Back to Journals » Research and Reports in Urology » Volume 6
The association of age of toilet training and dysfunctional voiding
Authors Hodges S, Richards K, Gorbachinsky I, Krane LS
Received 26 April 2014
Accepted for publication 30 June 2014
Published 3 October 2014 Volume 2014:6 Pages 127—130
DOI https://doi.org/10.2147/RRU.S66839
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Video abstract presented by Steve J Hodges.
Views: 1102
Steve J Hodges, Kyle A Richards, Ilya Gorbachinsky, L Spencer Krane
Department of Urology, Wake Forest University, Winston-Salem, NC, USA
Objective: To determine whether age of toilet training is associated with dysfunctional voiding in children.
Materials and methods: We compared patients referred to the urologic clinics for voiding dysfunction with age-matched controls without urinary complaints. Characteristics including age and reason for toilet training, method of training, and encopresis or constipation were compared between both groups.
Results: Initiation of toilet training prior to 24 months and later than 36 months of age were associated with dysfunctional voiding. However, dysfunctional voiding due to late toilet training was also associated with constipation.
Conclusion: Dysfunctional voiding may be due to delayed emptying of the bowel and bladder by children. The symptoms of dysfunctional voiding are more common when toilet training early, as immature children may be less likely to empty in a timely manner, or when training late due to (or in association with) constipation.
Keywords: voiding dysfunction, constipation
Introduction
The majority of the evidence in the literature points to an association between later toilet training and dysfunctional voiding. However, no clear hypothesis has been put forth or tested as to why this would occur. Paradoxically, all our physiological models point to the uninhibited voiding typical of infants in diapers as beneficial to bladder development and compliance. In fact, it has been demonstrated that bladder growth continues in infants up to the point of toilet training.1 Conversely, models of inhibited voiding (which mimic a toilet trained child delaying voiding), demonstrate the development of bladder dysfunction and overactivity.2 A possible explanation of the discordance between the published studies and our physiological models is that undiagnosed constipation plays a role in the higher incidence of dysfunctional voiding in children training late. We hypothesize that dysfunctional voiding is more likely to develop in children trained early or children trained late due to (or in association with) constipation.
Methods
The Wake Forest University School of Medicine Institutional Review Board approved this case-control prospective study (IRB00013101 – October 12, 2010). Cases consisted of children between the ages of 3 and 10 years old who presented to the pediatric urology clinic over a 6-month period for treatment of dysfunctional voiding. Patients were considered to have dysfunctional voiding if they presented with symptoms of non-neurogenic daytime urinary incontinence, urinary frequency, and/or urgency. Patients were considered to have constipation if they had any of the following findings: encopresis, the Rome 3 criteria for functional constipation, bowel movements consistent with Bristol Stool scale types 1–2, grossly decreased level of perception and increased tolerance to balloon insufflation in the presence of normal rectoanal relaxation on rectal manometry, and/or radiographic evidence of rectal stool (>3 cm transverse diameter). The control group included children recruited from a general pediatric clinic and pediatric emergency room in the same geographic area that did not have a history of dysfunctional voiding. Patients with anatomic malformations of the urinary tract, diabetes mellitus, proteinuria, or a history of neurological conditions were excluded from the study.
For cases and controls, information was gathered via questionnaire regarding age of child, sex, age of toilet training, reason for initiation of training, use of timed voiding as a training method, presence of day or night incontinence, urgency, parent-reported constipation, and encopresis. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Pearson’s chi-squared test was used to compare categorical variables, with a P-value of <0.05 considered statistically significant. Nonparametric testing was used to compare continuous data. Univariate nominal logistic regression analysis was used to create odds ratios. Statistical analysis was performed using JMP 9.0 (SAS Institute Inc., Cary, NC, USA).
Results
A total of 112 patients were included in this study. Table 1 demonstrates demographics associated with the patient cohort. A total of 61 (54%) patients were male. The majority of patients initiated toilet training between the ages of 24 and 36 months. Overall, 38% (43) patients had parents who reported a history of constipation, and 50 (45%) of patients reported daytime wetting.
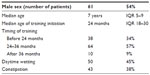  | Table 1 Demographics |
When grouping patients based on early, normal or late training, a significantly larger proportion of patients in the early and late groupings had complaints of daytime wetness as compared with the normal group (P=0.004). In addition to this, these patients also had higher rates of constipation than the normal group (P=0.002) (Table 2). Using a univariate logistic regression analysis, patients who trained early were 3.33 (95% confidence interval [CI] 1.43–7.95, P=0.005) times more likely to complain of constipation than the normal group. Patients who trained late also reported more constipation than the normal group, with an OR of 7.00 (95% CI 1.73–35.76, P=0.006). Early trainers had a 3.37-times increased risk of daytime wetness (95% CI 1.48–7.95, P=0.004) as compared with the normal group. This was also found in patients who trained late (OR 5.13, 95% CI 1.28–25.77, P=0.020). Male sex (OR 1.03, P=0.92) and current age (OR 1.22 per year increase in age, P=0.75) were not associated with either daytime wetness or constipation.
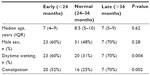  | Table 2 Comparison of toilet training ages |
Discussion
Many theories exist regarding the development of dysfunctional elimination syndrome in children. A historical belief was that a congenital urethral obstruction was the cause, and urethral dilation was the standard therapy.3 This presumed congenital urethral abnormality was later determined to actually be a dyssynergic contraction of the external sphincter, and the therapy of choice became pelvic floor physical therapy.4 Whether pelvic floor dyssynergia is congenital or acquired is still up for debate.
Interestingly, most of the literature examining toilet training and dysfunctional elimination associate late training with bladder overactivity, and therefore actually promote early training as a possible preventative measure.5–10
This seems counterintuitive for several reasons. First, anecdotally (and now we have demonstrated statistically) many of our patients with dysfunctional elimination are children who trained early and easily. The progressive bladder growth in pretoilet-trained children (with increasing compliance), which decreases abruptly at the age of toilet training, also seems to imply that the infantile period of uninhibited voiding in diapers is beneficial to bladder growth.1 Another example is the bladder in children with cerebral palsy, who (if they have no sphincter dyssynergia) maintain an infantile voiding pattern and progressive bladder growth.11 If uninhibited voiding leads to bladder growth, then the opposite may lead to decreasing bladder growth and compliance. We have numerous examples of inhibited or delayed voiding (such as posterior urethral valves), which lead to the development of uninhibited bladder contractions, as well as lower bladder capacity and compliance. Yet another example is the neurogenic bladder that develops in myelodysplastic patients.12–14 The volitional delaying of voiding strains the bladder in much the same way as anatomic obstruction, which results in decreasing compliance and uninhibited bladder contractions – the hallmarks of the dysfunctional voiding.
Thus, early training with delayed emptying in children may lead to dysfunctional elimination; however, the evidence that late training is also associated with dysfunctional elimination has led some authors to hypothesize that a “magic window” exists for toilet training around the age of 2 years old.8 How can this be explained?
It turns out that history may hold the answer. In the 1960s, scientists began to document the presence of urinary symptoms in children with Hirschsprung’s disease.15 O’Regan et al furthered this work with several groundbreaking studies linking rectal distention to bladder overactivity, with excellent success in treating voiding dysfunction simply by treating constipation.16–19
Scientists also noticed a high incidence of abnormal anal electromyograms in children with voiding dysfunction,20 and O’Regan et al17 demonstrated that in constipated children there is a maintenance of rectal sphincter contraction to maintain fecal continence causing concomitant urethral sphincter contraction.
We speculate that late training is associated with dysfunctional elimination because this population includes children who were already constipated, and therefore their training became more lengthy and difficult, but once trained led to dysfunctional voiding symptoms.
Our results linking constipation with both early and late populations with increased incidence of dysfunctional voiding perhaps imply that constipation, and not the age of training per se, is most important to the development of voiding dysfunction in children.
These findings suggest an aggressive evaluation for constipation in children with dysfunctional elimination, using not only simple questions regarding the timing and consistency of bowel movements, but also abdominal radiographs or anorectal manometry to diagnose rectal distention (even in cases without symptoms of functional constipation).
Disclosure
The authors report no conflicts of interest in this work.
References
Zerin JM, Chen E, Ritchey ML, Bloom DA. Bladder capacity as measured at voiding cystourethrography in children: relationship to toilet training and frequency of micturition. Radiology. 1993;187:803–806. | |
Frimberger D, Cheng E, Kropp BP. The current management of the neurogenic bladder in children with spina bifida. Pediatr Clin North Am. 2012;59:757–767. | |
Milanovic D, Sremcevic D, Perovic S, Scepanovic D, Krstic Z. [Stenosis of the external urethral opening as one of the causes of recurrent urinary infections in girls – surgical treatment]. Acta Chir Iugosl. 1989;36:229–237. Serbian. | |
Palmer LS. Biofeedback in the management of urinary continence in children. Curr Urol Rep. 2010;11:122–127. | |
Hellstrom AL, Sillen U. [Early potty training advantageous in bladder dysfunction. Decreases the risk of urinary infection]. Lakartidningen. 2001;98:3216–3219. Swedish. | |
Bakker E, Wyndaele JJ. Changes in the toilet training of children during the last 60 years: the cause of an increase in lower urinary tract dysfunction? BJU Int. 2000;86:248–252. | |
Barone JG, Jasutkar N, Schneider D. Later toilet training is associated with urge incontinence in children. J Pediatr Urol. 2009;5:458–461. | |
Bakker E, Van Gool JD, Van Sprundel M, Van Der Auwera C, Wyndaele JJ. Results of a questionnaire evaluating the effects of different methods of toilet training on achieving bladder control. BJU Int. 2002;90:456–461. | |
Rugolotto S, Sun M, Ball T, Boucke L, de Vries M. A surging new interest on toilet training started during the first months of age in Western countries. Tech Coloproctol. 2007;11:162–163. | |
Joinson C, Heron J, Von Gontard A, Butler U, Emond A, Golding J. A prospective study of age at initiation of toilet training and subsequent daytime bladder control in school-age children. J Dev Behav Pediatr. 2009;30:385–393. | |
Richardson I, Palmer LS. Clinical and urodynamic spectrum of bladder function in cerebral palsy. J Urol. 2009;182:1945–1948. | |
Hodges SJ, Patel B, McLorie G, Atala A. Posterior urethral valves. ScientificWorldJournal. 2009;9:1119–1126. | |
Chung DE, Sandhu JS. Overactive bladder and outlet obstruction in men. Curr Urol Rep. 2011;12:77–85. | |
Madersbacher H. Neurogenic bladder dysfunction in patients with myelomeningocele. Curr Opin Urol. 2002;12:469–472. | |
Shopfner CE. Urinary tract pathology associated with constipation. Radiology. 1968;90:865–877. | |
O’Regan S, Schick E, Hamburger B, Yazbeck S. Constipation associated with vesicoureteral reflux. Urology. 1986;28:394–396. | |
O’Regan S, Yazbeck S, Hamberger B, Schick E. Constipation a commonly unrecognized cause of enuresis. Am J Dis Child. 1986;140:260–261. | |
O’Regan S, Yazbeck S, Schick E. Constipation, bladder instability, urinary tract infection syndrome. Clin Nephrol. 1985;23:152–154. | |
O’Regan S, Yazbeck S. Constipation: a cause of enuresis, urinary tract infection and vesico-ureteral reflux in children. Med Hypotheses. 1985;17:409–413. | |
Bailey JA, Powers JJ, Waylonis GW. A clinical evaluation of electromyography of the anal sphincter. Arch Phys Med Rehabil. 1970; 51:403–408. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
