahidayat I, Wahidayat PA. Genetic problems at present and their challenges in the future: as a model of thalassemia. Paediatr Indonesiana. 2006;46(5):189–194. doi:10.14238/pi46.5.2006.189-94
2. Sofro ASM. Molecular pathology of beta-thalassemia in Indonesia. Southeast Asian J Trop Med Public Health. 1995;26:221–224.
3. Thalassemia Center Cipto Mangunkusumo Hospital. Data Thalassemia Major Patients in Indonesia in 2015–2016. Jakarta; 2016.
4. Sanctis VD, Soliman AT, Skordis N. Endocrine disease. In: Cappellini CA, Porter J, editors. Guidelines for the Management of Transfusion-Dependent Thalassemia (TDT).
5. Soliman A, Sanctis VD, Yassin M, Abdelrahman MO. Growth hormone – insulin-like growth factor-I axis and bone mineral density in adults with thalassemia major. Indian J Endocrinol Metab. 2014;18(1):32c–8.
6. Abdelhadi MA. Endocrinopathies in beta-thalassemia major: prevalence, risk factors, and age at diagnosis in Northwest Saudi Arabia. Saudi Med J. 2013;34(1):67–73.
7. Perera NJ, Lau NS, Mathew S, Waite C, Ho PJ, Caterson ID. Overview of endocrinopathies associated with b-thalassemia major. Intern Med J. 2010;40(10):689–696. doi:10.1111/j.1445-5994.2010.02254.x
8. Poggi M, Pascucci C, Monti S, et al. Prevalence of adult growth hormone deficiency in β-thalassemia polytransfused Patients and Correlation with transfusional and chelation parameters. J Endocrinol Invest. 2010;33(8):534–538. doi:10.1007/BF03346643
9. Sanctis VD, Urso L, Scialpi V. Endocrine complications in β-thalassemia major. In: Maggio A, Hoffbrand AV, editors. Clinical Aspects and Therapy of Hemoglobinopathies. Italy: SEE-Firenze; 2014:293–315.
10. Olivieri NF, Weatherall DJ. Clinical aspects ofβ-thalassemia and related disorders. In: Steinberg MH, Forget BG, Higgs DR, editors. Disorders of Hemoglobin: Genetics, Pathophysiology and Clinical Management. UK: Cambridge University Press; 2009:357–369.
11. Kuskonmaz BC. Endocrinological problems in adult thalassemia patients. Gazi J Med. 2014;25:173–176.
12. Tzoulis P. Review of endocrine complications in adult patients with β-thalassemia major. Thalassemia Rep. 2014;4:51–56.
13. Kohgo Y, Ikuta K, Ohtake T, Torimoto Y, Kato J. Body of iron metabolism and pathophysiology of iron overload. Int J Hematol. 2008;88(1):7–15. doi:10.1007/s12185-008-0120-5
14. Crichton R. Iron and Oxidative Stress. Iron Metabolism - from Molecular Mechanisms to Clinical Consequences.
15. Barton JC, Edwards CQ, Phatak PD, Britton RS, Bacon BR. Normal Iron Metabolism and Iron Toxicity. In: Handbook of Iron Overload Disorders.
16. Argyropoulou MI, Kiortsis DN, Astrakas L, Metafratzi Z, Chalissos N, Efremidis SC. Liver, bone marrow, pancreas and pituitary gland iron overload in young and adult thalassemic patients: a T2 Relaxometry Study. Eur Radiol. 2007;17(12):3025–3030. doi:10.1007/s00330-007-0683-1
17. Chirico V, Rigoli L, Lacquniti A, et al. Endocrinopathies, metabolic disorders, and iron overload in thalassemia major and intermedia: serum ferritin as diagnostic and predictive markers associated with liver and cardiac T2 * MRI assessment. Eur J Haematol. 2014;1–9.
18. Soesanti F, Putriasih SA, Pulungan A, Wahidiyat PA. Endocrinopathies in thalassemia major patients in thalassemia center in Jakarta, Indonesia. Int J Pediatr Endocrinol. 2013;2013(S1):58. doi:10.1186/1687-9856-2013-S1-P58
19. Soliman AT, Al Yafei F, Al-Naimi L, Almarri N, Sabt A, Yassin M, et al. Longitudinal study on thyroid function in patients with thalassemia major: high incidence of central hypothyroidism by 18 years. Indian J Endocrinol Metab. 2013;17(6):1090–5.
20. Rashid HM, Shirodkar A, Ahmed J. Evaluation of growth, puberty and endocrine dysfunctions in relation to iron overload in thalassemia patients multitransfused Indian. Indian J Pediatr. 2011;78(6):679–683. doi:10.1007/s12098-010-0351-3
21. Eshragi P, Tamaddoni A, Zarifi K, Mohammadhasani A, Aminzadeh M. Thyroid function in patients with thalassemia major: is it related to height and chelation therapy ? Casp J Intern Med. 2011;2(1):190–193.
22. Scacchi M, Danesi L, Cattaneo A, Valassi E, Giraldi FP, Argento C, et al. Growth hormone deficiency (GHD) in adult thalassaemic patients. Clin Endocrin. 2007;67(5):790–5.
23. Zervas A, Katopodi A, Protonotariou A, Livadas S, Karagiorga M, Politis C, et al. Assessment of thyroid function in two hundred patients with betathalassaemia major. Thyroid. 2002;12:151–4.
24. Al-Hakeim HK, Al-Hakany MF. The effect of iron overload on the function of some endocrine glands in β-thalassemia major patients. Magazin of Al-kufa University for Biology. 2013;5:1–22.
25. Moayeri H, Oolomi Z. Prevalence of growth and puberty failure with respect to growth hormone and gonadotropins secretions in beta-thalassemia major. Arch Iran Med. 2006;9(4):329–334.
26. Hasibuan FD, Atmakusuma TD, Purnamasari D, Rumende CM. Korelasi antara muatan besi berlebih dengan fungsi endokrin pada pasien dewasa thalassemia beta bergantung transfusi yang mengalami retardasi pertumbuhan [The Correlation Between Iron Overload and Endocrine Function in Adult Transfusion Dependent Beta Thalassemia Patients with Growth Retardation] [Thesis]. Indonesia; 2018.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
