Back to Journals » Psychology Research and Behavior Management » Volume 16
The Association of Borderline Personality Features and Self-Injury Among Adolescents with Non-Suicidal Self-Injury: The Mediating Role of Alexithymia
Authors Liu J, Zhao K, Kang W, Tong S, Xu Y, Jin W, Qiao M, Li Y, Hong L, Yao K, Zheng T
Received 8 January 2023
Accepted for publication 12 April 2023
Published 8 May 2023 Volume 2023:16 Pages 1741—1754
DOI https://doi.org/10.2147/PRBM.S404057
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Igor Elman
Jie Liu,1,* Ke Zhao,2,* Wei Kang,1,* Siyu Tong,1 Yao Xu,1 Wei Jin,1 Mengxuan Qiao,1 Yuan Li,1 Lan Hong,3 Keqing Yao,4,5 Tiansheng Zheng6
1School of Mental Health, Wenzhou Medical University, Wenzhou, Zhejiang, People’s Republic of China; 2Lishui Second People’s Hospital Affiliated to Wenzhou Medical University, Lishui, People’s Republic of China; 3The Third Hospital of Quzhou, Quzhou, People’s Republic of China; 4Shenzhen Mental Health Center, Shenzhen, Guangdong, People’s Republic of China; 5Shenzhen Kangning Hospital, Shenzhen, Guangdong, People’s Republic of China; 6The Affiliated Kangning Hospital of Wenzhou Medical University Zhejiang Provincial Clinical Research Center for Mental Disorder, Wenzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Keqing Yao, Shenzhen Mental Health Center, Shenzhen Kangning Hospital, Shenzhen, Guangdong, People’s Republic of China, Tel +86-755-82927264, Email [email protected] Tiansheng Zheng, The Affiliated Kangning Hospital of Wenzhou Medical University Zhejiang Provincial Clinical Research Center for Mental Disorder, Wenzhou, People’s Republic of China, Email [email protected]
Introduction: Non-suicidal self-injury (NSSI) is becoming an increasingly prevalent phenomenon among adolescents, endangering their health. The aims of this study were to 1) explore the associations between borderline personality features, alexithymia and NSSI and 2) examine if alexithymia mediates the relationships between borderline personality features and both the severity of NSSI and the various functions that maintain NSSI in adolescents.
Methods: This cross-sectional study recruited 1779 outpatient and inpatient aged 12– 18 years from psychiatric hospitals. All adolescents completed a structured four-part questionnaire including demographic items, the Chinese version of the Functional Assessment of Self-Mutilation, the Borderline Personality Features Scale for Children and the Toronto Alexithymia Scale.
Results: The structural equation modelling results indicated that alexithymia partially mediated the associations between borderline personality features and both the severity of NSSI and the emotion regulation function of NSSI (B = 0.058 and 0.099, both p < 0.001), after controlling for age and sex.
Discussion: These findings suggest that alexithymia may play a role in the mechanism and treatment of NSSI among adolescents with borderline personality features. Further longitudinal studies are essential to validate these findings.
Keywords: self-harm, health, emotion regulation, structural equation modelling
Background
Non-suicidal self-injury (NSSI) refers to socially unacceptable behaviours that intentionally injure one’s body tissue without intending to commit suicide,1 including cutting, burning or scraping one’s skin, and hitting or biting oneself.2 NSSI has been included as a new research diagnosis in Part 3 of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).3 The global prevalence of NSSI among children and adolescents is approximately 19.5%.4 A recent national multicentre study using the DSM-5 diagnostic criteria reported that the overall prevalence of NSSI was 6.8% (outpatient) and 6.5% (inpatient) among Chinese population, with the highest prevalence among 13–17-year-olds (15.9%), followed by 18–22-year-olds (13.6%).5
Understanding the function behind NSSI is critical for not only assessing and determining the patient’s treatment goals but also characterizing the severity of NSSI behaviours. For example, in one study, NSSI behaviour aimed at intrapersonal functioning was found to be a significant positive predictor of NSSI severity, whereas NSSI for interpersonal functioning exhibited a significant negative association; moreover, NSSI for intrapersonal functioning significantly predicted more frequent and intense suicidal ideation, suicide planning and attempts.6 Thus, it appears that differences in NSSI functions are correlated with functional outcomes. This confirms the utility of assessing NSSI function as a measure of clinical progress.7,8 As such, NSSI function was explored in the current study. Studies7,8 suggest that NSSI function and personality structure are usually stable over time,9 and thus, we speculated that this stability in NSSI function may be related to the personality structure of the population performing NSSI behaviours. Therefore, this study explored the relationship between personality structure and NSSI.
The two-factor and the four-factor model proposed by Nock and Prinstein10 are assumed as the most plausible theoretical models of NSSI function. According to the two-factor model, the reasons for NSSI include automatic reinforcement (ie, self-reinforcement, eg, emotion regulation) and social reinforcement (ie, reinforced by others, eg, attention and avoidance).11 The four-factor functional model includes automatic positive reinforcement, automatic negative reinforcement, social positive reinforcement and social negative reinforcement. In recent studies, a well-fitting three-factor model (emotion regulation, attention seeking and social avoidance) was validated in Chinese clinical and non-clinical populations.12 Cultural differences have a considerable impact on the nature of NSSI. In the Chinese cultural context, the three-factor model showed a higher degree of fit than other model.13 The current study explores the reasons for NSSI from the perspective of this three-factor model.
The risk factors for NSSI have recently sparked the interest of scholars.1,14,15 NSSI is positively related to borderline personality features.16 Not only is adolescence a peak period for the emergence of NSSI, but borderline personality disorder symptoms peak in late adolescence, at around 14–17 years of age.17 Thus, it is crucial to consider borderline personality features when examining adolescent NSSI behaviours. Importantly, one study found a strong statistical association between NSSI and suicidal behaviour in people with borderline personality features.18 Research indicates that emotional dysregulation is a core characteristic of borderline personality disorder.19–21 Adolescents with borderline personality features often experience more negative emotions,22,23 which drive them to use NSSI as an emotion regulation strategy24–26 and to alleviate psychological distress, and this might lead to more NSSI behaviour.27 In line with this, previous studies have confirmed that emotion management is the primary function of NSSI among people with borderline personality features,28,29 and patients with emotion regulation symptoms are more likely to engage in NSSI as compared to patients with interpersonal problems.30 In addition, one study31 found that the intrapersonal function of NSSI was more closely related to borderline personality disorder symptoms, and self-injurers with borderline personality features endorsed more self-punishment, anti-suicide and anti-dissociation functions for NSSI than those without borderline personality features.
Alexithymia may be another important risk factor for NSSI. In a longitudinal study in New Zealand, the Alexithymia at baseline were significantly predictive of NSSI at five months later, which suggested that alexithymia may be a factor underlying NSSI.32 Alexithymia is a concept stemming from the field of psychosomatics.33 Individuals with alexithymia show a deficiency of words to express their affective state and find it difficult to discriminate feelings from physical sensations.34 On one hand, Previous studies have found that alexithymia is characterised by inflexible emotion regulation, with dysfunctions potentially across all stages of emotion processing, both psychologically and physiologically.35 Alexithymia is often accompanied by negative emotions. According to the emotional cascade model, the patient’s negative emotions trigger repetitive thinking, which, in turn, increases this negative emotion. This vicious cycle leads to intense negative emotional experiences, leading to extreme dissonant behaviours36 as a means to avoid these experiences, such as NSSI. In addition, in the case of mood disorders, alexithymia influences an individual’s susceptibility to the use of NSSI as an escape strategy or an alternative way to express one’s feelings.32 On the other hand, adolescents with alexithymia cannot express their emotions directly and may use self-injury to gain attention.37 In the interpersonal influence model, NSSI is used to influence or manipulate the behaviour of others in the self-injurer’s environment. It is also seen as a way of asking for help, avoiding abandonment, an attempt to be taken more seriously, or a way of influencing the behaviour of others.38
High levels of borderline personality features are not only related to NSSI but are also associated with alexithymia. The clinical descriptions of both alexithymia and borderline personality features are similar. Difficulty identifying and describing emotions are key characteristics of both borderline personality features39 and alexithymia.34 Moreover, there are many similarities in the findings related to each concept. For example, individuals with borderline personality features and those with alexithymia both exhibit negatively inclined emotional responses and impaired emotion management functions.40 Further, one study41 found a correlation between alexithymia characteristics and borderline personality features characteristics among 200 college students, while another study of college students found that individuals with borderline personality features had significant alexithymia.42
Although previous studies have suggested that borderline personality features and alexithymia are correlated with NSSI, no study has explicitly addressed the mediating effect of alexithymia on the association between borderline personality features and NSSI (including NSSI frequency and NSSI function). The harmful effects of borderline personality features might increase the severity of NSSI as well as the various functions that maintain NSSI by increasing alexithymia.
Thus, to fill this knowledge gap, the current study examined whether borderline personality features is positively associated with alexithymia and whether alexithymia mediates the associations between borderline personality features and both the severity of NSSI as well as the various functions that maintain NSSI.
Methods
Participants and Procedure
A total of 1779 participants were recruited from the psychiatric outpatient clinics or wards of 14 psychiatric hospitals or general hospitals in nine provinces in China. Participants were consecutively recruited by research assistants in clinics or wards through flyers. Recruitment occurred from December 2020 to December 2021. All participants met DSM-5 diagnostic criteria for NSSI and the following criteria: (1) age 12–18 years old, (2) at least six years of education, (3) having a history of at least one NSSI behaviour in the past 12 months. Patients were excluded if they: (1) had a previous history of schizophrenia or intellectual disability; (2) had a previous traumatic brain injury, epilepsy or other known severe neurological or organic brain diseases; and (3) had comorbidities with chronic somatic diseases, infectious diseases, immune system disorders, borderline personality disorder, eating disorder or substance abuse.
Measures
Demographics
Demographic data, including age and sex (male coded 1, female coded 2), were collected.
NSSI Behaviours
The Chinese version of the Functional Assessment of Self-Mutilation (C-FASM)12 was used to measure the frequency of each method and function of NSSI. This is a self-report scale that contains a 10-item method checklist (cutting, hitting, pulling hair, tattooing, wound-picking, pinching, biting, stabbing, scratching and head banging) and a 15-item function checklist of NSSI.12 Participants are asked to report the frequency of each endorsed NSSI behaviour. Since there is a large range in reported frequency, the variability of NSSI frequency was minimized by classifying NSSI into categories based on frequency in the past year43–45 (Calculate the number of NSSI in a year at [1365], taking the quartile of the values in the interval: 0–25% is encoded as 1 (very Less), 25–50% are encoded as 2 (occasionally), 50–75% are encoded as 3 (often), and more than 75% are encoded is 4 (frequent). In addition, direct encodings with 0 times are 0 (never), and direct encodings with more than 365 times are 4 (frequent), which forms a five-point scale answer form of 0, 1, 2, 3, 4). Research indicates that the number of ways and frequency of self-injury can indicate the severity of self-injury.46,47 For NSSI functions, participants reported their level of agreement with the 15 reasons for self-injury on a four-point Likert-type scale ranging from 0 (Never) to 3 (Always). All items were assessed in the past 12 months. The three-factor structure of NSSI function was documented: emotion regulation, attention seeking and social avoidance, according to previous research.48 Previous studies have validated C-FASM in Chinese adolescents with good content, structure validity and reliability.12 In this study, Cronbach’s α was 0.74 for the method checklist and 0.83 for the function checklist.
Borderline Personality Features
The Borderline Personality Features Scale for Children (BPFS-C) was first validated with 964 school students in China49 and has been widely applied to evaluate the borderline personality features of children and adolescents aged 8–18 years. The BPFS-C has four dimensions, including affective instability, identity problems, negative relationships and self-harm, with six items for each domain.50 Each item is measured on a Likert scale ranging from 1 (Not at all true) to 5 (Always true). The total borderline personality features score ranges from 24 to 120. In this study, Cronbach’s α was 0.90.
Alexithymia
Alexithymia was measured by the Toronto Alexithymia Scale (TAS-20).51 The TAS-20 consists of three dimensions: difficulty identifying feelings (DIF) (7 items), difficulty describing feelings (DDF) (5 items) and external-oriented thinking (EOT) (8 items). Each item is measured on a five-point Likert scale ranging from 1 (Strongly agree) to 5 (Strongly disagree). The total score ranges between 20 and 100, with higher scores indicating higher degrees of alexithymia.52,53 Previous studies have validated TAS-20 in Chinese adolescents with good content, structure validity and reliability.54 In this study, Cronbach’s α for the TAS-20 was 0.78.
Statistical Analyses
Pearson’s correlation coefficients were computed using SPSS 26 to examine the bivariate associations between the variables. To understand the relationships between borderline personality features, alexithymia, NSSI frequency and NSSI function, a mediation model was examined. Structural equation model (SEM) with maximum likelihood estimation was performed using Mplus version 8.0. Alexithymia served as the mediator between borderline personality features and both NSSI frequency and NSSI function (emotion regulation, attention seeking, social avoidance). And to understand the relationships between borderline personality features, alexithymia and NSSI methods, a mediation model was examined. Alexithymia served as the mediator between borderline personality features and NSSI methods. All tests were two-tailed and statistical significance was defined at p < 0.05. The following criteria were used to evaluate the fit of the structural equation model: comparative fit index (CFI) ≥ 0.9, Tucker–Lewis index (TLI) ≥ 0.9, root mean square error of approximation (RMSEA) < 0.06 and standardized root mean square residual (SRMR) < 0.05.55,56
Results
The mean participant age was 14.86 years (SD = 1.644). The sample comprised 317 (17.8%) boys and 1462 (82.2%) girls. Table 1 presents the descriptive statistics for NSSI frequency and NSSI function (emotion regulation, attention seeking and social avoidance). Table 2 presents the descriptive statistics of NSSI methods by gender.
 |
Table 1 Average Scores, Followed by Standard Deviation (Brackets) for Female and Male Participants on the Continuous Variables |
 |
Table 2 Descriptive Statistics of Non-Suicidal Self-Injury Methods by Gender |
Table 3 presents the correlation coefficients for the study variables. NSSI frequency was positively associated with borderline personality features, alexithymia and the three measures of NSSI function (emotion regulation, attention seeking, social avoidance). The three measures of NSSI function were all positively associated with borderline personality features and alexithymia. Borderline personality features was positively associated with alexithymia. And Table 4 presents the correlation coefficients for non-suicidal self-injury methods.
 |
Table 3 Pearson Correlation Coefficients for Study Variables |
 |
Table 4 Pearson Correlation Coefficients for Non-Suicidal Self-Injury Methods |
Figure 1 and Table 5 present the results of the mediation model with alexithymia mediating the relationships between borderline personality features and both NSSI frequency and NSSI function. The model fit indices indicated that the model was an acceptable fit (CFI = 0.927, TLI = 0.906, RMSEA = 0.055, SRMR = 0.039). The total effects of alexithymia and borderline personality features were positively associated with NSSI frequency (standardized β (STB) = 0.093 and 0.360; both p < 0.001). The total effect of Alexithymia and borderline personality features were positively associated with NSSI function-emotion regulation (STB = 0.159 and 0.536, both p < 0.001). The paths (indirect effect) from borderline personality features through alexithymia to NSSI frequency and NSSI function-emotion regulation were significant (STB = 0.058 and 0.099, both p < 0.001). In addition, the total effect of borderline personality features was positively associated with NSSI function-attention seeking and social avoidance (STB = 0.282 and 0.352, both p < 0.001). Furthermore, the total effect of age on NSSI frequency was significant (STB = −0.156, p < 0.001). The total effects of sex was also associated with NSSI frequency (STB = 0.066, p = 0.003). And the total effect of sex on emotion regulation was significant (STB = 0.129, p < 0.001). These results suggest that girls and younger participants had higher levels of borderline personality features, which led to higher NSSI frequency. Moreover, NSSI in girls was more likely to be used for emotional regulation.
 |
Table 5 Standardized Coefficients for Direct, Indirect and Total Effects from the Structural Equation Model |
Figure 2 and Table 6 present the results of the mediation model with alexithymia mediating the relationships between borderline personality features and the endorsement of NSSI method. The total effects of alexithymia was positively associated with the endorsement of cutting and biting (standardized β (STB) = −0.081 and 0.065, p =0.007 and p = 0.048, respectively). The total effects of borderline personality features was positively associated with the endorsement of all methods of NSSI, except for tattooing (STB = 0.048, p = 0.077). The paths (indirect effect) from borderline personality features through alexithymia to cutting and biting were significant (STB = −0.050 and 0.041, p =0.007 and p = 0.049, respectively). In addition, the total effect of age on cutting, tattooing biting and scraping were significant. This result indicates that younger participants had higher endorsement of cutting, lower endorsement of tattooing, biting and scraping. Furthermore, the total effect of sex was also associated with picking at a wound, biting, picking areas of body and punching walls or objects. These results suggest that the NSSI method of girl participants with highest endorsement was picking at a wound, biting, picking areas of body, and the NSSI method of boy participants with highest endorsement was punching walls or objects.
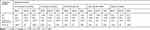 |
Table 6 Standardized Coefficients for Direct, Indirect and Total Effects from the Mediation Model |
Discussion
This study revealed several important findings. First, the severity of NSSI was significantly positively correlated with all three NSSI functions; emotion regulation exhibited the strongest correlation, followed by social avoidance and finally, attention seeking. One study57 found that NSSI to achieve emotion regulation function was more likely to lead to more frequent and severe NSSI behaviour. A follow-up study by Zanarini et al27 also found that patients with more episodes of NSSI at baseline reported more internal causes of NSSI at follow-up than patients who had fewer episodes. Therefore, it is crucial to study the different functions of NSSI and the choice of intervention modality for NSSI behaviours. These results also highlight the importance of assessing the specific functions of NSSI to identify individuals with more severe NSSI.
Second, borderline personality features was positively associated with the severity of NSSI and the three NSSI functions (emotion regulation, attention seeking and social avoidance). After controlling for TAS-20 scores, borderline personality features was still associated with NSSI function, which may mean that people with higher borderline personality features engage in NSSI more frequently for emotion regulation, attention seeking and social avoidance functions. These findings are consistent with previous studies.31,58,59 According to the emotional cascade model, negative emotions among patients with borderline personality disorder symptoms can be continuously positively reinforced by rumination, and NSSI is used as an emotion regulation strategy to divert attention and interrupt this emotional cascade.60 Another study of self-injury among college students reported that interpersonal difficulties may be an important trigger for NSSI.57 Moreover, among adolescents with borderline personality features who report significant interpersonal dysfunction, relationship conflict may be particularly prominent, leading to the triggering of more NSSI behaviours.30 Likewise, high levels of alexithymia are related to higher severity of NSSI and more frequent engagement in NSSI for emotion regulation. Alexithymia is the underlying mechanism of emotional dysregulation.41 In the face of strong negative emotions, adolescents with alexithymia are more likely to adopt suppression strategies like NSSI to interrupt the emotional cascade.61,62
Third, the structural equation model indicated that alexithymia partially mediated the associations between borderline personality features and both the severity of NSSI and the emotion regulation function of NSSI. This is similar to the findings of Sleuwaegen et al, who found that alexithymia in borderline personality disorder patients may lead to an increased tendency to engage in NSSI.40 Another study of 2261 college students also found that difficulty identifying and describing feelings may mediate the relationship between borderline personality disorder symptoms and borderline personality disorder related-behaviours like NSSI, indicating that alexithymia may exacerbate the impact of borderline personality disorder symptoms on NSSI.63 Another previous study reported that NSSI in borderline personality disorder patients is associated with alexithymia, and borderline personality disorder patients are more likely to engage in NSSI if they are confused about their feelings and have difficulty expressing them verbally.40
Fourth, this is the first study to explore the relationship between NSSI method, borderline personality features and alexithymia. We found some interesting findings regarding the frequency and endorsement of NSSI method. The NSSI method with highest endorsement was cutting, consistent with previous research.32,64 And the frequency and endorsement of all NSSI methods (except for cutting) were positively associated with borderline personality features and alexithymia. Endorsement of cutting was negative associated with borderline personality features and alexithymia. With the increase of borderline personality features and alexithymia, the endorsement of other NSSI methods increases, and adolescents take more methods of NSSI, which indirectly reduces the endorsement of cutting. In addition, the mediation model indicated that alexithymia partially mediated the associations between borderline personality features and both cutting and biting. This preliminary finding should be verified in future studies.
Finally, the results were similar to those of previous studies,65,66 we found some sex differences in NSSI. The NSSI method of girl participants with highest endorsement was picking at a wound, biting, picking areas of body. Girl participants had higher levels of borderline personality features and higher NSSI frequency. And NSSI in girls was more likely to be used for emotional regulation. Previous studies have found higher levels of rumination in girl,67 and the emotional cascade model68 states that more rumination leads to increased emotional intensity, which leads to subsequent behavioral dysregulation, such as self-injury.60
There are several limitations of this study that should be noted. First, the participants were recruited from psychiatric outpatient clinics or wards. Thus, representativeness is limited. These results should be replicated in a community sample. Further, the measures employed in this study were self-report, and thus, may be biased by social desirability factors. Another limitation is that the correlative and cross-sectional nature of this study limits the ability to make causal conclusions. As such, a prospective longitudinal design is needed to further explore the relationships between these variables. Despite these limitations, the measures used in this study are reliable and valid, and the large clinically relevant sample is a strength of this study, which reflects part of the clinical practice situation.
Conclusion
This study found that participants with higher borderline personality features had more severe NSSI and more frequent adoption of NSSI for the three functions (emotion regulation, attention seeking, social avoidance). Furthermore, alexithymia acted as a partial mediator of the relationships between borderline personality features and both the severity of NSSI and more frequent adoption of NSSI for the purpose of emotion regulation. In other words, borderline personality features may increase alexithymia which, in turn, increases the severity of NSSI as well as the emotion regulation function of NSSI. Future researchers could investigate the mediation role of alexithymia in the relationships between borderline personality features and both the severity and function of NSSI using a longitudinal design. This would enable clarification of the direction of causality. The results of our study may be useful in improving our knowledge of NSSI in adolescents and their relationship with borderline personality features and alexithymia, in order to develop effective strategies specifically designed for NSSI treatment in adolescents.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The study was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. The protocol for this study was approved by the Ethics Review Committee of Shenzhen Kangning Hospital (approval number 2020-k021-02). All subjects and their families agreed to participate in this study and provided written informed consent. This study was conducted in strict accordance with the relevant national and international regulations.
Acknowledgment
We are deeply grateful to all participants who made contributions to our study for their generous participation, and psychiatrists for their help in the recruitment of patients with non-suicidal self-injury.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by Zhejiang Provincial Natural Science Foundation of China under Grant (NO. LY22H090022), Zhejiang Provincial Medical health Project under Grant (NO. 2022520621), Wenzhou Science and Technology Bureau project under Grant (NO. Y20210761), Shenzhen Fund for Guangdong Provincial High-level Clinical Key Specialties (No. SZGSP013), Shenzhen Science and technology research and Development Fund for Sustainable development project (No. KCXFZ20201221173613036), National Innovation and Entrepreneurship Training Program for College Students (202110343060S).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Brown RC, Plener PL. Non-suicidal self-injury in adolescence. Curr Psychiatry Rep. 2017;19(3):20. doi:10.1007/s11920-017-0767-9
2. Rodríguez-Blanco L, Carballo-Belloso JJ, de León S, Baca-García E. A longitudinal study of adolescents engaged in Non-Suicidal Self Injury (NSSI): clinical follow-up from adolescence to young adulthood. Psychiatry Res. 2021;297:113711. doi:10.1016/j.psychres.2021.113711
3. Zetterqvist M. The DSM-5 diagnosis of nonsuicidal self-injury disorder: a review of the empirical literature. Child Adolesc Psychiatry Ment Health. 2015;9:31. doi:10.1186/s13034-015-0062-7
4. Lim KS, Wong CH, McIntyre RS, et al. Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: a meta-analysis. Int J Environ Res Public Health. 2019;16(22). doi:10.3390/ijerph16224581
5. Wang C, Zhang P, Zhang N. Adolescent mental health in China requires more attention. Lancet Public Health. 2020;5(12):e637. doi:10.1016/s2468-2667(20)30094-3
6. Brausch AM, Muehlenkamp JJ. Perceived effectiveness of NSSI in achieving functions on severity and suicide risk. Psychiatry Res. 2018;265:144–150. doi:10.1016/j.psychres.2018.04.038
7. Victor SE, Styer D, Washburn JJ. Functions of nonsuicidal self-injury (NSSI): cross-sectional associations with NSSI duration and longitudinal changes over time and following treatment. Psychiatry Res. 2016;241:83–90. doi:10.1016/j.psychres.2016.04.083
8. Victor SE, Styer D, Washburn JJ. Corrigendum to “Functions of nonsuicidal self-injury (NSSI): cross-sectional associations with NSSI duration and longitudinal changes over time and following treatment” [Psychiatry Res. 241 (2016) 83–90]. Psychiatry Res. 2018;270:1185. doi:10.1016/j.psychres.2018.11.053
9. Robins RW. Psychology. The nature of personality: genes, culture, and national character. Science. 2005;310(5745):62–63.
10. Nock MK, Prinstein MJ. Contextual features and behavioral functions of self-mutilation among adolescents. J Abnorm Psychol. 2005;114(1):140–146. doi:10.1037/0021-843X.114.1.140
11. Reinhardt M, Kökönyei G, Rice KG, Drubina B, Urbán R. Functions of nonsuicidal self-injury in a Hungarian community adolescent sample: a psychometric investigation. BMC Psychiatry. 2021;21(1):618. doi:10.1186/s12888-021-03613-4
12. Qu D, Wang Y, Zhang Z, et al. Psychometric properties of the Chinese version of the Functional Assessment of Self-Mutilation (FASM) in Chinese clinical adolescents. Front Psychiatry. 2022;12:755857. doi:10.3389/fpsyt.2021.755857
13. You J, Lin M-P, Leung F. Functions of nonsuicidal self-injury among Chinese community adolescents. J Adolesc. 2013;36(4):737–745. doi:10.1016/j.adolescence.2013.05.007
14. Barrocas AL, Giletta M, Hankin BL, Prinstein MJ, Abela JRZ. Nonsuicidal self-injury in adolescence: longitudinal course, trajectories, and intrapersonal predictors. J Abnorm Child Psychol. 2015;43(2):369–380. doi:10.1007/s10802-014-9895-4
15. Fox KR, Franklin JC, Ribeiro JD, Kleiman EM, Bentley KH, Nock MK. Meta-analysis of risk factors for nonsuicidal self-injury. Clin Psychol Rev. 2015;42:156–167. doi:10.1016/j.cpr.2015.09.002
16. Jacobson CM, Muehlenkamp JJ, Miller AL, Turner JB. Psychiatric impairment among adolescents engaging in different types of deliberate self-harm. J Clin Child Adolesc Psychol. 2008;37(2):363–375. doi:10.1080/15374410801955771
17. Courtney-Seidler EA, Klein D, Miller AL. Borderline personality disorder in adolescents. Clin Psychol. 2013;20(4):425–444. doi:10.1111/cpsp.12051
18. Alberdi-Páramo I, Díaz-Marsá M, Sáiz González MD, Carrasco Perera JL. Association between non-suicidal self-injury and suicidal behavior in Borderline Personality Disorder: a retrospective study. Actas Esp Psiquiatr. 2021;49(5):199–204.
19. Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: elaborating and extending Linehan’s theory. Psychol Bull. 2009;135(3):495–510. doi:10.1037/a0015616
20. Jacob GA, Ower N, Buchholz A. The role of experiential avoidance, psychopathology, and borderline personality features in experiencing positive emotions: a path analysis. J Behav Ther Exp Psychiatry. 2013;44(1):61–68. doi:10.1016/j.jbtep.2012.07.006
21. Kuo JR, Fitzpatrick S, Metcalfe RK, McMain S. A multi-method laboratory investigation of emotional reactivity and emotion regulation abilities in borderline personality disorder. J Behav Ther Exp Psychiatry. 2016;50:52–60. doi:10.1016/j.jbtep.2015.05.002
22. Chapman AL. Borderline personality disorder and emotion dysregulation. Dev Psychopathol. 2019;31(3):1143–1156. doi:10.1017/S0954579419000658
23. McLachlan J, Mehdikhani M, Larham B, Centifanti LCM. Borderline personality traits and emotion regulation strategies in adolescents: the role of implicit theories. Child Psychiatry Hum Dev. 2022;53(5):899–907. doi:10.1007/s10578-021-01169-8
24. Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G, Weinberg I, Gunderson JG. The 10-year course of physically self-destructive acts reported by borderline patients and axis II comparison subjects. Acta Psychiatr Scand. 2008;117(3):177–184. doi:10.1111/j.1600-0447.2008.01155.x
25. Goodman M, Tomas IA, Temes CM, Fitzmaurice GM, Aguirre BA, Zanarini MC. Suicide attempts and self-injurious behaviours in adolescent and adult patients with borderline personality disorder. Personal Ment Health. 2017;11(3):157–163. doi:10.1002/pmh.1375
26. Groschwitz RC, Plener PL, Kaess M, Schumacher T, Stoehr R, Boege I. The situation of former adolescent self-injurers as young adults: a follow-up study. BMC Psychiatry. 2015;15:160. doi:10.1186/s12888-015-0555-1
27. Zanarini MC, Laudate CS, Frankenburg FR, Wedig MM, Fitzmaurice G. Reasons for self-mutilation reported by borderline patients over 16 years of prospective follow-up. J Pers Disord. 2013;27(6):783–794. doi:10.1521/pedi_2013_27_115
28. Kleindienst N, Bohus M, Ludäscher P, et al. Motives for nonsuicidal self-injury among women with borderline personality disorder. J Nerv Ment Dis. 2008;196(3):230–236. doi:10.1097/NMD.0b013e3181663026
29. Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. J Abnorm Psychol. 2002;111(1):198–202.
30. Sadeh N, Londahl-Shaller EA, Piatigorsky A, et al. Functions of non-suicidal self-injury in adolescents and young adults with Borderline Personality Disorder symptoms. Psychiatry Res. 2014;216(2):217–222. doi:10.1016/j.psychres.2014.02.018
31. Vega D, Torrubia R, Soto À, et al. Exploring the relationship between non suicidal self-injury and borderline personality traits in young adults. Psychiatry Res. 2017;256:403–411. doi:10.1016/j.psychres.2017.07.008
32. Garisch JA, Wilson MS. Prevalence, correlates, and prospective predictors of non-suicidal self-injury among New Zealand adolescents: cross-sectional and longitudinal survey data. Child Adolesc Psychiatry Ment Health. 2015;9:28. doi:10.1186/s13034-015-0055-6
33. Hemming L, Haddock G, Shaw J, Pratt D. Alexithymia and its associations with depression, suicidality, and aggression: an overview of the literature. Front Psychiatry. 2019;10:203. doi:10.3389/fpsyt.2019.00203
34. Gramaglia C, Gambaro E, Zeppegno P. Alexithymia and treatment outcome in anorexia nervosa: a scoping review of the literature. Front Psychiatry. 2019;10:991. doi:10.3389/fpsyt.2019.00991
35. Panayiotou G, Panteli M, Vlemincx E. Adaptive and maladaptive emotion processing and regulation, and the case of alexithymia. Cogn Emot. 2021;35(3):488–499. doi:10.1080/02699931.2019.1671322
36. Selby EA, Anestis MD, Joiner TE. Understanding the relationship between emotional and behavioral dysregulation: emotional cascades. Behav Res Ther. 2008;46(5):593–611.
37. Lumley MA. Alexithymia, emotional disclosure, and health: a program of research. J Pers. 2004;72(6):1271–1300.
38. Hepp J, Störkel LM, Wycoff AM, Freeman LK, Schmahl C, Niedtfeld I. A test of the interpersonal function of non-suicidal self-injury in daily life. Behav Res Ther. 2021;144:103930. doi:10.1016/j.brat.2021.103930
39. Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. Guilford Press; 1993:xvii, 558–xvii, 558.
40. Sleuwaegen E, Houben M, Claes L, Berens A, Sabbe B. The relationship between non-suicidal self-injury and alexithymia in borderline personality disorder: “Actions instead of words”. Compr Psychiatry. 2017;77:80–88. doi:10.1016/j.comppsych.2017.06.006
41. Ridings LE, Lutz-Zois CJ. Emotional dysregulation and borderline personality disorder: explaining the link between secondary psychopathy and alexithymia. Pers Individ Dif. 2014;57:14–19.
42. Webb D, McMurran M. Emotional intelligence, alexithymia and borderline personality disorder traits in young adults. Personal Ment Health. 2008;2(4):265–273.
43. Burke TA, Ammerman BA, Hamilton JL, Alloy LB. Impact of non-suicidal self-injury scale: initial psychometric validation. Cognit Ther Res. 2017;41(1):130–142. doi:10.1007/s10608-016-9806-9
44. Hasking PA, Coric SJ, Swannell S, Martin G, Thompson HK, Frost ADJ. Brief report: emotion regulation and coping as moderators in the relationship between personality and self-injury. J Adolesc. 2010;33(5):767–773. doi:10.1016/j.adolescence.2009.12.006
45. Hamza CA, Willoughby T. A longitudinal person-centered examination of nonsuicidal self-injury among university students. J Youth Adolesc. 2014;43(4):671–685. doi:10.1007/s10964-013-9991-8
46. Victor SE, Klonsky ED. Correlates of suicide attempts among self-injurers: a meta-analysis. Clin Psychol Rev. 2014;34(4):282–297. doi:10.1016/j.cpr.2014.03.005
47. Anestis MD, Khazem LR, Law KC. How many times and how many ways: the impact of number of nonsuicidal self-injury methods on the relationship between nonsuicidal self-injury frequency and suicidal behavior. Suicide Life Threat Behav. 2015;45(2):164–177. doi:10.1111/sltb.12120
48. Wang Y, Zhou X, Cao B, et al. The psychological characteristics and risk factors of suicidal attempt among mood disorders adolescents accompany with non-suicidal self-injury: a multi-center study. J Affect Disord. 2022;298(Pt A):301–307. doi:10.1016/j.jad.2021.10.130
49. Liu P, Wang X. Evaluation of reliability and validity of Chinese-version borderline personality features scale for children. Med Sci Monit. 2019;25:3476–3484. doi:10.12659/MSM.912662
50. Crick NR, Murray-Close D, Woods K. Borderline personality features in childhood: a short-term longitudinal study. Dev Psychopathol. 2005;17(4):1051–1070.
51. Taylor GJ, Ryan D, Bagby RM. Toward the development of a new self-report alexithymia scale. Psychother Psychosom. 1985;44(4):191–199.
52. Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale--I. Item selection and cross-validation of the factor structure. J Psychosom Res. 1994;38(1):23–32.
53. Bagby RM, Parker JDA, Taylor GJ. Twenty-five years with the 20-item Toronto Alexithymia Scale. J Psychosom Res. 2020;131:109940. doi:10.1016/j.jpsychores.2020.109940
54. Ling Y, Zeng Y, Yuan H, Zhong M. Cross-cultural validation of the 20-item Toronto Alexithymia Scale in Chinese adolescents. J Psychiatr Ment Health Nurs. 2016;23(3–4):179–187. doi:10.1111/jpm.12298
55. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. doi:10.1080/10705519909540118
56. Hooper D, Coughlan JP, Mullen MR. Structural equation modelling: guidelines for determining model fit. Electron J Bus Res Methods. 2008;6:53–60.
57. Muehlenkamp J, Brausch A, Quigley K, Whitlock J. Interpersonal features and functions of nonsuicidal self-injury. Suicide Life Threat Behav. 2013;43(1):67–80. doi:10.1111/j.1943-278X.2012.00128.x
58. Iskric A, Ceniti AK, Bergmans Y, McInerney S, Rizvi SJ. Alexithymia and self-harm: a review of nonsuicidal self-injury, suicidal ideation, and suicide attempts. Psychiatry Res. 2020;288:112920. doi:10.1016/j.psychres.2020.112920
59. Zareen G, Ashraf F. Sub-clinical borderline personality disorder symptoms as predictor of suicidality and non-suicidal self-injury in young Pakistani females. J Pak Med Assoc. 2021;71(2(b)):740–743. doi:10.47391/jpma.1088
60. Selby EA, Joiner TE. Cascades of emotion: the emergence of borderline personality disorder from emotional and behavioral dysregulation. Rev Gen Psychol. 2009;13(3):219.
61. Chen J, Xu T, Jing J, Chan RCK. Alexithymia and emotional regulation: a cluster analytical approach. BMC Psychiatry. 2011;11:33. doi:10.1186/1471-244X-11-33
62. Richmond S, Hasking P, Meaney R. Psychological distress and non-suicidal self-injury: the mediating roles of rumination, cognitive reappraisal, and expressive suppression. Arch Suicide Res. 2017;21(1):62–72. doi:10.1080/13811118.2015.1008160
63. Meaney R, Hasking P, Reupert A. Borderline personality disorder symptoms in college students: the complex interplay between alexithymia, emotional dysregulation and rumination. PLoS One. 2016;11(6):e0157294. doi:10.1371/journal.pone.0157294
64. Ammmerman BA, Hong M, Sorgi K, Park Y, Jacobucci R, McCloskey MS. An examination of individual forms of nonsuicidal self-injury. Psychiatry Res. 2019;278:268–274. doi:10.1016/j.psychres.2019.06.029
65. Bresin K, Schoenleber M. Gender differences in the prevalence of nonsuicidal self-injury: a meta-analysis. Clin Psychol Rev. 2015;38:55–64. doi:10.1016/j.cpr.2015.02.009
66. Zetterqvist M, Lundh L-G, Dahlström O, Svedin CG. Prevalence and function of non-suicidal self-injury (NSSI) in a community sample of adolescents, using suggested DSM-5 criteria for a potential NSSI disorder. J Abnorm Child Psychol. 2013;41(5):759–773. doi:10.1007/s10802-013-9712-5
67. Nolen-Hoeksema S. Emotion regulation and psychopathology: the role of gender. Annu Rev Clin Psychol. 2012;8:161–187. doi:10.1146/annurev-clinpsy-032511-143109
68. Selby EA, Anestis MD, Bender TW, Joiner TE. An exploration of the emotional cascade model in borderline personality disorder. J Abnorm Psychol. 2009;118(2):375–387. doi:10.1037/a0015711
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


