Back to Journals » International Journal of General Medicine » Volume 15
The Association Between Sagittal Spinopelvic Alignment and Persistent Low Back Pain After Posterior Lumbar Interbody Fusion for Treatment of Mild L5-S1 Spondylolisthesis: A Retrospective Study
Authors Yuan JJ, Li G, Liu Y, Zhang Q, Ren ZS, Tian R
Received 20 December 2021
Accepted for publication 13 April 2022
Published 10 May 2022 Volume 2022:15 Pages 4807—4816
DOI https://doi.org/10.2147/IJGM.S353797
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Jian-Jun Yuan,* Guang Li,* Yan Liu, Quan Zhang, Zhi-Shuai Ren, Rong Tian
Department of Spinal Surgery, Tianjin Union Medical Center, Tianjin, 300121, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jian-Jun Yuan, Department of Spinal Surgery, Tianjin Union Medical Center, No. 190 Jieyuan Road, Hongqiao District, Tianjin, 300121, People’s Republic of China, Tel +86 18602663218, Fax +86 022-27557256, Email [email protected]
Introduction: The aim of this study was to explore the association between sagittal spinopelvic alignment and persistent low back pain (PLBP) following posterior decompression and instrumented fusion for mild L5-S1 spondylolisthesis.
Methods: By retrieving medical records from January 2015 to April 2020, 200 patients following PLIF for mild L5-S1 spondylolisthesis were retrospectively reviewed. Patients were divided into two groups: PLBP group and non-PLBP group. The baseline characteristics and radiographic parameters were analyzed and compared between groups.
Results: The PLBP group comprised 26 patients, and the non-PLBP group comprised 174 patients. No significant differences in preoperative spinopelvic parameters were found between the two groups (p > 0.05). There were statistically significant differences between the preoperative and postoperative variations of LL, SL, LSA, SD, and HOD spinopelvic parameters, regardless of group (p < 0.05). Postoperative PT and SS differed significantly between the PLBP group and non-PLBP group (p < 0.05). In the PLBP group, there were no significant differences between preoperative and postoperative PT; the same applied to SS. However, significant differences were found for the variations in preoperative and postoperative PT and SS between the two groups. The ΔPT was found as an independent risk factor for postoperative PLBP.
Conclusion: Patients with mild L5-S1 spondylolisthesis with PLBP after posterior lumbar spinal fusion had decreased SS and increased PT.
Keywords: sagittal spinopelvic alignment, persistent low back pain, mild L5-S1 spondylolisthesis, posterior lumbar spinal fusion
Introduction
Lumbar spondylolisthesis is the forward slippage of the vertebral body and is a common spinal disease leading to low back pain and neuropathic leg pain. It typically occurs in the lumbosacral region.1 With the progression of vertebral slippage, the sagittal spinopelvic alignment tends to undergo a series of changes.2 Normal sagittal spinopelvic alignment is helpful to maintaining a stable posture. Conversely, abnormal sagittal spinopelvic alignment may disturb the normal spinopelvic sagittal balance and result in a negative clinical outcome. In patients with persistent symptomatology or conservative management failure, surgical treatment should be considered. The most common surgical procedures are posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF).3 The purpose of surgery for lumbar spondylolisthesis is to rectify sagittal spinopelvic alignment; it consists of reducing forward slippage by posterior translation, correcting lordosis of the kyphotic segmental angle, and restoring the height of the intervertebral disc.4 The restoration of sagittal spinal balance has been directly related to reduction of pain and improvement of function. Although most patients have satisfactory clinical outcomes, many patients still complain of adjacent segment degeneration and postoperative persistent low back pain (PLBP).5,6
To date, most studies have focused on PLBP after PLIF for treatment of high-grade isthmic and degenerative spondylolisthesis. The postoperative change of sagittal balance parameters affecting PLBP in mild spondylolisthesis remains unclear. We therefore evaluated the changes in abnormal preoperative and/or postoperative sagittal spinopelvic parameters after surgical correction of adult mild L5-S1 spondylolisthesis to determine which aspect of spinopelvic sagittal alignment most affects postoperative PLBP.
Materials and Methods
Study Design and Population
We performed a retrospective study involving 215 patients recruited from the Department of Spinal Surgery, Tianjin Union Medical Center, between January 2015 and April 2020. All patients had mild L5-S1 spondylolisthesis (Meyerding class I or II) according to the Meyerding classification and had undergone posterior lumbar spinal fusion with pedicle screw systems (with or without interbody fusion) and had suffered postoperative PLBP. To be eligible for study inclusion, patients had to have a clinical and radiographic follow-up at 12 months; 15 patients who did not complete the follow-up were therefore dropped from the study. Participants were provided with detailed information about the study. Patient characteristics collected included age, gender, body mass index (BMI), age, preoperative and postoperative numeric rating scale (NRS), Oswestry Disability Index score (ODI), hospital stays, and follow-up. The radiographic parameters collected were as follows: pelvic incidence (PI), pelvic tilt (PT), lumbar lordosis (LL), sacral slope (SS), segmental lordosis (SL), lumbosacral angle (LSA), slip degree (SD), and height of intervertebral disk (HOD). In cases where postoperative PLBP was reported, NRS and ODI was used to evaluate the severity. Postoperative PLBP was defined as an NRS score reduction of less than 50% for more than 6 months and with no improvement after conservative treatment.13 The patients were divided into an experimental group and a control group according to the presence or absence of postoperative PLBP.
Inclusion and Exclusion Criteria
The inclusion criteria for patients were as follows: (1) age between 18 and 70 years, (2) diagnosis of mild L5-S1 spondylolisthesis according to the Meyerding classification, (3) completion of posterior lumbar spinal fusion with pedicle screw systems with or without interbody fusion, and (4) complete clinical data with follow-up period of more than 12 months. Subjects were excluded if they had (1) spinal fracture, spinal tumor, or previous spinal fusion; (2) history of disorder of pelvis, hip joint, or other area, which might affect the spinopelvic parameters; (3) contraindication for radiographic exposure (eg, pregnancy, fracture, or tumor); or (4) pelvic deformity, significant lower limb discrepancy, or any other condition that might affect the radiographic measurements.
Clinical Measurements
Spinopelvic parameters were measured on preoperative and postoperative lateral radiographs of the lumbosacral spine, which were taken with the arms in the fists-on-clavicles position (ie, elbows fully flexed with fists resting on the clavicles) and with knees and hips fully extended in a standing position. All radiological parameters were measured by a single author and the spinopelvic parameters (PI, PT, LL, SS, SL, LSA, SD, and HOD) were carefully measured using the tools in the online INFINITT PACS (Figures 1 and 2).5
 |
Figure 1 Measurement of spinopelvic parameters, including pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS) on a lateral radiograph. |
Statistical Analysis
In our study, SPSS software version 20.0 was used for the statistical analysis of the data. The continuous variables were measured as mean ± standard deviation. The parametric variables with normal distribution were compared between groups using the independent t-test. Proportions were compared using the chi-squared test, p < 0.05 was considered statistically significant. Correlations between the changes in sagittal spinopelvic parameters and clinical outcomes were analyzed using Spearman correlation analysis. The logistic regression model was used to assess the influence of each variable on PLBP.
Results
Based on whether postoperative PLBP was reported in the most recent follow-up, the patients were divided into an experimental group (PLBP) and a control group (non-PLBP). There were 26 subjects in the PLBP group and 174 in the non-PLBP group. There were no statistically significant differences between the two groups in terms of age, gender, BMI, grade, hospital stays, and follow-up (Table 1). All patients completed at least 12 months follow-up: 15.2 ± 2.8 months in the PLBP group, and 14.8 ± 2.2 months in the non-PLBP group. Both groups achieved significant improvements in NRS and ODI after surgery compared with pre-operation; in the PLBP group, p = 0.02 (Table 1).
 |
Table 1 Demographic Data of the Patients |
Of the 200 patients, 26 (13%) suffered from postoperative PLBP. No significant differences in preoperative spinopelvic parameters were found between the two groups (p >0.05). There were statistically significant differences between the variations of preoperative and postoperative spinopelvic parameters LL, SL, LSA, SD, and HOD, regardless of patient group (p < 0.05), but the variation of PI in both groups was not significant. Postoperative PT and SS differed significantly between the PLBP group and non-PLBP group (p < 0.05); however, no significant differences in postoperative LL, SL, LSA, SD, HOD were found between the two groups. In the PLBP group, the variations in PT and SS showed no significant difference between preoperative and postoperative measurements. However, in the non-PLBP group, significant differences were found in the variations in PT and SS (Table 2 and Figure 2). Figure 3 shows preoperative and postoperative positive and lateral views of a 65-year-old female patient who suffered from degenerative spondylolisthesis at L5 and underwent PLIF.
 |
Table 2 Preoperative and Postoperative Spinopelvic Parameters |
There was noticeable correlation between partial sagittal spinopelvic parameters, such as ΔPT and ΔSS, ΔLL, ΔSL, ΔSS and ΔLL, ΔLL and ΔSL. Improvement of NRS and ODI were correlated with ΔPT (Table 3). In logistic regression analysis, age, BMI and most sagittal spinopelvic parameters did not have a significant impact on postoperative PLBP. The ΔPT was found as an independent risk factor for postoperative PLBP (odds ratio=1.45, 95% confidence interval: 1.23–1.68, P<0.001) (Table 4 and Figure 4).
 |
Table 3 Correlation Analysis Between Spinopelvic Parameters and Clinical Outcomes |
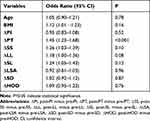 |
Table 4 Logistic Analysis of Each Variable for Postoperative PLBP |
Discussion
Postoperative onset of low back pain or recurrent back pain is common. The short-term and long-term proportion of recurrent low back pain after primary single-level lumbar discectomy ranged from 3% to 34% and 5% to 36%, respectively.6 PLBP may increase the incidence of postoperative complications, as well as decrease the patients’ satisfaction, and thus need to be paid specific attention. PLBP has been reported to be associated with many risk factors, including preoperative long-term backache, fatty infiltration, inadequate decompression, vertebral instability, misjudgment of the response level, and paraspinal muscle degeneration.7 Unfortunately, the exact reason for postoperative low back pain remains unclear. Recently, there has been increased recognition that abnormal preoperative and/or postoperative sagittal spinopelvic parameters, particularly postoperative PLBP, affect outcomes in spinal fusion. Korovessis et al8 suggest that sagittal balance of the lumbar spine is related to chronic low back pain after surgery, although the exact etiology is unclear. Some authors state that postoperative pain after lumbar or lumbosacral fusion is associated with failure of the restoration of spinopelvic parameters such as sacral slope (SS), pelvic tilt (PT), and lumbar lordosis (LL).9,10 Lazennec et al11 demonstrated that patients with persistent postoperative back pain after lumbosacral fusion had a more vertical sacrum, with decreased SS and increased PT: PT in patients with PLBP was almost twice the normal value. He et al12 investigated spinopelvic sagittal balance and clinical outcomes after PLIF in patients with degenerative spondylolisthesis; they conclude that insufficient restoration of PT is an independent factor for PLBP.
PLIF is currently one of the most effective surgical methods for treating lumbar spondylolisthesis. Although surgical techniques have improved, many patients still complain of postoperative PLBP. PLBP may increase the incidence of postoperative complications, as well as decrease the patients’ satisfaction, and thus need to be paid specific attention. Carragee et al14 report an 11% incidence of persistent back or leg pain after limited discectomy, and a 23% incidence of persistent back or leg pain after aggressive discectomy. Schoeggl et al15 demonstrated that 24% of the patients experienced persistent or recurrent pain at a mean follow-up of 7.3 years. We performed a retrospective study including 200 patients, which discovered a 13% incidence of PLBP after PLIF in mild L5-S1 spondylolisthesis. Previous studies have demonstrated that postoperative PLBP is associated with many factors. Papaioannou et al16 proved that preoperative pain catastrophizing was a unique predictor of acute postoperative back pain at an early stage, and of analgesic use following lumbar fusion operation. Hui et al7 report that PLBP following posterior decompression and instrumented fusion was related to preoperative long-term backache, a higher rate of fatty infiltration, and in particular surgery at L5-S1 segment. L5-S1 facet joints are “deep”, and the pedicle screw entering angle is more outward-inclined, requiring a larger range of surgical exposure. Other factors such as inadequate decompression, vertebral instability, misjudgment of the responsible level, and recurrent disc herniation are all risk factors for PLBP.7 Unfortunately, the exact cause of PLBP remains unspecified. Today, with growing knowledge and understanding of the sagittal balance of the spinopelvic unit, there is increased recognition that abnormal preoperative and/or postoperative sagittal spinopelvic parameters affect outcomes in spine surgery, particularly in spinal fusion. Radovanovic et al17 have revealed that restoration of spinopelvic sagittal balance (sagittal vertical axis less than 50 mm) is associated with good clinical outcomes postoperatively in degenerative spondylolisthesis. Kawakami et al9 report that a decrease in SD, an increase in LL, and subsequent restoration of sagittal alignment improved clinical outcomes in the treatment of degenerative spondylolisthesis by posterolateral fusion. Kim et al,18 in their study of degenerative spondylolisthesis patients, note that patients whose PT improved after surgery had greater improvements in their NRS and ODI scores. In view of current reports, we recruited 200 patients from our institutions with mild L5-S1 spondylolisthesis. The patients were divided into two groups according to the presence or absence of postoperative PLBP. There were no statistically significant differences between the two groups in terms of age, gender, BMI, grade, hospital stays, and follow-up. The confounding factors influencing postoperative low back pain were excluded in order to observe the effect of sagittal spinopelvic parameters on postoperative low back pain in mild L5-S1 spondylolisthesis.
Sagittal spinopelvic parameters have been investigated in many studies in recent years. The preoperative and postoperative sagittal spinopelvic parameters in lumbar spondylolisthesis are mainly concentrated on pelvic incidence (PI), pelvic tilt (PT), lumbar lordosis (LL), sacral slope (SS), segmental lordosis (SL), lumbosacral angle (LSA), slip degree (SD), and height of intervertebral disk (HOD). Despite segmental involvement, this pathology affects the whole biomechanical balance of the spine. PI, which is a descriptor of pelvic shape, is the only variable that remained unchanged in our study; it can be calculated by the sum of PT and SS.19 PI tends to increase during childhood and adolescence, before stabilizing in adulthood.20–27 Park et al4 describe the basic deformities of isthmic spondylolisthesis as forward slippage of the vertebral body (SD), kyphotic slip angle (SA), and loss of HOD. They found that, among deformity parameters, only HOD was significantly correlated with improvement of pelvic parameters and sagittal balance. In short, the maintenance of a balanced spinopelvic alignment needs a stable relationship between PI, SS, and LL. Increased PT is a sign of sagittal imbalance.
It is currently well accepted that spinopelvic alignment is important to postoperative outcome for adult spondylolisthesis surgery, particularly with regard to persistent PLBP. Lafage et al28 demonstrated that increased PT results in increased pain and the reduction of function. Chaléat-Valayer et al29 state that in a large proportion of patients, chronic low back pain is related to low SS, low LL, and small PI. Kawakami et al9 report that increased LL was beneficial to the realignment of the spine. Park et al4 found a correlation between changes in HOD and LL; they assume that restoration of the HOD is the most important surgical step and expect that increased LL and subsequent restoration of sagittal balance can improve clinical outcomes. Feng et al30 found that PT and L5I preoperative evaluation may play an important role in the reconstruction of the sagittal alignment and therapeutic outcome. They also found that HOD and SD are correlated with LL in the treatment of isthmic L5-S1 spondylolisthesis. Lazennec et al11 demonstrated that patients with persistent postoperative back pain after lumbosacral fusion had a more vertical sacrum, with decreased SS and increased PT: PT in patients with PLBP was almost twice the normal value. He et al12 found that SL and PT were correlated with NRS and ODI, and that insufficient restoration of PT was an independent factor for PLBP. In our study, 26 of the 200 patients (13%) suffered from postoperative PLBP. No significant differences in preoperative spinopelvic parameters were found between the two groups (PLBP and non-PLBP) (p > 0.05). There were statistically significant differences between variations in preoperative and postoperative spinopelvic parameters SS, LL, SL, LSA, SD, and HOD, regardless of group (p < 0.05), but the variations in PI and PT in the PLBP group had no significant differences.
After rectifying the slip, an appropriately sized cage was inserted between L5 and S1, which would clearly improve HOD, SD, and LSA. As described above (eg, in relation to Melikian et al and Feng et al), HOD, SD, and LSA are correlated with SL and LL. Consequently, SL and LL will also change. These changes at the lumbosacral area produce a secondary adaptation of pelvic orientation in the standing position, presumably to maintain a stable posture. As described above (see Oh et al), SS and PT are directly related to pelvic position. Therefore, rectifying the L5-S1 spondylolisthesis must include restoring PT and SS. Insufficient restoration of PT and SS is a crucial factor for PLBP. Previous authors have discussed the importance of obtaining a PT of less than 20 degrees. This result is confirmed by He et al,12 who found that insufficient restoration of PT was an independent factor for PLBP; and by Lazennec et al,11 who demonstrated that PT in patients with PLBP was almost twice the normal value. In our study, we found that patients with mild L5-S1 spondylolisthesis with PLBP after PLIF had decreased SS and increased PT. This conclusion is similar to that of Lazennec et al. Compared with non-PLBP patients, PLBP patients had significantly worse improvement of PT and SS. We also conducted the correlation analysis between sagittal spinopelvic parameters and clinical outcomes. We found that compared with the non-PLBP group, the PLBP group had worse clinical outcomes and less improvement of PT, indicating the sagittal spinopelvic parameter may be a risk factor for postoperative PLBP. There was noticeable correlation between partial sagittal spinopelvic parameters, such as ΔPT and ΔSS, ΔLL, ΔSL, ΔSS and ΔLL, ΔLL and ΔSL, indicating the change of single sagittal spinopelvic parameter can be affected by the others, which also revealed the impact of on postoperative PLBP was not alteration of one parameter but two or more parameters. Similarly, in logistic regression analysis, the ΔPT was found as an independent risk factor for postoperative PLBP. For this reason, we consider that restoration of PT is crucial in avoiding persistent postoperative back pain. However, our follow-up is very short, and sample size is not large enough, which are limitations of this study. We will avoid these shortcomings in future studies.
Conclusions
The retrospective nature of this study and the possible biases associated with this design bring some limitations to our study. Although confounding factors that may influence clinical outcomes were excluded (eg, there were no significant differences in age, gender, BMI, grade, and operative level of patients in the treatment and control groups), other factors besides the sagittal spinopelvic parameters may affect surgical outcomes. Even if restoration of PT appears a logical goal of treatment, there is no clear evidence that improving spinopelvic alignment has any impact on outcomes for patients. Despite these limitations, this study provides some new information about the surgical treatment of mild L5-S1 spondylolisthesis. On the basis of this study, further large sample collection and long-term postoperative follow-up are necessary.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of Tianjin Union Medical Center. Written informed consent was obtained from all participants. This study was conducted in accordance with the declaration of Helsinki.
Funding
This work was supported by grants from the Foundation of Tianjin Health Bureau (ZC20108).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Faldini C, Di Martino A, Perna F, et al. Changes in spino-pelvic alignment after surgical treatment of high-grade isthmic spondylolisthesis by a posterior approach: a report of 41 cases. Eur Spine J. 2014;23 Suppl 6(6 Supplement):714. doi:10.1007/s00586-014-3552-z
2. Funao H, Tsuji T, Hosogane N, et al. Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis. Eur Spine J. 2012;21(11):2181–2187. doi:10.1007/s00586-012-2374-0
3. Yoshihara H, Yoneoka D. National trends in the surgical treatment for lumbar degenerative disc disease: United States, 2000 to 2009. Spine J. 2015;15(2):265–271. doi:10.1016/j.spinee.2014.09.026
4. Park SJ, Lee CS, Chung SS, et al. Postoperative changes in pelvic parameters and sagittal balance in adult isthmic spondylolisthesis. Neurosurgery. 2011;68(2 Suppl Operative):
5. Mehta VA, Amin A, Omeis I, Gokaslan ZL, Gottfried ON. Implications of spinopelvic alignment for the spine surgeon (vol 70, pg 707, 2011). Neurosurgery. 2012;70(5):1324. doi:10.1227/NEU.0b013e31823262ea
6. Schaller B. Failed back surgery syndrome: the role of symptomatic segmental single-level instability after lumbar microdiscectomy. Eur Spine J. 2004;13(3):193–198. doi:10.1007/s00586-003-0632-x
7. Hui W, Tao W, Qian W, et al. Incidence and risk factors of persistent low back pain following posterior decompression and instrumented fusion for lumbar disk herniation. J Pain Res. 2017;10:1019–1025. doi:10.2147/JPR.S132862
8. Korovessis P, Repantis T, Papazisis Z, et al. Effect of sagittal spinal balance, levels of posterior instrumentation, and length of follow-up on low back pain in patients undergoing posterior decompression and instrumented fusion for degenerative lumbar spine disease: a multifactorial analysis. Spine. 2010;35(8):898–905. doi:10.1097/BRS.0b013e3181d51e84
9. Kawakami M, Tamaki T, Ando M, et al. Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine. 2002;27(1):59. doi:10.1097/00007632-200201010-00014
10. Korsgaard M, Christensen FB, Thomsen K, et al. The influence of lumbar lordosis on spinal fusion and functional outcome after posterolateral spinal fusion with and without pedicle screw instrumentation. J Spinal Disord Tech. 2002;15(3):187–192. doi:10.1097/00024720-200206000-00003
11. Lazennec JY, Ramaré S, Arafati N, et al. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9(1):47–55. doi:10.1007/s005860050008
12. He S, Zhang Y, Ji W, et al. Analysis of spinopelvic sagittal balance and Persistent Low Back Pain (PLBP) for Degenerative Spondylolisthesis (DS) following Posterior Lumbar Interbody Fusion (PLIF). Pain Res Manag. 2020;2020:1–7.
13. Lee JH, Lee SH. Clinical efficacy and its prognostic factor of percutaneous endoscopic lumbar annuloplasty and nucleoplasty for the treatment of patients with discogenic low back pain. World Neurosurg. 2017;105:832. doi:10.1016/j.wneu.2017.06.112
14. Carragee EJ, Spinnickie AO, Alamin TF, et al. A prospective controlled study of limited versus subtotal posterior discectomy: short-term outcomes in patients with herniated lumbar intervertebral discs and large posterior anular defect. Spine. 2006;3(6):88–89. doi:10.1016/S1529-9430(03)00226-2
15. Schoeggl A, Maier H, Saringer W, et al. Outcome after chronic sciatica as the only reason for lumbar microdiscectomy. Clin Spine Surg. 2002;15:415–419.
16. Papaioannou M, Skapinakis P, Damigos D, et al. The role of catastrophizing in the prediction of postoperative pain. Pain Med. 2009;10(8):1452–1459. doi:10.1111/j.1526-4637.2009.00730.x
17. Radovanovic I, J C U, Ganapathy V, et al. Influence of postoperative sagittal balance and spinopelvic parameters on the outcome of patients surgically treated for degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2017;26(4):448–453. doi:10.3171/2016.9.SPINE1680
18. Kim MK, Lee SH, Kim ES, et al. The impact of sagittal balance on clinical results after posterior interbody fusion for patients with degenerative spondylolisthesis: a Pilot study. BMC Musculoskelet Disord. 2011;12(1):69. doi:10.1186/1471-2474-12-69
19. Legaye J, Duval-Beaupère G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99–103. doi:10.1007/s005860050038
20. Mac-Thiong JM, Berthonnaud É, Dimar JRI, et al. Sagittal alignment of the spine and pelvis during growth. Spine. 2004;29(15):1642–1647. doi:10.1097/01.BRS.0000132312.78469.7B
21. Duval-Beaupère G, Schmidt C, Cosson P. A barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20(4):451–462. doi:10.1007/BF02368136
22. Oh SK, Chung SS, Lee CS. Correlation of pelvic parameters with isthmic spondylolisthesis. Asian Spine J. 2010;3:21.
23. Berthonnaud E, Dimnet J, Roussouly P, et al. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18(1):40–47. doi:10.1097/01.bsd.0000117542.88865.77
24. Gelb DE, Lenke LG, Bridwell KH, et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20(12):1351–1358. doi:10.1097/00007632-199520120-00005
25. Ferrero E, Ould-Slimane M, Gille O, et al. Sagittal spinopelvic alignment in 654 degenerative spondylolisthesis. Eur Spine J. 2015;24(6):1219–1227. doi:10.1007/s00586-015-3778-4
26. Vialle R, Ilharreborde B, Dauzac C, et al. Is there a sagittal imbalance of the spine in isthmic spondylolisthesis? A correlation study. Eur Spine J. 2007;16(10):1641–1649. doi:10.1007/s00586-007-0348-4
27. Melikian R, Yoon ST, Kim JY, et al. Sagittal plane correction using the lateral transpsoas approach. SPINE. 2016;41:E1016–E1021.
28. Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine. 2009;34(17):E599. doi:10.1097/BRS.0b013e3181aad219
29. Chaléat-Valayer E, Mac-Thiong J-M, Paquet J, Berthonnaud E, Siani F, Roussouly P. Sagittal spino-pelvic alignment in chronic low back pain. Eur Spine J. 2011;20(5 Supplement):634. doi:10.1007/s00586-011-1931-2
30. Feng Y, Chen L, Gu Y, et al. Influence of the posterior lumbar interbody fusion on the sagittal spino-pelvic parameters in isthmic L5-S1 spondylolisthesis. Clin Spine Surg. 2014;27:E20–E25.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



