Back to Journals » Patient Preference and Adherence » Volume 14
The Added Value of a Behavioral Medicine Intervention in Physiotherapy on Adherence and Physical Fitness in Exercise-Based Cardiac Rehabilitation (ECRA): A Randomised, Controlled Trial
Authors Borg S, Öberg B , Nilsson L, Söderlund A , Bäck M
Received 10 October 2020
Accepted for publication 1 December 2020
Published 24 December 2020 Volume 2020:14 Pages 2517—2529
DOI https://doi.org/10.2147/PPA.S285905
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Sabina Borg,1,2 Birgitta Öberg,1 Lennart Nilsson,3 Anne Söderlund,4 Maria Bäck1,5
1Department of Health, Medicine and Caring Sciences, Unit of Physiotherapy, Linköping University, Linköping, Sweden; 2Department of Cardiology and Department of Health, Medicine and Caring Sciences, Linköping University, Linköping, Sweden; 3Department of Health, Medicine and Caring Sciences, Unit of Cardiovascular Sciences, Linköping University, Linköping, Sweden; 4Department of Physiotherapy, School of Health, Care and Social Welfare, Mälardalen University, Västerås, Sweden; 5Department of Occupational Therapy and Physiotherapy, Sahlgrenska University Hospital, Gothenburg, Sweden
Correspondence: Maria Bäck
Department of Health, Medicine and Caring Sciences, Unit of Physiotherapy, Linköping University, S-581 83, Linköping, Sweden
Tel +46 700 852795
Email [email protected]
Purpose: Despite beneficial effects, adherence to exercise-based cardiac rehabilitation (exCR) is low in patients with coronary artery disease (CAD). The aim of this study was to investigate adherence to and the effects of a behavioral medicine intervention in physiotherapy (BMIP) added to routine exCR care on the primary outcome of physical fitness compared with routine exCR care.
Patients and Methods: In a randomized, controlled trial, 170 patients with CAD (136 men), mean age 62.3 (7.9) years, were included at a Swedish university hospital. Patients were randomized 1:1 to routine exCR care (RC) or to a BMIP added to routine exCR care for four months, with a long-term follow-up at 12 months. The outcome assessment included submaximal aerobic exercise capacity, muscle endurance and self-reported physical activity and physical capacity.
Results: The four-month follow-up showed improvements in all outcomes for both groups, but changes did not differ significantly between the groups. Patients in the BMIP group were more adherent to exCR recommendations compared with the RC group (31% vs 19%) and a non-significant tendency towards the maintenance of submaximal aerobic exercise capacity over time was seen in the BMIP group, whereas patients in the RC group appeared to deteriorate.
Conclusion: Both groups improved significantly at the four-month follow-up, while the 12-month follow-up showed a non-significant tendency towards better long-term effects on submaximal aerobic exercise capacity and exercise adherence for a BMIP compared with RC. In spite of this, a better understanding of the role of a BMIP in enhancing adherence is needed.
Keywords: aerobic capacity, coronary artery disease, control theory, secondary prevention
Introduction
Coronary artery disease (CAD) is one of the leading causes of death worldwide.1 Mortality rates in CAD have decreased markedly in recent decades, due mainly to improved evidence-based treatment and reductions in cardiovascular risk factors. As a result, the proportion of patients in need of secondary prevention is increasing.2,3 In the treatment of CAD, secondary prevention administered through cardiac rehabilitation is an important contributor to mortality reduction.3 Exercise-based cardiac rehabilitation (exCR) is often described as a central part of cardiac rehabilitation and has been given high priority in international guidelines.4,5 Meta-analyses clearly indicate the positive health benefits of exCR in terms of reduced cardiovascular mortality and a reduced risk of hospital re-admission,6,7 as well as beneficial effects on cardiovascular risk factors,7 anxiety and depression8 and aerobic exercise capacity.9 The combination of both aerobic and resistance exercise has been shown to achieve the best effects on overall risk reduction and cardiovascular fitness.10 In patients with CAD, aerobic exercise capacity is a strong predictor of mortality and a small gain in oxygen uptake can therefore improve both functional capacity and survival prospects.11,12
In spite of its established positive effects, exCR remains underutilized in patients with CAD, with referral rates in Europe in recent decades of about 50% and with a minority of the referred patients actually attending and adhering to exCR.13 In Sweden in 2019, only 19% of referred patients completed an exCR program during the first year after an acute myocardial infarction.14 A recent Cochrane Review has found insufficient evidence of the effects of interventions aiming to increase adherence to exCR.15 The ability to determine the consistency of findings was limited due to multifaceted, varied interventions and more research is needed.15 Behavioral medicine interventions have previously been shown to be effective in healthy adults and self-monitoring has been shown to be the most important component for a behavioral change to be successful when changing exercise behaviour.16 It has also been shown that interventions that combined self-monitoring with other components, such as goal-setting or feedback on behavior/exercise, were more effective in promoting physical activity than other evaluated interventions.16 A few studies have used a behavioral medicine intervention in the context of exCR in order to increase adherence to exercise programmes.15,17–19 One review has shown that self-monitoring and goal-setting may be effective behavioral change techniques to increase physical activity levels in patients with CAD. Knowledge of interventions evaluating the effects of behavioral medicine interventions in the context of exCR is still limited, however, and further high-quality research is needed. By promoting adherence to exCR, the effectiveness of this treatment in terms of improved aerobic exercise capacity is likely to be increased and this would in turn affect cardiovascular mortality. The aim of the present study was to investigate adherence to and the effects of a behavioral medicine intervention added to routine exCR care on the primary outcome of physical fitness compared with routine exCR care.
Patients and Methods
Study Design
This study is an open-label, randomized, controlled trial.
Subjects
Patients were screened consecutively for study inclusion at a coronary care unit at a Swedish university hospital. The inclusion criteria were an index event due to CAD and/or percutaneous coronary intervention (PCI), age ≥ 18 years and < 75 years. The exclusion criteria were serious physical or psychological disease interfering with participation in exCR and an inability to understand the Swedish language. The study is performed in accordance with the principles stated in the Declaration of Helsinki. Ethical approval was obtained from the regional ethical review board in Linköping, Sweden in 2015 (Registration number: 2015/209-31), and with an amendment in 2018 (Registration number: 2018/383-32). The study is registered at ClinicalTrials.gov (NCT02895451). All patients gave their informed written consent before entering the study.
Inclusion Procedure and Randomization
Physiotherapists at the coronary care unit received, through patient records, daily information about patients eligible for inclusion in the study, asked potential patients about participation and obtained informed consent. Baseline testing, performed by the physiotherapist responsible for the testing procedure, took place within two to three weeks after discharge. After completed baseline tests, patients were randomized 1:1, using sealed envelopes, to either routine exCR care (RC) or to a behavioral medicine intervention in physiotherapy (BMIP), in addition to routine exCR care for four months. Randomization was stratified by submaximal aerobic work capacity and a cut-off at 100 watts was used.20 The physiotherapists performing the tests were not blinded to group allocation for organizational reasons. Different physiotherapists were responsible for the testing procedure and the behavioral medicine intervention. Details about the methods in this study have been given in the previously published study protocol.20
Intervention
Routine exCR Care
Patients randomized to RC followed routine exCR care. The exercise program was individually prescribed, based on tests of physical fitness, and consisted of hospital-based continuous aerobic exercise two days/week for 20–60 minutes/session at an intensity of 40–80% of VO2max, corresponding to 12–17 according to Borg´s Rating of Perceived Exertion Scale, and resistance exercise containing 8–10 different exercises, 10–15 repetitions in 1–3 sets.4,5 In order to achieve the recommendation of at least three aerobic exercise sessions/week, patients were instructed to perform one additional home-based aerobic exercise session/week. Following routine exCR care, patients were also able to choose to perform their entire exCR in a home-based setting. Home-based exercise sessions were registered by the patients in an exercise diary. The exercise diary was not followed up by a physiotherapist during the exCR period and no other structured interventions to control or increase exercise adherence were parts of routine care.
Behavioral Medicine Intervention
Patients in the intervention group received a BMIP added to routine exCR care, with the aim of increasing adherence to the prescribed exercise program and thereby also with the potential to affect physical fitness. The behavioral change techniques used in this study, ie specific goal-setting, re-evaluation of the goals, self-monitoring and feedback, are based on the control theory (CT).21 CT describes a model of self-regulation that can be used in the analysis of human behavior. CT is part of the Social Cognitive Theory of Self-Regulation22 in which the importance of self-efficacy is emphasized and goal-setting and self-monitoring are central behavioral change techniques23 in supporting an increase in self-efficacy for adherence to exCR in our study. Providing feedback on performance is also included in the CT.21
Specific Goal-Setting and Re-Evaluation of Goals
Figure 2 illustrates an overview of the timeline of the behavioral medicine intervention. Initially, the patients met a physiotherapist for detailed planning and specific goal-setting for the exCR program. Specific goal-setting according to the CT involves detailed planning that specifies what to do, the exercise dose and the context in which the exercise is performed.21 Since the intervention in this study has a patient-centered approach, it was important that the detailed planning for the exCR program (what to do, the exercise dose and the context for exercise) was agreed between the patient and the physiotherapist. In relation to achieving the exercise goals, possible facilitators and barriers were identified and an action plan with strategies to promote facilitators and overcome barriers was developed together with the patient. The patient’s motivation and self-efficacy for the exCR program were also discussed in relation to the goals set. In accordance with CT,21 the exercise goals were re-evaluated during and at the end of the intervention period.
 |
Figure 1 Flowchart of study participants. |
Self-Monitoring and Feedback
In accordance with CT,21 the patients self-monitored their exercise goal, including a specification of the performed exercise dose, in an exercise diary. The exercise diary was followed up by a physiotherapist every three weeks and the patients received positive feedback on achieved goals, supporting feedback in relation to barriers and the opportunity to discuss strategies to increase adherence. At nine weeks, visual feedback on physical activity levels, using accelerometer cut-points to classify the measured physical activity into different intensity levels, was also given.
At the end of the intervention (16 weeks), a follow-up meeting with the physiotherapist took place to discuss how the intervention had been perceived, goal achievement and to set a long-term exercise goal.
To summarize, the behavioral medicine intervention contained one face-to-face meeting (baseline), three structured telephone/face-to-face follow-ups (3, 6 and 12 weeks), one face-to-face follow-up for visual feedback (9 weeks) and one face-to-face meeting at the end of the intervention (16 weeks).
Outcomes
Exercise Adherence
Exercise adherence was defined as “the extent to which a patient acts in accordance with the advised interval, exercise dose and exercise dosing regimen”.24 In the current study, we chose a definition of exercise adherence of meeting at least 75% of the recommended exercise dose according to exCR guidelines.4,5 This definition is used in accordance with both European position statement recommendations and the Swedish SWEDEHEART quality registry.14,25 Exercise adherence was calculated from patient records and exercise diaries.
Physical Fitness
Clinical and demographic patient characteristics were collected from medical records and patient interviews. Outcome assessments at baseline, four and 12 months included the variables listed below, apart from self-rated physical capacity, which was only measured at four and 12 months. All outcomes, with the exception of self-reported physical activity, are part of routine exCR care in Sweden, are included in the Swedish SWEDEHEART quality registry and have been found to be reliable for patients with CAD.26,27
Primary Outcome
Submaximal Aerobic Exercise Capacity
Submaximal aerobic exercise capacity (watts, (W)) was evaluated with a submaximal exercise test on a bicycle ergometer, according to the modified WHO protocol.28 The test has been found to be reliable for patients with CAD and has been described in detail elsewhere.26
Secondary Outcomes
Muscle Endurance
Muscle endurance was evaluated by the number of repetitions performed on two clinical muscle endurance tests for lower (unilateral isotonic heel lift) and upper extremities (unilateral isotonic shoulder flexion).26
Self-Reported Physical Activity and Physical Capacity
The level of physical activity was measured using two indicator questions regarding physical activity from the Swedish National Board of Health and Welfare (the BHW PA questions),29 while physical capacity was measured on a visual analogue scale according to the SWEDEHEART registry.27 The BHW PA questions consist of two questions regarding total time of exercise (high intensity) and everyday physical activity (moderate intensity) during a regular week, specified in fixed response alternatives. The results for the two questions are merged into a new dimension called “activity minutes”. The BHW PA questions have been found to be valid for adults in Sweden.29 Patients also self-rated their physical capacity on a visual analogue scale (VAS) ranging from 0–100, where 0 is the worst possible state and 100 the best possible state of physical capacity.27
Statistical Methods
Descriptive statistics were used for demographic data and are presented as means and standard deviations (SD), or numbers and proportions (%), as appropriate. Since the data on submaximal aerobic exercise capacity, muscle endurance, self-reported physical activity and physical capacity were normally distributed, differences between groups were tested with an independent samples t-test and, for comparisons within groups, a paired t-test was used. An intention-to-treat and a per-protocol analysis were performed. Missing values for submaximal aerobic exercise capacity, muscle endurance, self-reported physical activity and physical capacity were handled with multiple imputation. Demographic data, patient records and outcome measurements at baseline were included as independent variables, while outcome measurements at 16 weeks and one year were entered as both independent and dependent variables in the multiple imputation models. Multiple imputation using the chained equations procedure (fully conditional specification method in SPSS) with 10 data sets was used.30 Constraints were applied to each variable according to the minimum and maximum value from observed data, except for self-reported physical capacity, for which the range of the scale (0–100) was used. The results of the pooled analyses were used for each of the variables. A response analysis on demographic data and outcome measurements at baseline was performed, comparing patients with complete data at 16 weeks follow-up and patients without complete data at 16 weeks follow-up. No substantial differences were revealed, whereby missing at random could be assumed. Statistical analysis was performed using SPSS statistical software for Windows (SPSS Version 25, IBM Corporation, New York, USA).
Sample Size Calculation
Sample size calculation was based on data from a similar clinical exCR setting (n=50) for differences in submaximal aerobic exercise capacity (W), before and after a completed exCR program. The estimated total sample size was 160 patients in order to detect a least mean difference at 10W (SD 20W), with a power of 80%, a two-sided significance level of p < 0.05 and a calculated loss to follow-up of 20%. To compensate for a possible larger loss to follow-up, an additional 10 patients were recruited.
Results
Study Population and Demographic Data
Of 453 consecutively screened patients, a total of 170 patients were included. The enrolment period extended from January 2016 to October 2018. The study flowchart is presented in Figure 1. The mean (standard deviation) age was 62.3 (7.9) years and 136 (80%) were men.
 |
Figure 2 Overview of the timeline of the behavioral medicine intervention. |
There were no major differences in baseline demographics between the groups (Table 1). However, a significantly lower proportion of non-ST-elevation myocardial infarction (p=0.037) and a correspondingly higher proportion of unstable angina (p=0.011), as the index cardiac event, were seen in the BMIP group. No statistical differences between the groups were found in submaximal aerobic exercise capacity and muscle endurance at baseline. Patients in the BMIP group had a significantly higher number of activity minutes in the BHW PA questions at baseline (309.1 vs 243.8 activity minutes, p=0.004), compared with patients in the RC group.
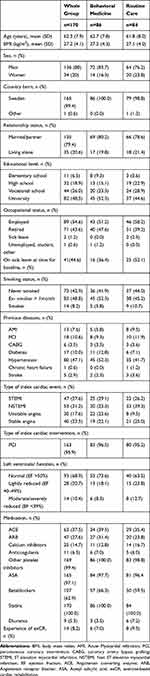 |
Table 1 Baseline Demographics for Participants in the ECRA-Study, n=170 |
The largest proportion of patients in both groups chose to perform the exCR in a home-based setting (n=55 in BMIP and n=58 in RC respectively), whereas 20 patients in each group participated in hospital-based exCR. Five (RC) and 10 (BMIP) patients respectively chose to participate once a week in hospital-based exCR in combination with home-based exercise. Data on the choice of exercise setting were missing for one patient in each group due to early exclusion after baseline tests (critical ischaemia or other disease). No serious adverse events related to exCR or the behavioral medicine intervention were reported. The following events were noted; back strain (BMIP: n=2), foot injury/sprain (BMIP: n=3, RC: n=1), dizziness (RC: n=1), knee pain (BMIP: n=1), heel spurs (BMIP: n=1) and joint or muscle pain (BMIP: n=1, RC: n=3).
Adherence to Intervention
One hundred and forty-five of 170 patients (BMIP: n=75 and RC: n=70) had data from patient records and/or exercise diaries and could be included in the evaluation of exercise adherence. Twenty-three (31%) patients in the BMIP group and 13 (19%) patients in the RC group were considered to have adhered to the exCR program. Patients in both groups were more adherent to aerobic exercise than to resistance exercise, with 43 (57%) in the BMIP group and 31 (44%) in the RC group meeting the adherence definition of at least 75% of the recommended aerobic exercise dose.
Primary Outcome
There were no significant differences between the two groups in terms of the change in submaximal aerobic exercise capacity either between baseline and 16 weeks or between 16 weeks and 12 months (Table 2). Nonetheless, a non-significant tendency towards the maintenance of submaximal aerobic exercise capacity in the BMIP group (118.3 vs 120.0 W, p=0.333) and a deterioration in the RC group (115.3 vs 111.6 W, p=0.095) was found between the end of the intervention (16 weeks) and the long-term follow-up (12 months).
 |
Table 2 Intention-to-Treat Analysis of Change in Outcomes Within and Between Groups |
Secondary Outcomes
No significant differences between the groups for any of the secondary outcomes were found (unilateral isotonic heel lift, unilateral isotonic shoulder flexion, the BHW PA questions and the VAS physical capacity), between baseline and 16 weeks or between 16 weeks and 12 months (Table 2).
Differences Within the Groups
Both groups improved significantly in all outcomes between baseline and 16 weeks, but there was no significant difference in change within groups between 16 weeks and the 12-month follow-up (Table 2).
Per-Protocol Analysis Within and Between Groups
Similar to the results of the intention-to-treat analysis, no significant differences in change between the groups were found (Table 3). Adherent patients in both groups improved significantly in all outcomes between baseline and 16 weeks (Table 3). Adherent patients in both groups also had higher outcome values (except for unilateral shoulder flexion in the RC group) at 16 weeks and at 12 months, compared with the results of the intention-to-treat analysis. Baseline values were also slightly higher for adherent patients in both groups (except for unilateral isotonic heel lift in the BMIP group).
 |
Table 3 Per-Protocol Analysis of Change in Outcomes Within and Between Groups |
Submaximal aerobic exercise capacity was also evaluated in the 43 patients in the BMIP group and the 31 patients in the RC group who were adherent to aerobic exercise alone. The results showed a non-significant tendency similar to the intention-to-treat analysis, i.e. a further improvement in the BMIP group (127.76 vs 130.51 W) and a deterioration in the RC group (123.94 vs 121.11 W) between 16 weeks and the 12-month follow-up.
Discussion
This study presents the results of one of the first randomized, controlled studies to investigate adherence to and the effects of a behavioral medicine intervention in physiotherapy, containing goal-setting, self-monitoring and feedback, on the primary outcome of physical fitness in exCR compared with routine exCR care. Patients in the BMIP group were more adherent to exCR recommendations than those in the RC group, but similar significant improvements in all outcomes were found in both groups at the 16-week follow-up. For the sustainable effect of physical fitness after the completion of exCR, the non-significant tendency towards a positive long-term effect on submaximal aerobic exercise capacity shown in this study is interesting and may indicate that a BMIP can be effective in supporting exercise adherence over time.
Continuing to exercise according to guidelines after the completion of an exCR-program has proven to be difficult.31,32 Studies have shown that fewer than 50% maintain an exercise regimen for six months or longer after the completion of an exCR programme31,32 and only 16% of European patients with CAD performed vigorous physical activity, ≥ 20 minutes, at least three times/week, one year after the index event.33 Since aerobic exercise capacity is a strong predictor of mortality in patients with CAD and a small exercise-induced gain can have a positive impact on survival prospects,11,12 it is essential that cardiac patients preserve the effects of exCR on physical fitness and continue to follow a regular exercise program over time. In the present study, a non-significant tendency towards the maintenance of submaximal aerobic exercise capacity in the BMIP group and a deterioration in the RC group was found between the end of the intervention (16 weeks) and a long-term follow-up (12 months). The non-significant tendency towards the maintenance of submaximal aerobic exercise capacity in the BMIP group and a deterioration in the RC group could possibly be explained by the sustained effects of the behavioral change supporting the intervention over time. Previous research has shown that behavioral medicine interventions are effective in increasing physical activity both in healthy adults and in cardiac patients.16,17,34 However, more studies that evaluate the effectiveness of behavioral medicine interventions, specifically on physical fitness, are needed. Findings from the review by Ferrier et al17 support self-monitoring and goal-setting as behavioral change techniques that may be effective in increasing physical activity in the post-CR context. This review was, however, limited by the small number of studies and the lack of a clear description of the behavioral interventions.17 The current study used goal-setting, feedback and self-monitoring based on the control theory.21 A combination of different behavioral change techniques, such as those used in our study, has previously been found to be effective in promoting physical activity behavior following the completion of CR programs in small study samples,35 as well as in healthy adults.16 The results of the present study are consistent with the results of a recent Cochrane Review, in which subgroup analyses did not reveal any significant differences between groups for theory-based interventions in a CR setting.15 Only a few interventions have been shown to improve adherence to exCR.15 Lynggaard et al19 found that the addition of learning and coping strategies improved adherence to a short eight-week exCR program, but the study lacked a long-term follow-up.19 Sniehotta et al18 showed that an intervention based on action planning and coping planning could enhance physical exercise and adherence in CR patients.18
It has been suggested that the evaluation of adherence levels, screening for non-adherence and promoting adherence to secondary prevention therapies should be included in the core components of a modern CR programme.5 Tailoring the exCR program based on patients’ preferences and the integration of the patients’ perspectives may help to increase uptake and adherence.5 The patients in the present study were given the choice of performing the exCR in a hospital-based, home-based or a combined setting. The proportion of patients in the different settings was representative of routine clinical practice. International guidelines support centre-based, supervised exCR,4,5 but various strategies for increasing uptake and adherence to exCR are ongoing, including home-based programmes and E-health solutions.36–40 However, the efficacy of these alternative intervention models still needs to be further investigated.40 A recent Cochrane Review by Santiago et al,15 focusing on interventions to promote the utilization of CR, found better effects on adherence when offered remotely. However, these findings should be interpreted with caution. The subgroup analysis supporting these findings has been performed on only a few studies with a relatively small study population. Furthermore, adherence ascertainment in supervised and unsupervised settings may not be comparable.15 Adherence to exCR is still a matter of concern and more research is needed to determine the appropriate organization of the programme.5
The results of the present study regarding improved aerobic exercise capacity after participation in exCR are in line with a newly published European position statement,25 which reports an expected improvement in aerobic exercise capacity of at least 5–10%.25 The mean change in submaximal aerobic exercise capacity before and after the exCR program in our study was also in line with Swedish quality registry data, which reports a mean change of 12.1 W (13.4%).14
A newly published position paper from the European Society of Cardiology5 emphasizes the need to increase uptake and adherence to secondary prevention through CR in order to realize the considerable potential for further reductions in cardiovascular mortality.5 The current study showed better exercise adherence to a behavioral medicine intervention added to exCR (31%) compared with routine exCR care (19%). Exercise adherence in the RC group was identical to the percentage of referred patients who completed a hospital-based exCR program in Sweden in 2019,14 whereas exercise adherence in the BMIP group was higher. Reports of adherence to recommended exercise guidelines from earlier studies vary widely, from levels of 30% up to 110%.41 The interpretation of the results is limited by the large variation in the exercise prescription methodologies used in different studies, as well as the basic definition of what constitutes exercise adherence.41 In our study, we used the same definition of exercise adherence (meeting at least 75% of the recommended exercise dose according to exCR guidelines), as used in both European position statement recommendations and the Swedish SWEDEHEART quality registry,14,25 but, as previous studies have also shown,13 realizing the definition of exCR adherence is a challenge.
Strengths and Limitations
One strength in the current study is its randomized, controlled design, which is regarded as the golden standard for examining whether a particular treatment is effective. Another strength is that the behavioral change techniques used in the present study are grounded in a theoretical framework,21 which has been shown to be effective in interventions in other patient groups42,43 and also specifically in cardiac patients.17,35 The behavioral medicine intervention used in our study requires no additional education or materials and can therefore be implemented as part of existing routine exCR care. Moreover, this study provides a long-term follow-up at 12 months, which enables analyses of the sustained effects of the behavioral change supporting interventions over time.
This study was conducted with a single-center design, which is a limitation, as it may affect the generalizability of the results. Furthermore, the per-protocol analysis was limited by the small number of patients in each group. The patients in the present study managed a higher workload on the symptom-limited bicycle ergometer test both at baseline and after the completed exCR period, compared with patients registered in the Swedish SWEDEHEART quality registry. This could be explained by selection bias, where participants in the current study are more prone to exercise, compared with patients with CAD in general. Moreover, the present study included patients up to the age of 75 years, while the age limit in SWEDEHEART has recently been increased to 80 years. In this study, the use of randomization, together with a lower loss to follow-up than calculated, minimized the effect of a possible selection bias. Due to organizational aspects, it was not possible to blind the physiotherapists performing the tests to group allocation. However, the test procedure was validated between the involved physiotherapists and standardized test protocols were used. Furthermore, group allocation was kept confidential to patients. Finally, exercise adherence was evaluated with self-reported exercise diaries, which may involve limitations in terms of accuracy and overestimation.
Conclusion
This study shows significant improvements in all outcomes for both groups at 16 weeks (end of intervention) and a non-significant tendency towards a behavioral medicine intervention in physiotherapy, added to routine exCR care, having better long-term effects on submaximal aerobic exercise capacity compared with routine exCR care. Patients who received a BMIP had better exercise adherence than RC patients. The improvement in physical fitness after participation in an exCR-program for both groups matches that identified in previous studies. Interventions that promote adherence and stimulate the maintenance of physical fitness and continued regular exercise habits, even after the completion of exCR, are important in order to realize the considerable opportunities for further reductions in cardiovascular mortality. A better understanding of the role played by a behavioral medicine intervention in physiotherapy in enhancing adherence and the effects on physical fitness in exCR could assist and improve the secondary prevention of patients with CAD.
Abbreviations
BHW PA, the Swedish National Board of Health and Welfare physical activity; BMIP, behavioral medicine intervention in physiotherapy; CAD, coronary artery disease; CT, control theory; exCR, exercise-based cardiac rehabilitation; PCI, percutaneous coronary intervention; RC, routine exercise-based cardiac rehabilitation care; SD, standard deviation; VAS, visual analogue scale.
Data Sharing Statement
The data generated and analysed during the present study are not publicly available but can be obtained from the corresponding author in response to a reasonable request.
Acknowledgments
The authors wish to thank the physiotherapists at the coronary care unit at which the study took place for their practical support with enrolment and the testing procedure.
Funding
This study was funded by the Swedish Heart and Lung Association and the Swedish Society of Medical Research, together with grants from Region Östergötland. These funding sources played no role in the design of this study, the data collection, the analysis and interpretation of data or in writing the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. WHO. The top 10 causes of death. Updated May 24, 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
2. Bjorck L, Rosengren A, Bennett K, Lappas G, Capewell S. Modelling the decreasing coronary heart disease mortality in Sweden between 1986 and 2002. Eur Heart J. 2009;30(9):1046–1056. doi:10.1093/eurheartj/ehn554
3. Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356(23):2388–2398. doi:10.1056/NEJMsa053935
4. Balady GJ, Williams MA, Ades PA, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115(20):2675–2682. doi:10.1161/circulationaha.106.180945
5. Ambrosetti M, Abreu A, Corrà U, et al. Secondary prevention through comprehensive cardiovascular rehabilitation: from knowledge to implementation. 2020 update. A position paper from the secondary prevention and rehabilitation section of the European Association of preventive cardiology. Eur J Prev Cardiol. 2020:2047487320913379. doi:10.1177/2047487320913379
6. Anderson L, Oldridge N, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart disease: cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67(1):1–12. doi:10.1016/j.jacc.2015.10.044
7. Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: a systematic review and meta-analysis of randomized controlled trials. Am Heart J. 2011;162(4):571–584.e2. doi:10.1016/j.ahj.2011.07.017
8. Verschueren S, Eskes AM, Maaskant JM, Roest AM, Latour CHM, Op Reimer WS. The effect of exercise therapy on depressive and anxious symptoms in patients with ischemic heart disease: a systematic review. J Psychosom Res. 2018;105:80–91. doi:10.1016/j.jpsychores.2017.11.018
9. Sandercock G, Hurtado V, Cardoso F. Changes in cardiorespiratory fitness in cardiac rehabilitation patients: a meta-analysis. Int J Cardiol. 2013;167(3):894–902. doi:10.1016/j.ijcard.2011.11.068
10. Marzolini S, Oh PI, Brooks D. Effect of combined aerobic and resistance training versus aerobic training alone in individuals with coronary artery disease: a meta-analysis. Eur J Prev Cardiol. 2012;19(1):81–94. doi:10.1177/1741826710393197
11. Kavanagh T, Mertens DJ, Hamm LF, et al. Prediction of long-term prognosis in 12 169 men referred for cardiac rehabilitation. Circulation. 2002;106(6):666–671. doi:10.1161/01.cir.0000024413.15949.ed
12. De Schutter A, Kachur S, Lavie CJ, et al. Cardiac rehabilitation fitness changes and subsequent survival. Eur Heart J Qual Care Clin Outcomes. 2018;4(3):173–179. doi:10.1093/ehjqcco/qcy018
13. Kotseva K, Wood D, De Bacquer D. Determinants of participation and risk factor control according to attendance in cardiac rehabilitation programmes in coronary patients in Europe: EUROASPIRE IV survey. Eur J Prev Cardiol. 2018;25(12):1242–1251. doi:10.1177/2047487318781359
14. Jernberg T. SWEDEHEART annual report 2019. 2020.
15. Santiago de Araujo Pio C, Chaves GS, Davies P, Taylor RS, Grace SL. Interventions to promote patient utilisation of cardiac rehabilitation. Cochrane Database Syst Rev. 2019;2:Cd007131. doi:10.1002/14651858.CD007131.pub4
16. Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701. doi:10.1037/a0016136
17. Ferrier S, Blanchard CM, Vallis M, Giacomantonio N. Behavioural interventions to increase the physical activity of cardiac patients: a review. Eur J Cardiovasc Prev Rehabil. 2011;18(1):15–32. doi:10.1097/HJR.0b013e32833ace0e
18. Sniehotta FF, Scholz U, Schwarzer R. Action plans and coping plans for physical exercise: a longitudinal intervention study in cardiac rehabilitation. Br J Health Psychol. 2006;11(Pt 1):23–37. doi:10.1348/135910705x43804
19. Lynggaard V, Nielsen CV, Zwisler AD, Taylor RS, May O. The patient education - learning and coping strategies - improves adherence in cardiac rehabilitation (LC-REHAB): a randomised controlled trial. Int J Cardiol. 2017;236:65–70. doi:10.1016/j.ijcard.2017.02.051
20. Borg S, Oberg B, Nilsson L, Soderlund A, Back M. The role of a behavioural medicine intervention in physiotherapy for the effects of rehabilitation outcomes in exercise-based cardiac rehabilitation (ECRA) - the study protocol of a randomised, controlled trial. BMC Cardiovasc Disord. 2017;17(1):134. doi:10.1186/s12872-017-0557-7
21. Carver CS, Scheier MF. Control theory: a useful conceptual framework for personality-social, clinical, and health psychology. Psychol Bull. 1982;92(1):111–135. doi:10.1037/0033-2909.92.1.111
22. Bandura A. Human agency in social cognitive theory. Am Psychol. 1989;44(9):1175–1184. doi:10.1037/0003-066x.44.9.1175
23. Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process. 1991;50:248–287. doi:10.1016/0749-5978(91)90022-L
24. Conraads VM, Deaton C, Piotrowicz E, et al. Adherence of heart failure patients to exercise: barriers and possible solutions: a position statement of the Study Group on exercise training in heart failure of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2012;14(5):451–458. doi:10.1093/eurjhf/hfs048
25. Abreu A, Frederix I, Dendale P, et al. Standardization and quality improvement of secondary prevention through cardiovascular rehabilitation programmes in Europe: the avenue towards EAPC accreditation programme: a position statement of the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology (EAPC). Eur J Prev Cardiol. 2020:2047487320924912. doi:10.1177/2047487320924912
26. Hellmark M, Back M. Test-retest reliability and responsiveness to change of clinical tests of physical fitness in patients with acute coronary syndrome included in the SWEDEHEART register. Eur J Cardiovasc Nurs. 2018;17(6):486–495. doi:10.1177/1474515117743978
27. SWEDEHEART. Fysioterapi SEPHIA. UCR. 20200102. Updated December 23, 2016. Available from: https://www.ucr.uu.se/swedeheart/dokument-sephia/fysioterapi-sephia/sjaelvupplevd-fysisk-aktivitet-sephia-161223/viewdocument.
28. Exercise tests in relation to cardiovascular function. Report of a WHO meeting. World Health Organ Tech Rep Ser. 1968;388:1–30.
29. Olsson SJ, Ekblom O, Andersson E, Borjesson M, Kallings LV. Categorical answer modes provide superior validity to open answers when asking for level of physical activity: a cross-sectional study. Scand J Public Health. 2016;44(1):70–76. doi:10.1177/1403494815602830
30. Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20(1):40–49. doi:10.1002/mpr.329
31. Daly J, Sindone AP, Thompson DR, Hancock K, Chang E, Davidson P. Barriers to participation in and adherence to cardiac rehabilitation programs: a critical literature review. Prog Cardiovasc Nurs. 2002;17(1):8–17. doi:10.1111/j.0889-7204.2002.00614.x
32. Moore SM, Dolansky MA, Ruland CM, Pashkow FJ, Blackburn GG. Predictors of women’s exercise maintenance after cardiac rehabilitation. J Cardiopulm Rehabil. 2003;23(1):40–49. doi:10.1097/00008483-200301000-00008
33. Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry. Eur J Prev Cardiol. 2019;26(8):824–835. doi:10.1177/2047487318825350
34. Tierney S, Mamas M, Skelton D, et al. What can we learn from patients with heart failure about exercise adherence? A systematic review of qualitative papers. Health Psychol. 2011;30(4):401–410. doi:10.1037/a0022848
35. Chase JA. Systematic review of physical activity intervention studies after cardiac rehabilitation. J Cardiovasc Nurs. 2011;26(5):351–358. doi:10.1097/JCN.0b013e3182049f00
36. Devi R, Singh SJ, Powell J, Fulton EA, Igbinedion E, Rees K. Internet-based interventions for the secondary prevention of coronary heart disease. Cochrane Database Syst Rev. 2015;12:Cd009386. doi:10.1002/14651858.CD009386.pub2
37. Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016;102(15):1183–1192. doi:10.1136/heartjnl-2015-308966
38. Verburg A, Selder JL, Schalij MJ, Schuuring MJ, Treskes RW. eHealth to improve patient outcome in rehabilitating myocardial infarction patients. Expert Rev Cardiovasc Ther. 2019;17(3):185–192. doi:10.1080/14779072.2019.1580570
39. Anderson L, Sharp GA, Norton RJ, et al. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6(6):Cd007130. doi:10.1002/14651858.CD007130.pub4
40. Xia TL, Huang FY, Peng Y, et al. Efficacy of different types of exercise-based cardiac rehabilitation on coronary heart disease: a network meta-analysis. J Gen Intern Med. 2018;33(12):2201–2209. doi:10.1007/s11606-018-4636-y
41. Deka P, Pozehl B, Williams MA, Yates B. Adherence to recommended exercise guidelines in patients with heart failure. Heart Fail Rev. 2017;22(1):41–53. doi:10.1007/s10741-016-9584-1
42. Holm S, Ljungman G, Åsenlöf P, Linton SJ, Söderlund A. Treating youth in pain: comparing tailored behavioural medicine treatment provided by physical therapists in primary care with physical exercises. Eur J Pain. 2016;20(4):626–638. doi:10.1002/ejp.780
43. Cederbom S, Rydwik E, Söderlund A, Denison E, Frändin K, von Heideken Wågert P. A behavioral medicine intervention for older women living alone with chronic pain - a feasibility study. Clin Interv Aging. 2014;9:1383–1397. doi:10.2147/cia.S66943
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
