Back to Journals » Orthopedic Research and Reviews » Volume 14
The Characteristic of 374 Surgically Treated Traumatic Brachial Plexus Injury Patients at an Indonesian Orthopedic Referral Hospital: An Epidemiologic and Sociodemographic View
Authors Sumarwoto T , Hadinoto SA, Kaldani F , Aprilya D , Abimanyu DR
Received 13 August 2022
Accepted for publication 6 November 2022
Published 16 November 2022 Volume 2022:14 Pages 419—428
DOI https://doi.org/10.2147/ORR.S386142
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Tito Sumarwoto,1 Seti Aji Hadinoto,1 Fathih Kaldani,1 Dina Aprilya,2 Dimitri R Abimanyu3
1Orthopaedic & Traumatology Department, Prof. Dr. R. Soeharso Orthopaedic Hospital Surakarta, Faculty of Medicine Sebelas Maret University, Surakarta, Indonesia; 2Orthopaedic & Traumatology Department, Siloam Agora Hospital, Jakarta, Indonesia; 3Faculty of Medicine Sebelas Maret University, Surakarta, Indonesia
Correspondence: Tito Sumarwoto, Orthopaedic & Traumatology Department, Prof. Dr. R. Soeharso Orthopaedic Hospital Surakarta, Faculty of Medicine Sebelas Maret University, Surakarta, Indonesia, Email [email protected]
Background: Traumatic brachial plexus injury (TBPI) is a severe injury in the upper extremity which can affect the quality of life. The incidence of these injuries has been increasing in recent years. The purpose of this study was to describe the characteristic of TBPI patients treated by surgery at a tertiary Orthopedic hospital in Surakarta, Indonesia.
Methods: This is a descriptive retrospective study of patients diagnosed with TBPI who underwent surgery between July 2013 and December 2021.
Results: This study included 374 patients with male predominance (86.10%) and an average age of 30.61 years. The most common age group was 20– 29 years (45.45% of all age groups). Traffic accidents were the most common cause of this injury (91.98%), especially motorcycle accidents (94.48% of traffic accidents). The most frequent type was complete preganglionic complete injury (48.93%). Most of the patients were the result of traction injury (96.26%). The right side (58.02%) was more common. One patient (0.27%) presented with bilateral lesions. As much as 52.67% of patients presented with concomitant injuries. Fractures were the most common concomitant injuries (90.73%). Humeral shaft fractures were the most common fractures (29.10%), followed by forearm and clavicle fractures (16.10% and 21.98% respectively). A total of 19.52% of patients underwent surgery between 3 and 6 months after trauma. Nerve procedures were performed in 57.38% of all surgical procedures and the rest were secondary procedures: Tendon transfers (36.92%), arthrodesis (2.53%), and Free Functional Muscle Transfer (FFMT) 2.74%.
Conclusion: The young population, especially men, were commonly subjected to this injury with motorcycle accidents as the most common cause. Early recognition and optimum treatment must be done to improve functional outcomes. Improvement of road safety and spreading the health education of TBPI are recommended to reduce the incidence of injury and improve functional outcomes.
Keywords: epidemiologic study, traumatic brachial plexus injury, surgical treatment, tertiary hospital
Introductions
Traumatic brachial plexus injury (TBPI) is an injury to the peripheral nerve network that makes up the brachial plexus. This devastating injury usually affects the young adult population causing motor and sensory disturbances along with pain associated with peripheral (sometimes with central) origin.1,2 Thus, it can cause significant socioeconomic losses and affect the quality of life.3–5 The poor outcome made the surgeons pessimistic and conservative treatment was the only recommended treatment in 1970. However, with the advancing microsurgery technique over the last few decades, surgery has become an important treatment in traumatic brachial plexus injury and has significantly changed the outcome of BPI.6,7
The incidence of TBPI is 10% of peripheral nerve lesions and about 14% of neurologic lesions in the upper limbs are the result of brachial plexus lesions.4,8 Furthermore, it is stated that the prevalence is about 1.2% after multiple traumatic injuries and the annual incidence is about 1.64 cases out of 100,000 people. This value may increase following the increase in the incidence of traffic accidents, especially motorcycles.9
In our experience, TBPI is not uncommon, as with other injury related to motorcycles accidents. However, delays in surgery might happen due to some misbeliefs of alternative treatments, low socioeconomic status or poor health education.10 Whereas, other than the initial extent of the injury, the functional outcome is significantly improved with the earlier time to the nerve reconstruction surgery. This is a preliminary descriptive study to emphasized the magnitude of TBPI problems in Indonesia as represent in Orthopedic Hospital Prof. Dr. R. Soeharso Surakarta which is one of orthopedic centers in Indonesia and the orthopedic referral hospital in our country. Thus, we developed a study to collect true and clear data on the sociodemographic and epidemiological characteristic of TBPI patients treated in our center from July 2013 to December 2021. The application of this data for public health is to raise the concern from both society and the government to reduce the incidence of TBPI from the enhancement of road safety as well as to shorten the period between injury and surgery in patients with surgical indication.
Materials and Methods
We retrospectively studied TBPI patients undergoing surgery at Orthopedic Hospital Prof. Dr. R. Soeharso Surakarta between April 2013 and December 2021. The inclusion criteria were TBPI patients that underwent surgery (either primary or secondary) in our center. The TBPI diagnosis was confirmed by clinical and radiological assessment (plain X-ray, Computed Tomography/CT scan, and Magnetic Resonance Imaging/MRI), as well as electrophysiological study. TBPI patient that were treated with conservative treatment, brachial plexopathy other than trauma origin, and neurological deficit with central nervous system origin were excluded.
The characteristic and demographic data were taken: gender, age, the side of the lesion, level of lesion, the injury mechanism, the time elapsed from the injury to the first management at the hospital and the surgery, and concomitant injuries. Preoperative diagnostic examinations were noted including the motoric and sensory function of the affected upper extremity, the presence of Horner syndrome, radiology, and neurophysiology examination.
The reconstructive procedures performed in our study were noted which included nerve reconstruction (primary procedures) and soft tissue reconstruction (secondary procedures). Nerve exploration and neurolysis (as needed) were performed either supraclavicular, infraclavicular, or both. Nerve transfer procedures were done to restore elbow flexion and shoulder stabilization with the donor from either intraplexal (median n., ulnar n., radial n.) or extraplexal (phrenic n., spinal accessory n., intercostal n.).11–15
The soft tissue procedures were noted in delayed cases or as the secondary procedure after nerve transfers which included tendon transfer to shoulder (SAHA procedures), elbow (Modified Steindler procedures) and wrist arthrodesis, as well as free functioning muscle transfer (FFMT).16–18 We used the gracilis muscle in all FFMT procedures. The neurovascular donors for FFMT were the phrenic nerve, transverse cervical artery, and external jugular vein.
The statistical analysis was performed using a descriptive frequency table using the IBM statistic 25 tool (SPSS Inc., Chicago, IL, USA).
Results
Sociodemographic Data
This study included 374 patients who underwent surgery for TBPI. Of these, 322 (86.10%) were males and 52 (13.90%) females. The median age of these patients was 26 years (7–77). Dividing these patients into age groups, 45.45% of patients were between 20 and 29 years of age with 86.47% of them were males (Figure 1). The male patients’ ages ranged from 7 to 77 years, while the female patients were 11–68 years old. The TBPI patients mostly came from the same province (45.20%), followed by the patients who came from the same region (32.33%), and the rest came from all over Indonesia (22.47%.)
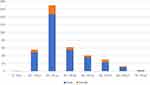 |
Figure 1 Age distribution of traumatic brachial plexus injury patient. |
Epidemiology
Among the mechanism of injury, the majority of cases were caused by traffic accidents (91.98%) which was dominated by motorcycle accidents (94.48%). Other mechanisms were domestic (5.61%) and industrial accidents (2.41%) (Table 1).
 |
Table 1 Mechanism of Traumatic Brachial Plexus Injuries |
The interval between the trauma and first surgery for the brachial plexus varied as shown in Figure 2. Based on the side of the lesion, 58.02% of the patients had right-sided injuries, 41.71% had left-sided injuries, and 1 patient (0.27%) had bilateral injuries. Traction injuries occurred in most of the patients. According to the anatomical classification, the complete pre-ganglionic type accounts for 48.93%, followed by the upper (33.15%) and complete (17.64%) post-ganglionic type. Only 1 patient (0.27%) was the lower type lesion (Table 2).
 |
Table 2 Epidemiologic Data of Traumatic Brachial Plexus Injury |
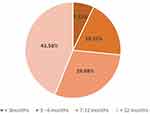 |
Figure 2 The intervals between the time of injury and the first brachial plexus surgery. |
As many as 52.67% of the patients had concomitant injuries. Fractures were the most common concomitant injuries (90.73%). Among them, most (99.07%) were closed fractures. Closed anterior dislocation of the glenohumeral joint was the second most common concomitant injury (3.38%), followed by the head/intracranial injury (3.09%), and the rest were acromioclavicular joint disruption, nerve lesion (peroneal nerve), lacerated wound, vascular rupture, crush injury, and hyphema (Table 3). Interestingly, these patients mostly visited the hospital within 24 hours after injury and were treated accordingly due to the concomitant injury. Upper limb fractures were commonly associated with TBPI (84.52%) with humerus fracture being the most common (29.10%), followed by radius (21.98%), and clavicle (16.10%) (Table 4).
 |
Table 3 Concomitant Injuries Associated with Traumatic Brachial Plexus Injury |
 |
Table 4 Fracture Associated with Traumatic Brachial Plexus Injury |
In preoperative clinical examination, Horner’s syndrome (ptosis and miosis ipsilateral) was found in 177 patients, hemidiaphragm palsy in 4 patients, and winging scapula in 17 patients. Diagnostic studies were performed to support the diagnosis. MRI examination was done in 85 patients, CT scan in 22 patients, and electrophysiological studies in 89 patients. In the preoperative predictive value analysis of root injury, at least one root abnormality of MRI was 71.28% and 70.10% of CT scans. The electrophysiological studies diagnosed 60.15% of preganglionically injured roots.
The total procedures done in this study were 474 procedures, consisting of nerve procedures, tendon transfers, arthrodesis, and free functional muscle transfer (FFMT). Nerve procedures were performed in 272 patients (57.38%) for patients who came less than 12 months. External neurolysis was performed in 42 patients (15.44%) of all nerve procedures. Among them, external neurolysis alone was performed in 4 TBPI patients that intraoperatively had a visibly intact plexus (surrounded by fibrosis) which transmitted nerve action potential (NAP) from the nerve stimulator. Nerve transfers (neurotization) were performed in 230 patients (84.56%) divided into supraclavicular neurotization for 139 patients (60.43%) and infraclavicular neurotization for 91 patients (39.57%).
In supraclavicular neurotization, intraplexal donor nerves (2 patients/1.44%) used were mainly from C5 and C6 roots. Extraplexal donor nerves were the phrenic nerve (74 patients), spinal accessories nerve/SAN (51 patients), the platysma motor branch (2 patients), and the great auricular nerve (1 patient). The nerve graft source used in this study were the sural nerve (83 patients) and the lateral antebrachial cutaneous (LABC) nerve (2 patients). The average length of used graft was 18.55 cm. The recipient nerves for these procedures were SSN (suprascapular nerve), MCN, and median nerve. In infraclavicular neurotization, Oberlin I and Oberlin II procedures were performed in 10 patients and 67 patients respectively. The Somsak Procedure was done on 14 patients.
The secondary procedures done were tendon transfer (36.92%), modified Steindler flexorplasty (32.57%), trapezius transfer procedures (59.43%), and tendon transfer for wrist, thumb, and finger extension (6.85%) Another secondary procedure was arthrodesis procedures that were performed on 12 patients (2.53%). Three joints that had already undergone surgery for arthrodesis were the glenohumeral joint (9 patients/75.0%), the wrist joint (2 patients/16.67%), and the carpometacarpal joint (1 patient/8.33%). Lastly, free functioning muscle transfer (FFMT) using gracilis muscle was performed in 13 patients (2.74%). The summary of procedures done for TBPI is presented on Table 5.
 |
Table 5 Various Reconstructive Procedures for Traumatic Brachial Plexus Injury |
Discussions
In this study, most patients were in the age group 20–29 years old and dominated by males. These results are similar to previous studies conducted in Surabaya, Indonesia,19 and some other countries such as Malaysia,20 Thailand,21 and India.22 This was due to the higher mobility for the male especially in the young adult age group. As it affects mostly young male, able-bodied individuals, this devastating injury will cause a far-reaching economic impact on both the individual and the society as illustrated by a study conducted in the United States.23
The demographic data shows that most of the patients live in the same province (Central Java) with our center. The rest of the TBPI patients came from all over Indonesia since our center is a national referral tertiary orthopedic hospital. This result showed that the specialized surgeon and facility to support the TBPI surgery was still scarce in our country which might contribute to the delayed of the treatment in addition to the lack health education in our country. However, we need to prove this in larger series.
The TBPI has been reported as a result of either blunt (mostly traction injuries related to motor vehicle accidents) or penetrating injuries.24 In a large series in 218 patients by Peach et al25 the prevalence for each mechanism included 111 traction injuries (51%), 42 gun-shot wounds (19%), and 38 stab wounds (17%). In this study, almost all patients had traction injuries with a smaller amount of direct (blunt) trauma around the shoulder. Traffic accidents were the most common cause of injury (91.98%) and motorcycle accidents dominated the traffic accident. This result corresponds with other previous studies in other developing countries where motorcycle accidents are common.20–22 Motorcycle is the most common motor vehicle accident that causes TBPI. It accounts for 100% of all motor vehicle accidents in Malaysia, 82% in Thailand, and 90% in India. As motorcycle restriction is nearly impossible to do in developing countries, the prevention of BPI should be carried out via road safety improvement.20–22
Diagnostic tools that are commonly used to adjunct the clinical diagnosis of TBPI are radiological examinations and nerve conduction studies.26 CT gradually replaced cervical myelography to identify root lesions in BPI and give a better result of nerve status in preoperative examination. MRI is non-invasive and offers detailed information on the condition of the plexus. Li et al7 presented the specificity and sensitivity of MRI for detecting root avulsion as 81.3% and 92.9% respectively. Electrophysiology examination is effective in preoperative assessment and could be revealed approximately 10–21 days after the injury.7 In our study, cervical x-ray with adjunctive CT scans were conducted when there was a possibility of neck fractures. Moreover, a combination of CT and MRI of the cervical spine was used to rule out avulsion injury. The electrophysiology examination included electromyelography and nerve conduction velocities were routinely done if the patient came in the early stage.
Surgical options were based on the time of presentation, intraoperative findings, and patients’ demands. The golden period for nerve procedure surgeries in TBPI is considered between 3 and 6 months after the accident with another 3 months delay considered as acceptable.27,28 In our study, most TBPI patients came with an onset of more than 1 year (43.58%), and only 19.52% had the first nerve reconstruction surgery in a timely manner. This result is in accordance with Suroto et al19 study conducted in another center of Indonesia, in which only 23.5% of patients received surgical treatment within six months following injury, 15.5% of patients were delayed (6–12 months), and 61.1% of patients were operated after 12 months following injury.19 This is why efforts must be taken to encourage patients, particularly in our country, to seek medical attention earlier from the time of injury.
Some studies recommend to wait for at least 3 months before surgery since spontaneous recovery might occur.1,2,11 Many studies also discourage delays longer than 6 months since long denervation times can decrease muscle strength.1,2,11 Timing is essential because nerve axons regenerate at a speed of only 1–2.5 mm per day, and denervation times include both the delay in surgery and the time before a nerve reaches its target. Most articles showed significantly better motor outcomes with delays to surgery of fewer than 6 months, with some studies specifying even shorter delays. Pain and quality of life scores were also significantly better with a shorter delay.1,2,19,29
These timeframes are the core of the treatment selection. In our study, nerve procedures were done in patients who come within 12 months after injury. However, nerve procedures can restore function effectively when performed within 6 to 9 months from injury as a time-dependent change occurs in the motor-end plate and the muscle itself, which diminishes reinnervation potential.28 The higher apoptosis activity of the proximal stump motoneuron was observed more than six months after the injury.30 Late (or secondary) reconstruction procedures (tendon transfers, arthrodesis, and FFMT) are considered to adjunct the initial nerve procedures for the residual functional deficit or for the patient who came on the later stage.
Lastly, fractures were the predominant concomitant injuries associated with BPI and were dominated by upper extremity long bone fractures, in accordance with the study by Li et al7 that fractures were presented in 76.27% of all associated injuries with upper limb fractures accounted for 65.31% of all fractures. Moreover, Terzis et al31 in 1999 revealed that fractures were associated in 57% of TBPI patients in their study and dominated with the upper extremity fractures (53.52%).
Summary
Traumatic brachial plexus injury potentially causes a great economic burden as it occurs mostly in the male population and productive age group. Traffic accidents, specifically motorcycle accidents, were the most common cause of TBPI in developing countries. Thus, the improvement of road safety will potentially reduce the incidence of TBPI. Furthermore, in this study, only a small group of patients came to seek medical attention in a timely manner. Health education about TBPI and time-strict management should be spread actively by clinicians and the government to reduce the TBPI incidence and at the same time, increase the possibility of getting a better functional outcome if the patients were treated earlier.
Ethical Approval
This study complied with the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of Prof. Dr. R. Soeharso Orthopedic Tertiary Hospital, Surakarta No: LB.02.01/XXX.3/2525/2021, April 20th, 2021.
Informed Consent
Informed consent was obtained from all individual participants and parent of under-aged patients. The privacy and personal identity information of all participants were protected.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no conflicts of interest in relation to this work.
References
1. Sinha S, Khani M, Mansoori N, Midha R. Adult brachial plexus injuries: surgical strategies and approaches. Neurol India. 2016;64(2):289–296. doi:10.4103/0028-3886.177597
2. Limthongthang R, Bachoura A, Songcharoen P, Osterman AL. Adult brachial plexus injury. Evaluation and management. Orthop Clin North Am. 2013;44(4):591–603. doi:10.1016/j.ocl.2013.06.011
3. Yang J, Qin B, Fu G. Modified pathological classification of brachial plexus root injury and its MR imaging characteristics. J Reconstr Microsurg. 2014;30(03):171–178. doi:10.1055/s-0033-1357498
4. Sakellariou VI, Badilas NK, Mazis GA, et al. Brachial plexus injuries in adults: evaluation and diagnostic approach. ISRN Orthop. 2014;2014:1–9. doi:10.1155/2014/726103
5. Dy CJ, Lingampalli N, Peacock K, Olsen MA, Ray WZ, Brogan DM. Direct cost of surgically treated adult traumatic brachial plexus injuries. J Hand Surg Glob Online. 2020;2(2):77–79. doi:10.1016/j.jhsg.2019.12.001
6. Rasulić L, Savić A, Živković B, et al. Outcome after brachial plexus injury surgery and impact on quality of life. Acta Neurochir. 2017;159(7):1257–1264. doi:10.1007/s00701-017-3205-1
7. Li GY, Xue MQ, Wang JW, Zeng XY, Qin J, Sha K. Traumatic brachial plexus injury: a study of 510 surgical cases from multicenter services in Guangxi, China. Acta Neurochir. 2019;161(5). doi:10.1007/s00701-019-03871-y
8. Park HR, Lee GS, Kim IS, Chang J-C. Brachial plexus injury in adults. Nerve. 2017;3(1):1–11. doi:10.21129/nerve.2017.3.1.1
9. Smania N, Berto G, La Marchina E, et al. Rehabilitation of brachial plexus injuries in adults and children. Eur J Phys Rehabil Med. 2012;48(3):483–506.
10. Fox M. Social determinants of health and surgery: an overview. Am Coll Surg. 2021. Available from: https://bulletin.facs.org/2021/05/social-determinants-of-health-and-surgery-An-overview/#Does_surgery_have_an_SDOH_problem. Accessed September 20, 2022.
11. Mackinnon SE, Novak CB, Myckatyn TM, Tung TH. Results of reinnervation of the biceps and brachialis muscles with a double fascicular transfer for elbow flexion. J Hand Surg Am. 2005;30(5):978–985. doi:10.1016/j.jhsa.2005.05.014
12. Maldonado AA, Bishop AT, Spinner RJ, Shin AY. Five operations that give the best results after brachial plexus injury. Plast Reconstr Surg. 2017;140(3):545–556. doi:10.1097/PRS.0000000000003620
13. Gu Y-D, Ma M-K. Use of the phrenic nerve for brachial plexus reconstruction. Clin Orthop. 1996;323:119–121. doi:10.1097/00003086-199602000-00016
14. Oberlin C, Be´al DLS, Salon A, Dauge MC, Sarcy JJ, Sarcy JJ. Nerve transfer to biceps muscle using a part Plexus:, of ulnar nerve for C5-C6 avulsion of the brachial plexus, anatomical study and report of four cases. J Hand Surg. 1994;19(A):232–237. doi:10.1016/0363-5023(94)90011-6
15. Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul PKW, Ketmalasiri W. Nerve transfer to biceps muscle using a part of the ulnar nerve in brachial plexus injury (upper arm type): a report of 32 cases. J Hand Surg. 1998;23(A):711–716. doi:10.1016/S0363-5023(98)80059-2
16. Satbhai NG, Doi K, Hattori Y, Sakamoto S. Functional outcome and quality of life after traumatic total brachial plexus injury treated by nerve transfer or single/double free muscle transfers: a comparative study. Bone Joint J. 2016;98B(2):209–217. doi:10.1302/0301-620X.98B2.35101
17. Brunelli GA, Vigasio A, Brunelli GR. Modified steindler procedure for elbow flexion restoration. J Hand Surg Am. 1995;20(5):743–746. doi:10.1016/S0363-5023(05)80424-1
18. Saha AK. Surgery of the paralyzed and flail shoulder. Acta Orthop Scand. 1967;38(sup97):97. doi:10.3109/ort.1967.38.suppl-97.01
19. Suroto H, Antoni I, Siyo A, et al. Traumatic brachial plexus injury in Indonesia: an experience from a developing country. J Reconstr Microsurg. 2021. doi:10.1055/s-0041-1735507
20. Choo P, Hasan S, Lim W, et al. Epidemiology and pattern of brachial plexus injury in Northern Malaysia; 2018. Available from:https://www.morthoj.org/supplements/moa-2019/OPH01-epidemiology-brachial-plexus.pdf. Accessed November 13, 2022.
21. Songcharoen P. Brachial plexus injury in Thailand: a report of 520 cases. Microsurgery. 1995;16(1):35–39. doi:10.1002/micr.1920160110
22. Jain DKA, Bhardwaj P, Venkataramani H, Sabapathy SR. An epidemiological study of traumatic brachial plexus injury patients treated at an Indian centre. Indian J Plast Surg. 2012;45(3):498–503. doi:10.4103/0970-0358.105960
23. Hong TS, Tian A, Sachar R, Ray WZ, Brogan DM, Dy CJ. Indirect cost of traumatic brachial plexus injuries in the United States. J Bone Joint Surg Am. 2019;101(16):E80. doi:10.2106/JBJS.18.00658
24. Lee S, Lee JW, Yeom JS, et al. A practical MRI grading system for lumbar foraminal stenosis. Am J Roentgenol. 2010;194(4):1095–1098. doi:10.2214/AJR.09.2772
25. Peach SA, Ackerman C. Results of treatment of BPIs. J Bone Joint Surg Am. 2001;83-B(Suppl 1):12.
26. Thatte M, Babhulkar S, Hiremath A. Brachial plexus injury in adults: diagnosis and surgical treatment strategies. Ann Indian Acad Neurol. 2013;16(1):26. doi:10.4103/0972-2327.107686
27. Suroto H, Wardhani IL, Haryadi RD, Aprilya D. The relationship between patient factors and clinical outcomes of free functional muscle transfer in patients with complete traumatic brachial plexus injury. Orthop Res Rev. 2022;14(June):225–233.
28. Martin E, Senders JT, DiRisio AC, Smith TR, Broekman MLD. Timing of surgery in traumatic brachial plexus injury: a systematic review. J Neurosurg. 2019;130(4):1333–1345. doi:10.3171/2018.1.JNS172068
29. Sumarwoto T, Suroto H, Mahyudin F, et al. Brachial plexus injury: recent diagnosis and management. Open Access Maced J Med Sci. 2021;9(F):13–24. doi:10.3889/oamjms.2021.5578
30. Adyaksa G, Suroto H. Apoptosis of proximal stump postganglionic brachial plexus injury, before and after six months post-trauma. Ann Med Surg. 2021;63:102156. doi:10.1016/j.amsu.2021.02.002
31. Terzis JK, Vekris MD, Soucacos PN. Outcomes of brachial plexus reconstruction in 204 patients with devastating paralysis. Plast Reconstr Surg. 1999;104(5):1221–1240. doi:10.1097/00006534-199910000-00001
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
