Back to Journals » Clinical Ophthalmology » Volume 17
The Combined Utilization of Epithelial Thickness Mapping and Tomography in Keratorefractive Surgery Screening: One Imaging Modality is Not Sufficient
Authors Corbin WM , Payne CJ, Momeni-Moghaddam H , Ronquillo YC , Hoopes Snr PC , Moshirfar M
Received 3 February 2023
Accepted for publication 30 March 2023
Published 24 May 2023 Volume 2023:17 Pages 1457—1463
DOI https://doi.org/10.2147/OPTH.S404019
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Wyatt M Corbin,1 Carter J Payne,2,3 Hamed Momeni-Moghaddam,4 Yasmyne C Ronquillo,2 Phillip C Hoopes Snr,2 Majid Moshirfar2,5,6
1Stritch School of Medicine, Loyola University Chicago, Maywood, IL, USA; 2Hoopes Vision Research Center, Hoopes Vision, Draper, UT, USA; 3Case Western Reserve University School of Medicine, Cleveland, OH, USA; 4Rehabilitation Sciences Research Center, Zahedan University of Medical Sciences, Zahedan, Iran; 5Moran Eye Center, University of Utah, Salt Lake City, UT, USA; 6Utah Lion’s Eye Bank, Murray, UT, USA
Correspondence: Majid Moshirfar, Hoopes Vision Research Center, Hoopes Vision, 11820 S. State St. Ste. 200, Draper, UT, 84020, USA, Tel +1 801 568-0200, Fax +1 801 563-0200, Email [email protected]
Abstract: Increasing popularity and utility of epithelial thickness mapping (ETM) in keratorefractive surgery screening may begin to inappropriately devalue the use of tomography. An increasing body of research suggests that the interpretation of ETM based solely on the corneal resurfacing function may be insufficient to screen and select patients for refractive surgery. ETM and tomography are complementary and, when used together, may provide the safest and most optimal tools for keratorefractive surgery screening.
Keywords: corneal tomography, corneal topography, corneal epithelial map, SMILE, LASIK, PRK
Background
The corneal epithelial thickness map (ETM) is an increasingly popular diagnostic image among refractive surgeons due to current knowledge regarding epithelial remodeling processes in response to various corneal pathologies. ETM has demonstrated impressive reproducibility, inter-device agreement and repeatability.1–5 Research has demonstrated the value of these epithelial measurements and the significant role they can play in the preoperative screening of keratorefractive surgery candidates.4–10 However, recent research has introduced nuances to our former understanding of the corneal epithelial resurfacing function upon which ETM interpretations are based.11–15 These nuances include conditions, such as chalazia, dry eye disease, and less common keratoconic presentations, and settings, such as contact lens wear, in which inaccurate interpretations of ETM results may be generated.11–16 Furthermore, various tomographic indices have been especially valuable in keratorefractive surgery screening.17–19 Therefore, despite the increasing popularity and impressive clinical value of ETM, ETM and tomographic imaging modalities should be appraised equally in the literature. This opinion article aims to explain why ETM and tomography should be used in combination to optimize the refractive surgery screening process. Future research will continue to guide clinicians in the co-utilization of these two imaging modalities as well as novel devices.
Perspective
Poor visual outcomes after keratorefractive surgery are related to postoperative morphologic changes that often occur in undetected preoperative ectasia and biomechanical abnormalities, predisposing patients to iatrogenic corneal ectasia and surgically induced corneal weakening.20,21 The most widely known corneal risk factor of postoperative ectasia is keratoconus (KC).21–24 It has been shown that KC follows biomechanical decompensation of the cornea resulting in morphological changes (curvature, elevation, and pachymetry) in the posterior and anterior corneal surfaces, which lead to a bulging forward of the cornea.20 Anterior corneal protrusions classically cause inferior steepening of the cornea which can be measured via keratometry. The corneal epithelium adapts to these protrusions to maintain a smooth and regular corneal surface by thickening over areas of flattening and thinning over areas of steepening.8,20,25 This masking process is also known as the corneal epithelial resurfacing function and provides the foundation for interpreting ETMs. For example, ETMs have detected earlier forms of KC by identifying regions of epithelial thinning, even when normal corneal tomography systems have not detected significant anterior or posterior curvature changes characteristic of KC. Therefore, ETM commonly screens out patients who may have undergone keratorefractive surgery and subsequently developed visually impairing corneal ectasia due to undetected KC.
ETM also allows refractive surgeons to confidently select suitable candidates for surgery.6,8 Due to these impressive clinical impacts, ETM has become increasingly popular. Consequently, many surgeons may be persuaded to solely utilize AS-OCT devices to obtain ETM based on its accuracy in diagnosing KC.8,26–28 However, as discussed further, less common keratoconic and corneal presentations have been recently reported in the literature that may cause confusion due to seemingly contradictory ETM and tomographic findings based on the corneal epithelial resurfacing function.11–14,17,25 In these cases, an ophthalmologist may wonder whether to rely on ETM or tomography. Therefore, we seek to raise awareness among clinicians about the advantages and limitations of ETM and corneal tomography imaging modalities to help them make optimal decisions during preoperative evaluation.
Many less common abnormal corneal presentations suggest the combined use of corneal ETM and tomography imaging modalities. For example, central corneal flattening, which correlates with areas of reversible central focal epithelial thinning in patients with periocular masses such as chalazia, demonstrates the need to utilize both ETM and tomography since the classic interpretation of an ETM in patients with central corneal flattening would incorrectly suggest that these patients are experiencing central focal thickening per the corneal resurfacing function.11 Recent research regarding another abnormal, but common corneal pathology, dry eye disease, has shown that the reproducibility and repeatability of epithelial thickness measurements in the presence of mask-associated dry eye (MADE) may lead to false-positive results, suggesting an increased value of tomographic indices.4 Furthermore, Wardani et al reported variations from the traditional keratoconic corneal resurfacing function as they identified epithelial thickening in 12 eyes corresponding to areas of corneal steepening measured via Oculyzer tomography. These authors termed this presentation pseudo-KC and attributed its etiology to several factors, including corneal warpage, dry eyes, chronic exposure, tear film abnormalities, and subclinical anterior basement membrane dystrophy.25 However, only half of these patients wore contact lenses, decreasing the likelihood of corneal warpage.25 Therefore, asking patients to remove contact lenses for a specific amount of time prior to refractive surgery screening may not resolve the apparent discrepancy in the diagnosis of KC and pseudo-KC using ETM solely. Furthermore, the female-to-male participant ratio in the Wardani et al study was curiously 2:1, indicating a need to better understand the etiology, pathophysiology, and genetic and environmental factors underlying this pseudo-KC presentation.25
Mohammadi et al provided another example of research that suggests a need to understand the pathogenesis of KC. They identified several keratoconic presentations among 215 patients via computer-based videokeratography using the Scheimpflug camera imaging system on Pentacam, and then classified them into six categories: KC, atypical normal KC, FFKC, posterior KC, anterior KC, and pseudo-KC.12 To differentiate between these various KC subtypes, they utilized criteria that included epithelial thickness measurements, many topographic parameters, keratometry reading values, and a progression index, suggesting a need for parameters other than epithelial thickness when evaluating patients with these less common KC subtypes.12 Other studies have also suggested that tomographic measurements, such as Belin-Ambrósio enhanced ectasia total deviation index (BAD-D) and index of height decentration (IHD) parameters, play valuable roles in detecting corneal abnormalities.22,29–31 Additionally, since KC is primarily defined as an anterior bulging of the anterior and posterior corneal surfaces, often beginning with subtle changes limited only to the posterior surface, parameters which detect these subtle elevation changes, especially in the posterior corneal surface, may be more valuable in early and accurate detection of KC and KC subtypes.32 A recent study showed that corneal thickness maps measured on the Pentacam HR were more highly correlated with front and back corneal elevation maps than RTVue epithelial thickness maps.33 This further suggests that tomographic imaging systems rather than epithelial thickness maps may have an enhanced ability to determine the location of KC cones and therefore allow for safer and more effective therapeutic interventions. These findings demonstrate the immense value of tomography, the limitations of ETM, as well as the various KC derivations about which we currently lack full understanding. The safer decision to “do no harm” may be to opt patients out of keratorefractive surgery when confronted with contradictory tomographic findings and ETM interpretation based on the corneal resurfacing function.11,12,25
To illustrate this discussion, we present ETM and tomographic imaging for two patients who both underwent evaluation for keratorefractive surgery. Patient 1 shows a classic “doughnut” pattern on ETM with obvious epithelial thinning centrally (48um) and peripheral thickening (around 57um) in the left eye (Figure 1). This is consistent with the tomographic changes seen in the Pentacam enhanced ectasia display and refractive maps for patient 1 (Figure 2), indicating frank KC, and thus this patient was denied keratorefractive surgery. In contrast, patient 2 demonstrates normal ETM in both eyes (Figure 3) but with changes on Pentacam concerning for KC suspect (Figure 4), a finding that would be missed if ETM was the only imaging modality used. Patient 2 was also denied keratorefractive surgery.
 |
Figure 1 OCT pachymetry and ETM demonstrating normal epithelial thickness OD but marked thinning centrally (red arrow) and thickening peripherally (black arrows) OS in a “doughnut” pattern consistent with KC. Notes: Figures 1 and 2 present a keratorefractive surgery candidate with frank KC as observed by concordant abnormal findings on both ETM and Tomography. |
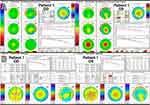 |
Figure 2 (A) Pentacam enhanced ectasia display maps demonstrating significant central thinning OU. (B) Pentacam refractive maps. Notes: Figures 1 and 2 present a keratorefractive surgery candidate with frank KC as observed by concordant abnormal findings on both ETM and Tomography. |
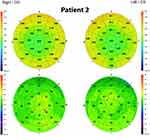 |
Figure 3 OCT pachymetry and ETM demonstrating normal epithelial thickness OU. Notes: Figures 3 and 4 present a keratorefractive surgery candidate with suspected KC as observed by discordant findings on ETM and Tomography. |
 |
Figure 4 (A) Pentacam enhanced ectasia display maps suggestive of central thinning. (B) Pentacam refractive maps. Notes: Figures 3 and 4 present a keratorefractive surgery candidate with suspected KC as observed by discordant findings on ETM and Tomography. |
In summary, ETM is an impressive and clinically valuable imaging tool that has been increasingly used in preoperative keratorefractive surgery screening due to its accuracy and precision in measuring epithelial thickness.1–3,7,9,11,34 However, due to the limited information that epithelial thickness maps can provide, especially in the context of increasing awareness of keratoconic and corneal derivations from the traditional corneal resurfacing model, valuable tomographic parameters provided by other systems must be utilized in combination with ETM for optimal clinical decision making.10–13,25 One imaging technology, the REVO NX (Optopol Technology, Zawiercie, Poland), is already moving in this direction and found to be effective in utilizing OCT scans to generate ETMs and other tomographic parameters from the same data points.35 However, more research on this device is needed to evaluate its performance with a larger number of study subjects and a greater variety of abnormal corneal presentations. Future research studies, similar to those by Silverman et al and Yücekul et al, may also strengthen the argument for the combined use of ETM and tomography, as well as provide imaging protocols that may be utilized to optimize the clinical efficacy of both modalities.5,10 Therefore, future research direction includes seeking an enhanced understanding of how to optimize the use of ETM and tomography when considering keratorefractive surgery in patients presenting with less common KC subtypes and specific ocular pathologies such as central corneal flattening associated with periocular masses or dry eye disease. These investigations may also include robust comparisons of the sensitivities and specificities of epithelial thickness measurements versus tomographic indices in the detection of KC and KC subtypes in a wide array of patients with various ocular presentations. As the presentation and pathogeneses of the various KC subtypes are studied more extensively, our knowledge of and ability to detect the signs of KC and KC subtypes, including at various stages of the disease, will be enhanced. Caution is advised in not overstating the use of ETM, lest refractive surgeons misinterpret research findings as advocating for the sole use of ETM. With these points in mind, approaching keratorefractive imaging research and surgical practice with an accurate understanding of ETM’s limitations and the value of tomographic indices in detecting keratoconic changes will lead to advancements in patient safety and long-term outcomes.
Disclosure
The authors report no conflicts of interest in this work and have no financial interests to disclose.
References
1. Georgeon C, Marciano I, Cuyaubère R, Sandali O, Bouheraoua N, Borderie V. Corneal and epithelial thickness mapping: comparison of enhanced spectral-domain-and spectral-domain-optical coherence tomography. J Ophthalmol. 2021. doi:10.1155/2021/3444083
2. Krause D, Mohr N, Shajari M, Mayer WJ, Priglinger S, Luft N. Reliability of corneal, epithelial, and stromal thickness mapping for a 9-mm zone using spectral-domain optical coherence tomography. Klin Monbl Augenheilkd. 2021;238(11):1213–1219. doi:10.1055/A-1535-1685
3. Ma JX, Wang L, Weikert MP, Montes De Oca I, Koch DD. Evaluation of the repeatability and reproducibility of corneal epithelial thickness mapping for a 9-mm zone using optical coherence tomography. Cornea. 2019;38(1):67–73. doi:10.1097/ICO.0000000000001806
4. Sella R, Zangwill LM, Weinreb RN, Afshari NA. Repeatability and reproducibility of corneal epithelial thickness mapping with spectral-domain optical coherence tomography in normal and diseased cornea eyes. Am J Ophthalmol. 2019;197:88–97. doi:10.1016/J.AJO.2018.09.008
5. Yücekul B, Dick HB, Taneri S. Systematic detection of keratoconus in OCT: corneal and epithelial thickness maps. J Cataract Refract Surg. 2022;48(12):1360–1365. doi:10.1097/J.JCRS.0000000000000990
6. Asroui L, Dupps WJ, Randleman JB. Determining the utility of epithelial thickness mapping in refractive surgery evaluations. Am J Ophthalmol. 2022;240:125–134. doi:10.1016/J.AJO.2022.02.021
7. Levy A, Georgeon C, Knoeri J, et al. Corneal epithelial thickness mapping in the diagnosis of ocular surface disorders involving the corneal epithelium: a comparative study. Cornea. 2022;41(11):1353. doi:10.1097/ICO.0000000000003012
8. Reinstein DZ, Archer TJ, Gobbe M. Corneal epithelial thickness profile in the diagnosis of keratoconus. J Refract Surg. 2009;25(7):604–610. doi:10.3928/1081597X-20090610-06
9. Salomão MQ, Hofling-Lima AL, Lopes BT, et al. Role of the corneal epithelium measurements in keratorefractive surgery. Curr Opin Ophthalmol. 2017;28(4):326–336. doi:10.1097/ICU.0000000000000379
10. Silverman RH, Urs R, RoyChoudhury A, Archer TJ, Gobbe M, Reinstein DZ. Combined tomography and epithelial thickness mapping for diagnosis of keratoconus. Eur J Ophthalmol. 2017;27(2):129–134. doi:10.5301/EJO.5000850
11. Kalas T, Gunn D. Corneal epithelial remodeling as a cause of chalazion-induced hypermetropia. Cornea. 2022;41(6):785–788. doi:10.1097/ICO.0000000000002899
12. Mohammadi SF, Mohammadzadeh V, Kadivar S, Beheshtnejad AH, Norooznezhad AH, Hashemi SH. Topographic typology in a consecutive series of refractive surgery candidates. Int Ophthalmol. 2018;38(4):1611–1619. doi:10.1007/S10792-017-0631-2
13. Santhiago MR. Patient with dissociation of corneal topography and epithelial mapping. J Cataract Refract Surg. 2021;47(12):1599. doi:10.1097/J.JCRS.0000000000000853
14. Tang M, Li Y, Chamberlain W, Louie DJ, Schallhorn JM, Huang D. Differentiating keratoconus and corneal warpage by analyzing focal change patterns in corneal topography, pachymetry, and epithelial thickness maps. Invest Ophthalmol Vis Sci. 2016;57(9):OCT544–OCT549. doi:10.1167/IOVS.15-18938
15. Tseng SSY, Hsiao JCJ, Chang DCK. Mistaken diagnosis of keratoconus because of corneal warpage induced by hydrogel lens wear. Cornea. 2007;26(9):1153–1155. doi:10.1097/ICO.0B013E318055E65C
16. Wilson SE, Lin DTC, Klyce SD, Reidy JJ, Insler MS. Topographic changes in contact lens-induced corneal warpage. Ophthalmology. 1990;97(6):734–744. doi:10.1016/S0161-6420(90)32516-2
17. Wilson SE, Klyce SD. Screening for corneal topographic abnormalities before refractive surgery. Ophthalmology. 1994;101(1):147–152. doi:10.1016/S0161-6420(94)31372-8
18. Motlagh MN, Moshirfar M, Murri MS, et al. Pentacam® corneal tomography for screening of refractive surgery candidates: a review of the literature, part I. Med Hypothesis Discov Innov Ophthalmol. 2019;8(3):177.
19. Hashem AO, Aziz BF, Wahba SS, Roshdy MM, Elawamry AI. Diagnostic accuracy of different keratoconus detection indices of pentacam in paediatric eyes. Eye. 2022;2022:1–9. doi:10.1038/s41433-022-02070-x
20. Vitar RML, Bonelli F, Rama P, Ferrari G. Nutritional and metabolic imbalance in keratoconus. Nutrients. 2022;14:4. doi:10.3390/NU14040913
21. Moshirfar M, Tukan AN, Bundogji N, et al. Ectasia after corneal refractive surgery: a systematic review. Ophthalmol Ther. 2021;10(4):753–776. doi:10.1007/S40123-021-00383-W
22. Ambrósio R, Dawson DG, Salomão M, Guerra FP, Caiado ALC, Belin MW. Corneal ectasia after LASIK despite low preoperative risk: tomographic and biomechanical findings in the unoperated, stable, fellow eye. J Refr Surg. 2010;26(11):906–911. doi:10.3928/1081597X-20100428-02
23. Randleman JB, Woodward M, Lynn MJ, Stulting RD. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology. 2008;115:1. doi:10.1016/J.OPHTHA.2007.03.073
24. Sorkin N, Kaiserman I, Domniz Y, Sela T, Munzer G, Varssano D. Risk assessment for corneal ectasia following photorefractive keratectomy. J Ophthalmol. 2017;2017:1–10. doi:10.1155/2017/2434830
25. Wardani M, Hashemi K, Aliferis K, Kymionis G. Topographic changes simulating keratoconus in patients with irregular inferior epithelial thickening documented by anterior segment optical coherence tomography. Clin Ophthalmol. 2019;13:2103–2110. doi:10.2147/OPTH.S208101
26. Yang Y, Pavlatos E, Chamberlain W, Huang D, Li Y. Keratoconus detection using OCT corneal and epithelial thickness map parameters and patterns. J Cataract Refract Surg. 2021;47(6):759–766. doi:10.1097/J.JCRS.0000000000000498
27. Schallhorn JM, Tang M, Li Y, Louie DJ, Chamberlain W, Huang D. Distinguishing between contact lens warpage and ectasia: usefulness of optical coherence tomography epithelial thickness mapping. J Cataract Refract Surg. 2017;43(1):60–66. doi:10.1016/j.jcrs.2016.10.019
28. Reinstein DZ, Gobbe M, Archer TJ, Silverman RH, Coleman J. Epithelial, stromal, and total corneal thickness in keratoconus: three-dimensional display with artemis very-high frequency digital ultrasound. J Refract Surg. 2010;26(4):259–271. doi:10.3928/1081597X-20100218-01
29. Belin MW, Khachikian SS, Ambrosio R, Salamao M. Keratoconus / ectasia detection with the oculus pentacam: belin/Ambrosio enhanced ectasia display. Highlights. 2007;35:5–12.
30. Bamdad S, Sedaghat MR, Yasemi M, Vahedi A. Sensitivity and specificity of belin Ambrosio enhanced ectasia display in early diagnosis of Keratoconus. J Ophthalmol. 2020;2020. doi:10.1155/2020/7625659
31. Belin MW, Khachikian SS. An introduction to understanding elevation-based topography: how elevation data are displayed-a review. J Refr Surg. 2008;24(9):875. doi:10.1111/j.1442-9071.2008.01821.x
32. Quisling S, Sjoberg S, Zimmerman B, Goins K, Sutphin J. Comparison of pentacam and orbscan iiz on posterior curvature topography measurements in keratoconus Eyes. Ophthalmology. 2006;113(9):1629–1632. doi:10.1016/j.ophtha.2006.03.046
33. Sedaghat MR, Momeni-Moghaddam H, Azimi Khorasani A, et al. Comparison of keratoconus cone location of different topo/tomographical parameters. Curr Eye Res. 2021;46(11):1666–1672. doi:10.1080/02713683.2021.1931343
34. Pircher N, Schwarzhans F, Holzer S, et al. Distinguishing keratoconic eyes and healthy eyes using ultrahigh-resolution optical coherence tomography-based corneal epithelium thickness mapping. Am J Ophthalmol. 2018;189:47–54. doi:10.1016/J.AJO.2018.02.006
35. Sikorski BL. Simultaneous corneal topography and epithelial thickness mapping from a single measurement using optical coherence tomography. J Ophthalmol. 2022;2022:1–12. doi:10.1155/2022/7339306
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
