Back to Journals » Open Access Emergency Medicine » Volume 14
The Anesthetic Techniques for Earthquake Victims in Indonesia
Authors Waloejo CS, Sulistiawan SS, Semedi BP, Dzakiyah AZ, Stella MA, Ikhromi N, Nahyani, Endriani E, Rahardjo E, Pandin MGR
Received 3 August 2021
Accepted for publication 10 February 2022
Published 25 February 2022 Volume 2022:14 Pages 77—84
DOI https://doi.org/10.2147/OAEM.S331344
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Christrijogo Soemartono Waloejo,1,2 Soni Sunarso Sulistiawan,2 Bambang Pujo Semedi,2 Afifah Zahra Dzakiyah,3 Maria Arni Stella,3 Noryanto Ikhromi,3 Nahyani,4 Elya Endriani,4 Eddy Rahardjo,1,2 Moses Glorino Rumambo Pandin1
1Master Program in Disaster Management, Postgraduate School, Universitas Airlangga, Surabaya, Indonesia; 2Anesthesiology and Reanimation Department, Dr. Soetomo Public Academic Hospital, Surabaya, Indonesia; 3Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia; 4Anesthesiologist in Public Hospital of Nusa Tenggara Barat, Mataram, Indonesia
Correspondence: Moses Glorino Rumambo Pandin, Disaster Management Program, Postgraduate School, Universitas Airlangga, Jl. Airlangga 4-6, Surabaya, East Java, 60286, Indonesia, Tel +62 89621780233, Email [email protected]
Introduction: In Lombok, three-large magnitude earthquakes occurred in July 2018 and caused major losses: 564 victims died, 1684 were injured, 445,343 people became refugees, and 215,628 houses were damaged. It damaged 408 health facilities, consisting of 89 public health centers, 13 hospitals, 174 auxiliary public health centers, 132 village health posts.
Aim: The purpose of this study is to describe the anesthetic techniques that were used to treat earthquake victims.
Methods: This study was a descriptive cross-sectional study that was conducted by collecting total sampling from all earthquake victims treated in the emergency room (ER) of the regional public hospital (RSUD NTB) on August 6th and 7th, 2018, and all victims who underwent surgery during August 5th– 25th, 2018. The data that were collected were surgery type, anesthetic techniques, and anesthesia drugs that were used.
Results: The results show that the highest number of patients were treated in the ER during the first seven days after the earthquake and that this number then decreased over several weeks. The majority of patients treated were trauma patients who needed orthopedic surgery. General anesthesia was more widely used than regional anesthesia, but the difference was not significant. The most commonly used regional anesthetic was lidocaine hyperbaric 75– 100 mg and clonidine 30– 50 mcg combination. Regional anesthesia techniques have better results in cases of lower limb injury, but it is difficult to be applied in earthquake victims who present with complex injuries and limited resources.
Keywords: anesthesia, technique, earthquake, victim management, health
Introduction
Earthquakes are the second most frequent natural Disaster after floods and caused the most significant economic losses in the world during 2007–2016.1 Indonesia is at the confluence of three active world plates: the India-Australia, Eurasia, and Pacific plates, making it vulnerable to earthquakes.2 Losses caused by earthquakes depend on the magnitude, the distance from the epicenter, the population density, earthquake preparedness, and mitigation efforts.3
From January to April 2017, there were 1426 earthquake events in Indonesia with a magnitude of 1–9.5 on the Richter scale.4 Usually, a large-magnitude earthquake only occurs once, followed by small-magnitude earthquakes. However, in Lombok in July 2018, a large-magnitude earthquake occurred three times: once on Jul 29th, 2018, Aug 5th, 2018, and Aug 19th, 2018 (Figure 1). In addition, there were 2087 small-magnitude earthquakes, 64 of which could be felt to occur afterward.5 The repeated large-magnitude earthquakes in Lombok caused major losses: 564 victims died, 1684 were injured, 445,343 became refugees, and 215,628 houses were damaged.61 In addition, the damaged were 408 health facilities, consisting of 89 Public Health Centers, 13 Hospitals, 174 auxiliary Public Health Centers, 132 Village Health Posts. The situation is made worse by the fact that health workers are also became victims (Figure 1).
 |
Figure 1 Map of districts/cities affected by the earthquake in Lombok, Indonesia. |
West Nusa Tenggara (NTB) Province is an archipelagic province consisting of 2 (two) large islands, namely Lombok and Sumbawa, with at least 332 small islands consisting of 7 regencies/cities. Its total population is 3,798,297, with a population density of 246 inhabitants/km2. However, only Mataram City has the number of health facilities that meet the minimum standard of availability of health facilities, while other regencies/cities still require additional health facilities (Figure 2). Furthermore, although all regencies/cities affected by the earthquake have not met the minimum standard for the availability of general practitioners and specialist doctors, only Mataram City has met the minimum standard availability of specialists.
 |
Figure 2 Number of health service facilities of districts/cities affected by the earthquake. |
In RSUD NTB, there were 11 operating Surgery rooms in the hospital building available. However, after the second earthquake hit, Surgery activities were moved to surgery rooms built from container boxes outside the hospital building with five rooms for safety precautions. In addition, two2 anesthesiologists were on duty for 2 weeks shift rotation in the hospital.
The main cause of death and injuries is building collapse.6 Most of these buildings are not designed to withstand earthquakes or were poorly constructed.7,8 The mode of injury when a building buries victims, the severity of the injury, and the length of time needed to evacuate victims affect the mortality and morbidity rates.9–12 The roles of physicians, general practitioners, specialist doctors, and nurses are also vital in the first hour after the earthquake to prevent the conditions of victims from worsening (Table 1). In such situations, anesthesiologists and surgeons are the most needed specialists to provide prompt therapy for injured victims.13 Anesthesia is also an essential component to manage victims’ pain before, during, and after surgery.14
 |
Table 1 The Number of Casualties by the Earthquake in Lombok, Indonesia |
Anesthesia techniques that can be applied in earthquake victims include general and regional anesthesia. During the management of the 2015 Nepal earthquake, regional anesthesia techniques were widely used because of several advantages, such as safety in the context of unknown patient history, a shorter period of anesthesia recovery and ICU use, minimized use of oxygen and other postoperative treatments, and the ability to reduce postoperative pain.15
This research was conducted to describe the conditions of Lombok earthquake victims managed by the RSUD NTB, especially to describe the anesthetic techniques used to treat the earthquake victims.
Methods
The current study was a descriptive cross-sectional study. The data were collected from the anesthesia record of all earthquake victims treated at the emergency room (ER) of the RSUD NTB on August 6th and 7th, 2018. In addition, the samples took from all victims who underwent Surgery from August 5th – 25th, 2018. Therefore, the study used total sampling, and the anesthesiologists on duty validated the data during the surgery.
The procedures: first, the patients were brought by the evacuation and triage team from the disaster site to the ER. Patients were examined in the ER to decide which patient would undergo surgery; second, anesthesiologists examined the patient prioritizing ASA 1 or 2 of ASA physical status.16 Finally, the anesthesiologists decide to exclude patients if they are deemed not visible to have surgery.
The data of drugs were collected from the type of anesthesia techniques and anesthesia drugs that were used. The criteria applied also distinguished based on trauma and non-trauma cases and the type of surgery performed. Since all data were secondary data from anesthesia earthquake victims, then, the informed consent were waived. The recorded data analyzed and presented in descriptive form using frequencies, pie charts, bar diagrams, and tables. Ethical clearance was approved from RSUD NTB (number: 070.1/25.a.KEP/2018).
Results
There were 166 victims treated in the ER of the RSUD NTB on August 6th and 7th, 2018. A total of 133 victims were trauma patients, and 33 others were non-trauma patients. There were also 153 surgeries performed during August 5th – 25th, 2018, as some patients required more than one surgery. No patients were excluded from surgery. Day 1, represents Jul 29th, 2018, when the first large-magnitude earthquake occurred. Day 7, represents Aug 5th, 2018, when the disaster management team started to evacuate victims, shown in Figure 3.
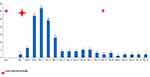 |
Figure 3 The number of cases per day during the earthquake. |
During this period, 79 females (51.6%) and 74 males (48.4%) patients underwent surgery. The youngest patient is 1(one) day old, the oldest patient is 95 years old, and the patients were generally 30 years old. Elderly patients were predominantly women, while children and young adult patients were predominantly men.
Comparison of the selection of general or regional anesthesia shows little difference. Eighty-four of 153 patients received general anesthesia (54.9%), and 69 others received regional anesthesia (45.1%). Similarly, a comparison of the anesthesia techniques used in male and female patients showed no significant difference. In men, 43 (28.1%) patients received general anesthesia, and 30 (19.6%) patients received regional anesthesia. In women, 39 (24.49%) patients received general anesthesia, and 38 (24.84%) patients received regional anesthesia.
The artificial airways used in general anesthesia included intubation, mask, and laryngeal mask airway (LMA). Intubation was the most widely used technique, applied in as many as 62 patients (75%), followed by the use of a mask in 12 patients (14%) and the use of an LMA in 9 patients (11%). The regional techniques used included subarachnoid block (SAB) and peripheral nerve block (PNB), applied in 66 patients (94%) and four patients (6%), respectively.
The regional anesthesia drugs used in this study were lidocaine 2% 20–30 cc, hyperbaric lidocaine 75–100 mg, levobupivacaine 15–20 mg, lidocaine hyperbaric 75–100 mg and Clonidine 30–50 mcg combination, and other drugs, such as Ropivacaine 0.75% 30 mg. The most used drug was hyperbaric lidocaine with Clonidine, at a rate of 49%, followed by lidocaine (20%), hyperbaric lidocaine (14%) levobupivacaine (10%), and other drugs (7%). Commonly, the most surgery type during earthquake management was orthopedic surgery (109 times, 70.8%), followed by neurosurgery (13%), general surgery (10.4%), plastic surgery (4.5%), and obstetric and urological surgery (both 0.6%). An illustration of the selection of anesthesia techniques by surgery type is shown in Figure 4.
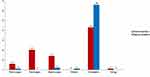 |
Figure 4 The nesthesia options and techniques based on the type of surgery and surgical techniques. |
Regional anesthesia was mainly used during orthopedic surgery. Based on the operative region, regional anesthesia was primarily used in the rural part (53.62%), followed by the femoral region (26.09%) and pedal region (7.25%).
According to the operative procedure, regional anesthesia was used in as much as 100%, 54.69%, and 59.57% of amputation, debridement, and fixation procedures, respectively. On the other hand, general anesthesia was predominantly used in craniotomy (100%) and other procedures (83.33%). In addition, the other procedures included skin grafting, reconstructive surgery, laparotomy, thoracentesis, and vertebral stabilization procedures.
Discussion
The earthquakes on Lombok Island are different from other earthquakes, as three large-magnitude earthquakes occurred in succession. The largest magnitude earthquake occurred on Aug 5th, 2018, and claimed the most casualties compared to the previous and subsequent major earthquakes. In addition, the earthquake occurred when people were typically asleep inside of their houses, such that they could not escape and look for shelter. This condition also explains why the victims predominantly showed orthopedic traumas and injuries.
In natural disasters such as earthquakes, the third to fifth days after the disaster are the busiest days when victims seek medical help.17 In this study, the highest number of victims were treated in the ER on the third to fifth day after the first largest magnitude earthquake occurred, or approximately a week after the first earthquake occurred. Thus, the demand for services at local health facilities is very high during the first week after an earthquake3 (Table 2).
 |
Table 2 The Number of Health Care Facilities Damaged by the Earthquake in Lombok, Indonesia |
Based on the results, the type of operation during earthquake management was dominated by orthopedic surgery, followed by neurosurgery, general surgery, and plastic surgery. These types of surgery are related to the kind of trauma experienced by the earthquake victims due to building collapse. Therefore, selecting the optimal anesthesia technique will minimize the physical and psychological stress on the patient.13 Moreover, providing appropriate pain management using anesthesia will prevent physical and psychological sequelae, especially in high-risk victims, such as children and the elderly.18–21
The selection of anesthesia techniques must be based on the existing conditions and facilities. In addition, the choice of anesthesia techniques should avoid cardiorespiratory depression and muscle relaxation as much as possible as the postoperative ICU is limited.22 In this study, general and regional anesthesia selection comparison showed no significant difference, although general anesthesia was used more. The use of general anesthesia is considered more often in disaster areas with minimal human resources. For example, in developing countries such as Indonesia, as stated by MSF (Medecins Sans Frontieres).23 However, the selection of artificial airways during general anesthesia must also be considered. With more patients undergoing mask artificial airway procedures, more anesthesiologists are needed to stand by for the patient during the operation. On the other hand, the increased usage of intubation and LMA during Surgery with general anesthesia allows anesthesiologists to perform other tasks during the operation.
In another study, the use of general inhalation anesthesia in disaster situations was more limited because of the catastrophic effects that make it impossible to provide facilities for anesthesia machines and inhalation drugs. In addition, most patients who receive general anesthesia have food in their stomach in a disaster condition. Therefore, it is necessary to perform rapid-sequence induction immediately followed by tracheal intubation to prevent gastric acid aspiration.24
In this happening and the previous earthquake, most victims experienced trauma to the lower limbs,25–28 especially fractures of the tibia and fibula. In cases of lower limb trauma, pain management is best performed with regional anesthesia,29–33 especially with a femoral nerve block.34 The same result was found in this study, as regional anesthesia was mostly used in cases of lower limb trauma. The high use of regional anesthesia in cases of simple extremity injuries after a disaster was also found in a previous study in which epidural anesthesia (EA) and SAB techniques were used in cases of lower limb injury, and PNB was used in cases of upper extremity injury.35
However, the higher frequency of general anesthesia than regional anesthesia in this study could have been caused by the application of regional anesthesia requiring special skills that not all doctors possess.36–38 For example, the doctor needs ultrasound facilities and nerve stimulators to perform regional anesthesia, but during the disaster, those apparatus were limited to implementation for regional anesthesia.20,39,40 Moreover, regional anesthesia is only effective in cases of simple hip or femoral fracture.36–38 In cases of more complex trauma, general anesthesia could be the better option.34
Regarding drugs that can be used in regional anesthesia, MSF has determined anesthesia techniques and drugs that can be applied in situations with limited resources and facilities. These drugs include thiopental and ketamine for general anesthesia without intubation, halothane for general anesthesia with intubation, 0.5% bupivacaine hyperbaric for spinal anesthesia, and levobupivacaine for regional anesthesia.14 However, it is different from what was found in this study.41 Drugs mostly used in regional anesthesia were hyperbaric lidocaine combined with clonidine hydrochloride, an alpha-2 agonist drug commonly used in anesthesia. Therefore, lidocaine is a local anesthesia drug commonly used in intravenous regional anesthesia (IVRA) because of its fast-onset and short duration of anesthesia.42 In addition, it made lidocaine reliable to use in source-limited conditions like earthquake disasters. Hyperbaric (heavy) lidocaine can accumulate in lower space based on gravity. Therefore, it prevents the spread of anesthesia block in the higher spinal segment hypotension and other cardiovascular events.
On the contrary, the different results obtained by other previous studies stated that hyperbaric lidocaine gives a more prolonged onset of anesthesia and a shorter duration of anesthesia than isobaric lidocaine,43 even Toft et al said those differences were not significant between the two groups.44 Furthermore, unfortunately, transient neurologic symptom (TNS) occurred more often in hyperbaric lidocaine postoperative than isobaric lidocaine.45 Even though hyperbaric lidocaine is still worth using because of the limitation on drug availability in the conditions after the earthquake. Clonidine is an alpha-2 agonist commonly used as an adjuvant to regional anesthesia. Clonidine has approximately 1/8 potency of dexmedetomidine. Although adding Clonidine to IVRA gives controversial results in the Kleinschmidt study,46 Reuben found that Clonidine made postoperative analgesia has better results.47 Besides, Clonidine as an adjuvant can increase anesthesia duration48 and prolong analgesia49 when used with intermediate and long-acting local anesthetics.
According to the operation type, orthopedic surgery was most commonly needed to treat earthquake victims, including amputation, fixation, debridement, and craniotomy. The same result was also found in other studies, in which fixation, debridement, and amputation of the lower limb were the most common procedures.50–54 Similar to the present study, in previous studies, regional anesthesia was also mostly used during orthopedic surgery.36–38 In addition, open and closed fractures were the most frequent injuries in a previous study, followed by crush injuries and compartment syndrome.54,55 The same finding was also presented by MSF, which stated that more than 90,000 surgical procedures in natural disasters are orthopedic but have difficulties related to the limited availability of resources to provide safe anesthesia for patients.55–57
This study has several limitations. First, this study did not record data that can help measure the effectiveness of the different anesthesia techniques and anesthesia drugs. However, some measurements could be recorded, like non-operative time (NOT = room turnover time plus anesthesia induction and emergence time),58 postoperative pain score,59 and Quality of Recovery Score.60 Another limitation is that this study only recorded events in Lombok’s three-large magnitude earthquakes in July 2018. More extensive data need to be collected from different disaster settings and times to get a broader view and better results that describe the population’s conditions.
Conclusion
The study concluded that the majority used regional anesthesia drugs were hyperbaric lidocaine and Clonidine. The management of earthquake victims on Lombok Island found that the role of anesthesiologists during a disaster is essential in achieving safe and optimal surgical conditions. However, the limited number of anesthesiologists in developing countries should be considered for optimal anesthesia techniques so that disaster preparation and disaster management can proceed well.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. CRED. Natural Disasters. Louvain, Belgium: CRED; 2017.
2. Marfai MA, King L, Singh LP, et al. Natural hazards in Central Java Province, Indonesia: an overview. Environ Geol. 2008;56(2):335–351. doi:10.1007/s00254-007-1169-9
3. Bartels SA, Vanrooyen MJ. Medical complications associated with earthquakes. Lancet. 2012;379(9817):748–757. doi:10.1016/S0140-6736(11)60887-8
4. Hamdani SB. Pengetahuan Manajemen Resiko Bencana Gempa Bumi Pada Kelompok Lansia Di Desa Lampulo Kecamatan Kuta Alam Kota Banda Aceh. [Knowledge of Earthquake Disaster Risk Management on Elderly Groups in Lampulo Village, Kuta Alam Kota Banda Aceh District]. Angew Chemie Int Ed. 2017;6(11):
5. BMKG. #Gempabumi Lombok 2018. 2018.
6. Noji EK. The public health consequences of disasters. Prehosp Disaster Med. 2000;15:21–31. doi:10.1017/S1049023X00025255
7. Glass RI, Urrutia JJ, Sibony S, Smith H, Garcia B, Rizzo L. Earthquake injuries related to housing in a Guatemalan village. Science (80-). 1977;197(4304):638–643. doi:10.1126/science.197.4304.638
8. Noji EK, Kelen GD, Armenian HK, Oganessian A, Jones NP, Sivertson KT. The 1988 earthquake in Soviet Armenia: a case study. Ann Emerg Med. 1990;19(8):891–897. doi:10.1016/S0196-0644(05)81563-X
9. Pointer JE, Michaelis J, Saunders C, et al. The 1989 Loma Prieta earthquake: impact on hospital patient care. Ann Emerg Med. 1992;21(10):1228–1233. doi:10.1016/S0196-0644(05)81751-2
10. Coburn A, Hughes R. Fatalities, injury and rescue in earthquakes. In: 2nd Conference of the Development Studies Association. Manchester, England: University of Manchester; 1987:1–80.
11. Coburn A, Murakami H, Ohta Y. Factors affecting fatalities and injury. In: Earthquakes: Engineering Seismology and Earthquake Disaster Prevention Planning Internal Report. Hokkaido, Japan: Hokkaido University; 1987:1–80.
12. Desforges J, Better OS, Stein JH. Early management of shock and prophylaxis of acute renal failure in traumatic rhabdomyolysis. N Engl J Med. 1990;322:825–829. doi:10.1056/NEJM199003223221207
13. Schultz CH, Koenig KL, Noji EK. A medical disaster response to reduce immediate mortality after an earthquake. N Engl J Med. 1996;334(7):438–444. doi:10.1056/NEJM199602153340706
14. Trelles Centurion M, Van Den Bergh R, Gray H. Anesthesia provision in disasters and armed conflicts. Curr Anesthesiol Rep. 2017;7(1):1–7. doi:10.1007/s40140-017-0190-0
15. Lehavi A, Meroz Y, Maryanovsky M, et al. Role of regional anaesthesia in disaster medicine: field hospital experience after the 2015 Nepal Earthquake. Eur J Anaesthesiol. 2016;33(5):312–313. doi:10.1097/EJA.0000000000000424
16. Committee on Economics American Society of Anesthesiologists. ASA physical status classification system; 2020. Available from: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system.
17. Naghii MR. Public health impact and medical consequences of earthquakes. Rev Panam Salud Publica. 2005;18(3):216–221. doi:10.1590/S1020-49892005000800013
18. Chen G, Lai W, Liu F, et al. The dragon strikes: lessons from the Wenchuan earthquake. Anesth Analg. 2010;110(3):908–915. doi:10.1213/ANE.0b013e3181cbc62c
19. Sinatra R, Pain C. Review article. Pain Medicine (Malden, Mass.). 2010;11:1859–1871. doi:10.1111/j.1526-4637.2010.00983.x
20. Missair A, Gebhard R, Pierre E, et al. Surgery under extreme conditions in the aftermath of the 2010 Haiti earthquake: the importance of regional anesthesia. Prehosp Disaster Med. 2010;25(6):487–493. doi:10.1017/S1049023X00008645
21. Lippert SC, Nagdev A, Stone MB, Herring A, Norris R. Pain control in disaster settings: a role for ultrasound-guided nerve blocks. Ann Emerg Med. 2013;61(6):690–696. doi:10.1016/j.annemergmed.2012.03.028
22. Adesunkanmi A. Where there is no anaesthetist: a study of 282 consecutive patients using intravenous, spinal, and local infiltration anaesthetic techniques. Trop Doct. 1999;27:56–57. doi:10.1177/004947559902900122
23. Ariyo P, Trelles M, Helmand R, et al. Providing anesthesia care in resource-limited settings. Anesthesiology. 2016;124(3):561–569. doi:10.1097/ALN.0000000000000985
24. Jenkins K, Baker AB. Consent and anaesthetic risk. Anaesthesia. 2003;58(10):962–984. doi:10.1046/j.1365-2044.2003.03410.x
25. Jacquet GA, Hansoti B, Vu A, Bayram JD. Earthquake-related injuries in the pediatric population: a systematic review. PLoS Curr. 2013;0–14. doi:10.1371/currents.dis.6d3efba2712560727c0a551f4febac16
26. Mulvey JM, Awan SU, Qadri AA, Maqsood MA. Profile of injuries arising from the 2005 Kashmir Earthquake: the first 72 h. Injury. 2008;39(5):554–560. doi:10.1016/j.injury.2007.07.025
27. Carlson LC, Hirshon JM, Calvello EJB, Pollak AN. Operative care after the Haiti 2010 earthquake: implications for post-disaster definitive care. Am J Emerg Med. 2013;31(2):429–431. doi:10.1016/j.ajem.2012.10.020
28. Kang P, Zhang L, Liang W, et al. Medical evacuation management and clinical characteristics of 3255 inpatients after the 2010 Yushu earthquake in China. J Trauma Acute Care Surg. 2012;72(6):1626–1633. doi:10.1097/TA.0b013e3182479e07
29. Antonis M, Chandwani D, McQuillen K. Ultrasound-guided placement of femoral 3-in-1 anesthetic nerve block for hip fractures. Acad Emerg Med. 1997;13:S122–123. doi:10.1197/j.aem.2006.03.302
30. Marhofer P, Schrögendorfer K, Koinig H, Kapral S, Weinstabl C, Mayer N. Ultrasonographic guidance improves sensory block and onset time of three-in-one blocks. Anesth Analg. 1997;85(4):854–857. doi:10.1213/00000539-199710000-00026
31. Snoeck MM, Vree TB, Gielen MJM, Lagerwert AJ. Steady-state bupivacaine plasma concentrations and safety of a femoral “3-in-1” nerve block with bupivacaine in patients over 80 years of age. Int J Clin Pharmacol Ther. 2003;41(3):107–113. doi:10.5414/CPP41107
32. McGlone R, Sadhra K, Hamer DW, Pritty PE. Femoral nerve block in the initial management of femoral shaft fractures. Arch Emerg Med. 1987;4(3):163–168. doi:10.1136/emj.4.3.163
33. Tan TT, Coleman MM, Fletcher AK, Heyes FLP; Femoral blockade for fractured neck of femur in the emergency department. Three-in-one femoral nerve blockade as analgesia for fractured neck of femur in the emergency department: a randomized, controlled trial. Ann Eme Ann Emerg Med. 2003;42(4):596–597. doi:10.1067/S0196-0644(03)00606-1
34. Levine AC, Teicher C, Aluisio AR, et al. Regional Anesthesia for Painful Injuries after Disasters (RAPID): study protocol for a randomized controlled trial. Trials. 2016;17(1):1–9. doi:10.1186/s13063-016-1671-z
35. Zheng W, Hu Y, Xin H. Successful implementation of thirty-five major orthopaedic procedures under poor conditions after the two thousand and fifteen Nepal earthquake. Int Orthop. 2016;40(12):2469–2477. doi:10.1007/s00264-016-3284-2
36. Foss NB, Kristensen BB, Bundgaard M, et al. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: a randomized, placebo-controlled trial. Anesthesiology. 2007;106(4):773–778. doi:10.1097/01.anes.0000264764.56544.d2
37. Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: a randomized controlled trial. Acad Emerg Med. 2013;20(6):584–591. doi:10.1111/acem.12154
38. Christos SC, Chiampas G, Offman R, Rifenburg R. Ultrasound-guided three-in-one nerve block for femur fractures. West J Emerg Med. 2010;11(4):310–313.
39. Buckenmaier CC, Lee EH, Shields CH, Sampson JB, Chiles JH. Regional anesthesia in austere environments. Reg Anesth Pain Med. 2003;28(4):321–327. doi:10.1097/00115550-200307000-00012
40. Stojadinovic A, Auton A, Peoples GE, et al. Responding to challenges in modern combat casualty care: innovative use of advanced regional anesthesia. Pain Med. 2006;7(4):330–338. doi:10.1111/j.1526-4637.2006.00171.x
41. Liu L, Qian J, Shen B, Xiao F, Shen H. Intrathecal dexmedetomidine can decrease the 95% effective dose of bupivacaine in spinal anesthesia for cesarean section: a prospective, double-blinded, randomized study. Medicine (Baltimore). 2019;98(9):e14666. doi:10.1097/MD.0000000000014666
42. Frisch NB, Darrith B, Hansen DC, Wells A, Sanders S, Berger RA. Single-dose lidocaine spinal anesthesia in hip and knee arthroplasty. Arthroplast Today. 2018;4(2):236–239. doi:10.1016/j.artd.2018.02.011
43. Harbers JBM, Stienstra R, Gielen MJM, Cromheecke GJ. A double blind comparison of lidocaine 2% with or without glucose for spinal anesthesia. Acta Anaesthesiol Scand. 1995;39(7):881–884. doi:10.1111/j.1399-6576.1995.tb04191.x
44. Toft P, Bruun-Mogensen C, Kristensen J, Hole P. A comparison of glucose-free 2% lidocaine and hyperbaric 5% lidocaine for spinal anaesthesia. Acta Anaesthesiol Scand. 1990;34(2):109–113. doi:10.1111/j.1399-6576.1990.tb03053.x
45. Imbelloni LE, Beato L. Lidocaine 2% with or without glucose 8% for spinal anesthesia for short orthopedic surgery. Can J Anesth. 2005;52(8):887–888. doi:10.1007/BF03021791
46. Kleinschmidt S, Stöckl W, Wilhelm W, Larsen R. The addition of Clonidine to prilocaine for intravenous regional anaesthesia. Eur J Anaesthesiol. 1997;14(1):40–46. doi:10.1046/j.1365-2346.1997.00063.x
47. Reuben SS, Steinberg RB, Klatt JL, Klatt ML. Intravenous regional anesthesia using lidocaine and clonidine. Anesthesiology. 1999;91(3):654. doi:10.1097/00000542-199909000-00015
48. Pöpping DM, Elia N, Marret E, et al. Clonidine as an adjuvant to local anesthetics for peripheral nerve and plexus blocks. A meta-analysis of randomized trials. Anesthesiology. 2009;111(2):406–415. doi:10.1097/ALN.0b013e3181aae897
49. McCartney CJL, Duggan E, Apatu E. Should we add clonidine to local anesthetic for peripheral nerve blockade? A qualitative systematic review of the literature. Reg Anesth Pain Med. 2007;32(4):330–338. doi:10.1016/j.rapm.2007.02.010
50. Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modeling strategy based on available data. Lancet. 2008;372(9633):139–144. doi:10.1016/S0140-6736(08)60878-8
51. Chu KM. Operative mortality in resource-limited settings. Arch Surg. 2010;145(8):721. doi:10.1001/archsurg.2010.137
52. Nickerson JW, Chackungal S, Knowlton L, McQueen K, Burkle FM. Surgical care during humanitarian crises: a systematic review of published surgical caseload data from foreign medical teams. Prehosp Disaster Med. 2012;27(2):184–189. doi:10.1017/S1049023X12000556
53. Wong EG, Gupta S, Deckelbaum DL, Razek T, Kushner AL. Prioritizing injury care: a review of trauma capacity in low and middle-income countries. J Surg Res. 2015;193(1):217–222. doi:10.1016/j.jss.2014.08.055
54. Alvarado O, Trelles M, Tayler-Smith K, et al. Orthopaedic Surgery in natural disaster and conflict settings: how can quality care be ensured? Int Orthop. 2015;39(10):1901–1908. doi:10.1007/s00264-015-2781-z
55. Pierre O, Lovejoy JF, Stanton R, et al. The use of emergency physicians to deliver anesthesia for orthopaedic surgery in austere environments: the expansion of the emergency physician’s general anesthesia syllabus to orthopaedic surgery. J Bone Joint Surg Am. 2018;100(7):e44. doi:10.2106/JBJS.16.01481
56. Wong EG, Razek T, Elsharkawi H, et al. Promoting quality of care in disaster response: a survey of core surgical competencies. Surg (United States). 2015;158(1):78–84. doi:10.1016/j.surg.2015.02.011
57. Chu K, Stokes C, Trelles M, Ford N. Improving effective surgical delivery in humanitarian disasters: lessons from Haiti. PLoS Med. 2011;8(4):5. doi:10.1371/journal.pmed.1001025
58. Harders M, Malangoni MA, Weight S, Sidhu T. Improving operating room efficiency through process redesign. Surgery. 2006;140(4):509–516. doi:10.1016/j.surg.2006.06.018
59. Aubrun F, Valade N, Coriat P, Riou B. Predictive factors of severe postoperative pain in the post anesthesia care unit. Anesth Analg. 2008;106(5):1535–1541. doi:10.1213/ane.0b013e318168b2ce
60. Stark PA, Myles PS, Burke JA. Development and psychometric evaluation of a postoperative quality of recovery score. Anesthesiology. 2013;118(6):1332–1340. doi:10.1097/ALN.0b013e318289b84b
61. Pusat Krisis Kesehatan Kementrian Kesehatan Republik Indonesia. Bencana di Provinsi Nusa Tenggara Barat Akibat Gempa bumi 2018. Laporan Pusat Krisis Kesehatan Kementrian Kesehatan Republik Indonesia, Jakarta. [Center for Health Crisis, Ministry of Health of the Republic of Indonesia. Disastersin West Nusa Tenggara Province Due to the 2018 Earthquake. The Report of the Health Crisis Center ofthe Ministry of Health of the Republic of Indonesia, Jakarta]. 2018.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
