Back to Journals » Journal of Blood Medicine » Volume 10
The association between ABO blood group distribution and peptic ulcer disease: a cross-sectional study from Ethiopia
Authors Teshome Y , Mekonen W , Birhanu Y , Sisay T
Received 26 March 2019
Accepted for publication 31 May 2019
Published 4 July 2019 Volume 2019:10 Pages 193—197
DOI https://doi.org/10.2147/JBM.S209416
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Martin Bluth
Yonas Teshome,1 Wondyefraw Mekonen,2 Yohannes Birhanu,3 Tariku Sisay4
1Department of Biomedical Sciences, College of Medicine, Debre Birhan University, Debre Birhan, Ethiopia; 2Department of Physiology, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 3Department of Internal Medicine Gastroenterology Unit, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 4Department of Biomedical Sciences, School of Medicine, College of Health Sciences, Mizan Tepi University, Mīzan Teferī, Ethiopia
Background: Studies have shown that ABO blood group antigens are associated with peptic ulcer disease (PUD). There are limited sources regarding the association of blood groups with PUD patients in Ethiopia. The aim of this study was to assess the association between ABO blood group distribution, non-steroidal anti-inflammatory drugs (NSAIDs), smoking, alcohol, coffee, and PUD at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia.
Methods: A cross-sectional study was undertaken, and a total of 63 endoscopically confirmed PUD patients and 63 healthy controls were screened for ABO blood grouping using the standard slide agglutination reaction. Stool antigens were checked to determine Helicobacter pylori status of PUD patients. Chi-square and logistic regression were used for statistical analysis.
Results: The ABO blood group distribution of PUD patients was 19.04% (12/63), 19.04% (12/63), 11.11% (7/63), 50.79% (32/63) for blood group A, B, AB, and O, respectively, while among control groups it was 25.39% (16/63), 23.80% (15/63), 12.69% (8/63), and 38.09% (24/63) for blood group A, B, AB, and O, respectively. 34.1% (22/63) of PUD patients had gastric ulcer and 65.9% (41/63) had duodenal ulcer. There was statistically a significant association between sex (p=0.001), use of NSAIDs (p=0.001), smoking cigarette (p=0.014), alcohol consumption (p=0.028), and PUD.
Conclusion: Although PUD trended as more prevalent among patients with blood group O than other blood group types their association was not statistically significant.
Keywords: ABO blood group, peptic ulcer disease, gastric ulcer, duodenal ulcer, NSAIDs
Introduction
ABO blood group was first discovered in 1901 by Karl Landsteiner1. It is the most widely used blood grouping system and encoded by a gene located on the long arm of chromosome nine.2 This gene control formation of A and B antigens which are carbohydrate molecules synthesized by the sequential action of the ABO glycosyltransferases.3
The antigens are also present in the secretory fluids such as saliva, sweat, and semen.4 FUT2, the secretor gene, acts independently of the ABO gene on chromosome nine and is active in 80% of the humans called the secretor individual.1 The secretion of these antigens on different tissue plays a role in the susceptibility or resistance to various infectious as well as non-infectious diseases.5–7 According to different literatures, blood group O has protective nature from venous thromboembolism,8,9 pancreatic cancer,10,11 severe malaria,12 while it was found to be prone for cholera and peptic ulcer disease (PUD).13
PUD is a sore in the lining of gastric or duodenal mucosa14 that affects around 5–10% of the general population worldwide.15 The imbalance between defensive factors such as the mucus-bicarbonate barrier, prostaglandins, mucosal blood flow, cell renewal and, aggressive factors such as hydrochloric acid, pepsin, and leukotrienes leads to the formation of peptic ulcer.16
There are many other factors that are responsible for the imbalance between aggressive and defensive factors. H. pylori infection, non-steroidal anti-inflammatory drug (NSAID), smoking, and alcohol consumption are the major ones.17 Psychosocial factors also may have an effect on the development of ulcer by increasing the duodenal acid load, altering local circulation or motility, intensifying Helicobacter pylori infection, stimulating corticosteroid secretion, and affecting health risk behaviors.18
Methods
Hospital-based cross-sectional study was conducted at the gastroenterology unit of Tikur Anbessa Specialized Hospital (TASH) on a total of 126 study participants. The ABO blood group distribution was investigated on endoscopically confirmed 63 PUD patients and 63 healthy control subjects. Stool antigen was checked to determine H. pylori status of PUD patients. The control group included healthy students and the staffs of the hospital that had no individual or family history of PUD.
The study was conducted in accordance with the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Ethics Committee of College of Health Sciences, Tikur-Anbesa, Medical School, Addis Ababa University. Written informed consent was obtained from all subjects before participation. For study participants under the age of 18 years, parents gave informed consent. The ABO blood grouping and stool examination were performed in the main laboratory of TASH, by laboratory technologist using the standard slide agglutination reaction and stool antigen test.
Statistical analysis
Data entry was entered into Epi Data statistical software version 3.1 then exported to SPSS software version 23 for analysis. Chi-square and logistic regression were used to compute the association between parameters. P-value of <0.05 at 95% confidence level was considered to be statistically significant in all the analyses.
Results
The study participants’ age varied between 14 and 81 years with a mean age of 39.10 years. The ABO blood group distribution among PUD patients was found to be 19.04% (12/63) for blood group A and B, 11.11% (7/63) for blood group AB and 50.79% (32/63) for blood group O while among control groups it was 25.39% (16/63) for blood group A, 23.80% (15/63) for blood group B, 12.69% (8/63) for blood group AB and 38.09% (24/63) for blood group O. Blood group O has higher distribution among PUD patients than control groups (50.79% vs 38.09%). (Figure 1).
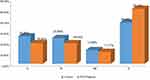 |
Figure 1 Distribution of ABO blood group among peptic ulcer disease patients and control groups in TASH, Addis Ababa, Ethiopia, 2018. |
The endoscopic findings in PUD patients were 34.1% (22/63) for Gastric Ulcer and 65.9% (41/63) for Duodenal Ulcer. Out of 63 PUD patients, 65% (41) was H. pylori positive, and the prevalence of H. pylori infection among the blood group was 56% (23/41) for blood group O, 14.6% (6/41) for blood group A, 19.5% (8/41) for blood group B and 9.7% (4/41) for blood group AB. Furthermore, out of 32 blood group O PUD patients, 72% were H. Pylori infected. Therefore, compared to other blood types, blood group O had a higher percent of H. pylori infection.
Factors associated with PUD
Multivariate analysis was done for those factors that were significantly associated with binary logistic regression. The analysis showed that there was a statistically significant association between sex, use of NSAID, smoking cigarette, and PUD. Accordingly, being a male was four times risky {p=0.001, AOR (95% CI) 4.21(3.30, 7.50)} for acquiring PUD than femaleness.
In the same way, those who smoke cigarette were approximately seven times more likely to have PUD than non-smokers {p=0.014, AOR (95%) 7.32 (1.48, 36.03)}. Even though blood group O was found to have higher distribution among PUD patients than in the control group, there was no statistically significant association between blood group and PUD (Table 1).
 |
Table 1 Multivariate analysis of factors associated with peptic ulcer disease among TASH patients, Addis Ababa, Ethiopia, 2018 |
Discussion
The findings of this study revealed a higher prevalence of PUD among patient with O blood group than other group types. This is consistent with research done in Iraq and Iran.19,20 It can be explained that this is because of the carbohydrate antigens that contributed to the susceptibility or resistance to infectious diseases.21 Especially, the H antigen of blood group O expressed in the gastric mucous membrane is suitable to the attachment of Helicobacter pylori bacillus which is identified to be the major cause of PUD.16,22
Despite the fact that PUD had a higher prevalence among blood group O patients, there was no significant association between ABO blood group distribution and PUD in the current study. This result is inconsistent with cohort research done in Stockholm, Sweden.23 The inconsistency might be due to the difference in sample size (63 vs 1,073,584) and study design (cross-sectional vs cohort). Additionally, phenotyping only the ABO blood groups in red blood cells not in other tissues or exocrine secretions (gastric mucosae, saliva, etc … ), can give chance for the 20% Secretor negative person to be included in the study and reduce the significance of association of blood group with PUD.
Smoking cigarette increases the risk of having PUD seven times according to this research, and the finding was consistent with a study done in Iran17 and Sweden.24 This might be because cigarette smoking increase basal gastric acid secretion through the stimulation of H2-receptor by histamine release25 and decrease the secretion of EGF from the salivary gland, which is necessary for gastric mucosal cell renewal.3
In the same way, alcohol consumption was found to increase the risk of acquiring PUD about three folds which is similar to the study conducted in Nairobi, Kenya that shows an association between alcohol consumption and PUD.26 This might be because alcohol consumption increases gastric acid secretion by maleic and succinic acids27 as well as cause mucosal damage and disruption which increases mucosal acid permeability.28,29
NSAIDs were significantly associated with PUD in this study. These drugs are known to initiate mucosal injury topically by their acidic properties and diminish the hydrophobicity of gastric mucus.30
NSAIDs also cause the decreased synthesis of mucosal prostaglandin which increases mucosal blood flow. Adequate blood flow in mucosal circulation will not be maintained when there is reduced prostaglandin production because of the inhibitory effect of NSAIDs.27
Conclusion
Although PUD trended as more prevalent among patients with blood group O than other blood group types their association was not statistically significant. PUD has a statistically significant association with the use of NSAIDs, alcohol consumption, smoking cigarette, and male sex.
Acknowledgments
We would like to thank all our participants who enthusiastically helped us. We would also like to thank the College of Health Sciences, Addis Ababa University for the financial support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hult A. Studies of the ABO and FORS Histo-Blood Group Systems: focus on flow cytometric and genetic analysis. Lund Univ. 2013;91:1652–1875.
2. Daniel G. Human Blood Groups.
3. Zhang L, Ren JW, Wong CCM, et al. Effects of cigarette smoke and its active components on ulcer formation and healing in the gastrointestinal mucosa. Curr Med Chem. 2012;19:63–69.
4. Thrumiaya T, Gayathri R, Priya VV. Efficacy and accuracy of ABO blood group determination from saliva. J Adv Pharm Edu Res. 2017;7(2):101–103.
5. Su M, Lu S, Tian D, et al. Relationship between ABO blood groups and carcinoma of esophagus and cardia in Chaoshan inhabitants of China. World J Gastroenterol. 2001;7(5):657–661. doi:10.3748/wjg.v7.i5.657
6. Xun Y, Huang Y, Feng JF. Is there an association between ABO blood group and overall survival in patients with esophageal squamous cell carcinoma. Int J Clin Exp Med. 2014;7(8):2214–2218.
7. Wang Z, Liu L, Ji J, et al. ABO blood group system and gastric cancer: a case-control study and meta-analysis. Int J Mol Sci. 2012;13:13308–13321. doi:10.3390/ijms131013308
8. Franchini M, Lippi G. Relative Risks of Thrombosis and Bleeding in Different ABO Blood Groups. New York: Thieme Medical Publishers; 2015:0094–100.
9. Zhong M, Zhang H, Reilly P, et al. ABO blood group as a model for platelet glycan modification in arterial thrombosis. Am Heart J. 2015;35:1570–1578.
10. Laufey A, Peter K, Rachael Z. Genome-wide association study identifies variants in the ABO locus associated with susceptibility to pancreatic cancer. National Ins Health. 2009;41(9):986–990.
11. Zhang B-L, Na H, Huang Y-B, et al. ABO blood groups and risk of cancer: a systematic review and meta-analysis. Asian Pac J Cancer Prev. 2014;15(11):4643–4650.
12. Panda A, Panda K, Sahu A, Tripathy R, Ravindran B, Das BK. Association of ABO blood group with severe falciparum malaria in adults: case control study and meta-analysis. Malar J. 2011;10:309–317. doi:10.1186/1475-2875-10-309
13. Anstee D. The relationship between blood groups and disease. Blood J. 2017;115(23):4635–4643. doi:10.1182/blood-2010-01-261859
14. Schwartz’s, Charles B, Dana K, et al. Principles of Surgery.
15. Lauret M, Pérez I, Rodrigo L. Peptic ulcer disease. Austin J Gastroenterol. 2015;2(5):1055–1063.
16. Amadeep K, Robin S, Ramica S, Sunil K. Peptic ulcer: a review on etiology and pathogenesis. Int Res J Pharm. 2012;3(6):34–38.
17. Barazandeh F, Yazdanbod A, Pourfarzi F, Sepanlou SG, Derakhshan MH, Malekzadeh R. Epidemiology of peptic ulcer disease: endoscopic results of a systematic investigation in Iran. Middle East J Dig Dis. 2012;4:90–96.
18. Levenstein S. Psychosocial factors in peptic ulcer and inflammatory bowel disease. J Consult Clin Psychol. 2002;70(3):739–750. doi:10.1037/0022-006X.70.3.739
19. Abdulridha MK. The relationship between ABO blood group distribution and the incidence of upper gastric and duodenal ulcer in Iraqi patients. Iraqi J Pharm Sci. 2013;22:1.
20. Rasmi Y, Sadreddini M, Peirovi T, et al. Frequency of ABO blood group in peptic ulcer disease in Iranian subjects. Pak J Biol Sci. 2009;12:13.
21. Mattos L, Moreira H. Genetic of the ABO blood system and its link with the immune system. Rev Bras Hematol Hhemoter. 2004;26(1):60–63. doi:10.1590/S1516-84842004000100012
22. Baqir G, Al-Sulami A, Hamadi S. Relationship between ABO blood groups and helicobacter pylori infection among patients with dyspepsia. J Virol Microbiol. 2016;(2016):30–31.
23. Edgren G, Henrik H, Klaus R, et al. Risk of gastric cancer and peptic ulcers in relation to ABO blood type: a cohort study. Am J Epidemiol. 2010;172:1280–1285. doi:10.1093/aje/kwq299
24. Aro P, Storskrubb T, Ronkainen J, et al. Peptic ulcer disease in a general adult population the kalixanda study: a random population-based study. Am J Epidemiol. 2006;163:129–139. doi:10.1093/aje/kwj129
25. Maity P, Biswas K, Roy S, et al. Smoking and the pathogenesis of gastroduodenal ulcer: recent mechanistic update. Mol Cell Biochem. 2003;253:329–338.
26. Edy Stermer. Alcohol consumption and the gastrointestinal tract. IMAJ. 2002;4:200–202.
27. Zatorski H. Pathophysiology and risk factors in peptic ulcer disease. In: Fichna, editor, Introduction to Gastrointestinal. Vol. 2. 2017.
28. Zhang L, Eslick GD, Xia HH-X, et al. Relationship between alcohol consumption and active helicobacter pylori infection. Alcohol Alcohol. 2010;45(1):89–94. doi:10.1093/alcalc/agp068
29. Mustafa M, Menon J, Muiandy RK. Risk factors,diagnosis, and management of peptic ulcer disease. IOSR J Dent Med Sci. 2015;14:40–46.
30. Katunge ML. Factors Associated with Peptic Ulcers among Adult Patient Attending St. Michael Digestive Diseases and Medical Care in Upper Hill. Nairobi County: University of NAIROBI; 2009.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
