Back to Journals » Clinical Ophthalmology » Volume 17
The Accuracy of Flap Thickness and Diameter in LASIK Using a Femtosecond Laser
Received 22 July 2023
Accepted for publication 5 December 2023
Published 13 December 2023 Volume 2023:17 Pages 3877—3882
DOI https://doi.org/10.2147/OPTH.S431885
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Stephen A Wexler,1,2 Brad Hall3
1John F. Hardesty, MD Department of Ophthalmology and Visual Sciences, Washington University School of Medicine, St Louis, MO, USA; 2Bismarck LASIK, pLLC, Bismarck, ND, USA; 3Sengi, Penniac, NB, Canada
Correspondence: Stephen A Wexler, Bismarck LASIK, 620 North 9th Street, Bismarck, ND, 58501, USA, Tel +1 701-222-2020, Email [email protected]
Purpose: To evaluate the resultant thickness of the WaveLight FS200 (Alcon Vision, LLC) created LASIK flap compared to intended thickness at the surgical visit, using the WaveLight EX500 (Alcon Vision, LLC) pachymeter and the resultant flap diameter compared to intended diameter.
Methods: This single arm, prospective, single surgeon study assessed the accuracy of the intended flap thickness and diameter, after successful bilateral LASIK surgery. The WaveLight FS200 femtosecond laser was used to create all flaps with an intended thickness of 120 μm. Flap thickness was calculated by subtracting the stromal bed thickness after flap lift from the preoperative corneal thickness using the WaveLight EX500 on-board optical pachymeter. Flap diameter was determined using digital analysis.
Results: A total of 58 subjects (116 eyes) completed the study. The calculated mean flap thickness was 120.6 ± 9.0 μm (range 102 to 143 μm) using the EX500 pre- and post-flap pachymetry measurements. There was no statistically significant difference between the planned and achieved flap thickness (p > 0.05). The mean difference in flap diameter between planned and actual was 0.02 ± 0.05 mm. Corneal thickness measured by Pentacam at up to 2 months preoperatively versus EX500 just prior to surgery was similar, with EX500 measuring 2 μm less on average than the Pentacam.
Conclusion: The results suggest that the WaveLight FS200 laser is reliable for LASIK flap thickness and diameter and accurately created flaps at the intended thickness and the intended diameter.
Plain Language Summary: Laser vision correction (LVC) is a popular procedure to treat refractive error and reduce or eliminate the need for spectacles. Laser in situ keratomileusis (LASIK) is one of the most common LVC procedures. With LASIK, a flap is created (using a manual blade or a femtosecond laser) in the cornea (the transparent front of the eye) and lifted to expose stromal tissue. Some of the stromal tissue is then removed by a laser to reshape the cornea and correct refractive error. Creating a flap at the desired thickness and diameter is crucial for good outcomes after LASIK. The purpose of this study was to evaluate the thickness and diameter of LASIK flaps that were created with a femtosecond laser. The results of this study suggest that the femtosecond laser accurately creates a flap at the intended thickness and at the intended diameter.
Keywords: LASIK, WaveLight FS200, WaveLight EX500, femtosecond laser, flap creation
Introduction
Laser in situ keratomileusis (LASIK) is one of the most common refractive procedures performed worldwide. By reshaping the cornea, it can be used to correct myopia, hyperopia, and astigmatism. However, for successful LASIK outcomes, the flap must be created in a safe and predictable manner.1 First, the achieved flap thickness must be very close to target thickness. A flap that is too thick may compromise the residual stroma and increase the risk for corneal ectasia.2 A flap that is too thin may lead to corneal haze, flap slippage, buttonholes, or striae.3 Second, the flap diameter must also be close to the target diameter. A flap that is larger in diameter than intended may increase the risk for postoperative dry eye as more corneal nerves may be damaged.4
To create the flap in LASIK, a manual keratome or a femtosecond laser can be used, although femtosecond lasers in refractive surgery may offer benefits over the manual keratome.5–7 The WaveLight FS200 (Alcon Vision, LLC) is one available femtosecond laser. It has been reported to create accurate flap thicknesses as measured by optical coherence tomography (OCT),8,9 ultrasonic pachymetry,10 and high frequency ultrasound biomicroscopy (HF-UBM).7 The WaveLight FS200 is fully integrated with an excimer laser (WaveLight EX500, Alcon Vision, LLC), which has a noncontact optical pachymeter. The on-board pachymeter can allow for measurements of corneal and flap thicknesses pre- and post-ablation and intraoperatively. There have been retrospective studies of flap thickness created with the WaveLight FS200 using the on-board pachymeter of the WaveLight EX500.6,11 However, to date, there are minimal prospective data. The purpose of this study was to evaluate the resultant thickness of the WaveLight FS200 created LASIK flap compared to plan at the surgical visit, using the WaveLight EX500 pachymeter and the resultant flap diameter compared to intended diameter.
Methods
This was a prospective, single arm, single surgeon, observational study of the accuracy of flap thickness and diameter using a femtosecond laser in LASIK surgery. The study was conducted at a private practice, therefore an independent institutional review board (IRB) was used. Salus IRB reviewed and approved the study (approval SW-22-001). All subjects gave written informed consent, and this study was conducted in compliance with International Harmonization (ICH) guidelines, the tenets of the Declaration of Helsinki, and Good Clinical Practice (GCP). The study was also registered on clinicaltrials.gov (NCT05501795). Data are not available for sharing.
Subjects were included who were appropriate candidates for uncomplicated bilateral LASIK surgery, were adults (≥18 years old), had spherical equivalent refractive errors up to 0 to −6 D with maximum cylinder up to 3.00 D, had stable refractive error, and had pachymetry above 490 μm with residual stromal thickness greater than 270 μm. Subjects were excluded if they had usual relative and absolute contraindications for LASIK surgery (severe dry eye, recurrent corneal erosion, uncontrolled glaucoma, collagen vascular disorders, keratoconus or signs of keratoconus, uncontrolled diabetes, herpes).
The primary endpoint was the resultant thickness of the femtosecond laser created LASIK flap compared to the planned thickness at the surgical visit using pre- and post-flap pachymetry as measured using the WaveLight EX500 on-board pachymeter. Secondary endpoints included the resultant diameter of the femtosecond laser created LASIK flap compared to planned diameter, and preoperative pachymetry measured with the on-board optical pachymeter of the excimer laser (WaveLight EX500) on the day of surgery compared to preoperative pachymetry measured with the Pentacam (Oculus) up to 2 months prior to surgery. Preoperative pachymetry was taken with both the on-board optical pachymeter of the EX500 laser and the Pentacam. Post-flap lift pachymetry was taken with only the on-board optical pachymeter of the EX500 laser. Achieved flap thickness was calculated using a subtraction technique, where flap thickness is equal to the difference in pachymetry before flap lift to pachymetry after flap lift. The resultant flap diameter was determined using digital analysis, as described by Kanellopoulos and Asimellis.12 In brief, a single image containing the applanation cone and flap diameter for each eye was imported into software (Illustrator 2023, Adobe); then, the diameters of each were determined (in pixels) by a masked evaluator (masked to the intended diameter of each eye) using the built-in measurement tool of the software. Finally, using the known cone diameter of 13.4 mm, the flap diameter was calculated as 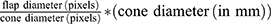 . An additional exploratory objective of the study was to determine if there was a correlation between the measured full corneal thickness and the actual achieved flap thickness.
. An additional exploratory objective of the study was to determine if there was a correlation between the measured full corneal thickness and the actual achieved flap thickness.
For LASIK surgical planning, preoperative tomography was performed using the Pentacam, and topography was performed using the Vario topographer (Alcon Vision, LLC). LASIK surgeries were performed by an experienced surgeon (SW) using his preferred standard of care. Flap diameter was chosen based on the preoperative white to white measurement. All flaps were planned for a thickness of 120 microns. Flaps were created using the WaveLight FS200 femtosecond laser (Alcon Vision, LLC). Stromal ablation was done using the WaveLight EX500 excimer laser (Alcon Vision, LLC).
It was estimated that the study would require a sample size of at least 49 patients (98 eyes) to achieve a power of 90% and a level of significance of 5% (two sided), for detecting a mean of the differences of 5 μm between planned and achieved flap thickness and assuming the standard deviation of the differences to be 15 μm.
All statistical analyses were performed using the software program R (version 4.2.2; The R Foundation for Statistical Computing, Vienna, Austria). A paired t-test was used to compare differences between parametric data, and a p-value ≤ 0.05 was considered significant.
Results
A total of 58 subjects (116 eyes) were enrolled and completed the study. The preoperative and patient demographics are shown in Table 1. There were no adverse events reported during the study.
 |
Table 1 Preoperative and Demographic Data |
Table 2 and Figure 1 show the distribution of flap thicknesses achieved, calculated using the EX500 on-board pachymeter before and after flap lift. All flaps were targeted for 120 μm. Mean achieved thickness was 120.64 ± 9.0 μm (range 102 to 143 μm; 95% confidence interval 108 and 133 μm). The mean directional difference in achieved minus intended flap thickness was 0.64 ± 9.0 μm (range −18 to 23 μm). This difference was not statistically significant (p > 0.05). The mean absolute difference between achieved and intended flap thickness was 7.02 ± 5.63 μm (range 0 to 23 μm).
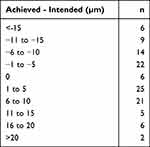 |
Table 2 Thickness Differences |
 |
Figure 1 Density plot of achieved flap thicknesses, calculated using the WaveLight EX500 on-board pachymeter before and after flap lift. The red dashed line represents the mean. |
Table 3 summarizes the intended flap diameters in this study. Figure 2 shows the overall correlation between achieved and intended flap diameter. The mean directional difference in achieved minus intended flap diameter was 0.02 ± 0.05 mm (range −0.1 to 0.1 mm). This difference was statistically significant (p < 0.001), but not clinically relevant. The mean absolute difference between achieved and intended flap thickness was 0.03 ± 0.05 mm (range 0.0 to 0.1 mm). Pearson’s correlation coefficient was 0.82 between achieved and intended.
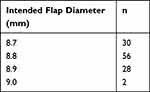 |
Table 3 Intended Flap Diameters |
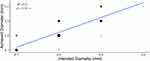 |
Figure 2 Overall correlation between achieved and intended flap diameter. The linear fit regression line is shown in blue. Point size is proportional to the number of overlapping points. |
Mean preoperative pachymetry with the Pentacam was 553.1 ± 29.4 μm (range 498 to 631 μm) compared to 555.2 ± 30.9 μm (range 500 to 639 μm) for the on-board optical pachymeter of the EX500. The mean of the difference was −2.1 ± 5.8 μm and was statistically significant (p < 0.001), but not clinically relevant. In addition, preoperative corneal thickness, as measured by Pentacam or EX500, was not correlated to the achieved flap thickness (p > 0.05, R2 = 0.008; and p > 0.05, R2 =−0.007, respectively).
Discussion
In LASIK procedures, the flap must be created in a safe and predictable manner to achieve good clinical outcomes. This includes creating the flap close to both the intended thickness and intended diameter. Surgeons need to be able to trust that the achieved flap parameters will be the same as the intended flap parameters. To the best of our knowledge, this is the first prospective study of flap thickness created with the FS200 and measured using the on-board pachymeter of the EX500.
The results of this study suggest that the FS200 can create flaps accurate to the intended thickness. Mean achieved thickness was 120.64 ± 9.0 μm. This is similar to that reported by Cummings et al,6 who observed a mean achieved flap thickness of 120.23 ± 13.94 μm in a retrospective analysis, using the on-board pachymeter of the EX500 to measure flap thickness. Mifflin et al11 reported a mean difference between intended and achieved flap thickness of 9 μm, in another retrospective analysis using the on-board pachymeter of the EX500, compared to 0.64 μm in our study. Other studies have also reported that the FS200 can accurately create flaps of the intended thickness using other methods to measure flap thickness including HF-UBM,7 OCT,8,9 and ultrasonic pachymetry.10 Use of the on-board pachymeter intraoperatively may offer advantages over a handheld pachymeter, such as noncontact (reducing the risk of bacterial contamination of the stromal bed) and shorter time between creation of the flap and stromal ablation.13
The range of achieved flap thicknesses in our study was 102 to 143 μm. Possible explanations for the discrepancies between target and achieved thicknesses include normal variation in actual flap thickness outcomes, variation in preoperative pachymeter measurements, and variation in post flap-lift pachymeter measurements. Cummings et al6 also targeted 120 μm flap thickness and reported a larger range (73 to 176 μm).
The results of this study also suggest that the FS200 can create flaps accurate to the intended diameter. All achieved diameters were within 0.1 mm of the intended diameter. In addition, the standard deviation was relatively small (± 0.05 mm), and the Pearson’s correlation coefficient was 0.82 between achieved and intended. We determined flap diameter using the digital analysis methodology reported by Kanellopoulos and Asimellis.12 In their study, the authors reported similar results, with standard deviations ranging from ± 0.04 to ± 0.06 mm. However, Kanellopoulos and Asimellis12 reported higher Pearson’s correlation coefficients of 0.96 and 0.997. This disparity may be explained by subjective differences between examiners when conducting the digital analysis. Moshirfar et al14 used a different digital analysis technique and reported higher standard deviations with the FS200 flap diameters compared to our study (± 0.13 to ± 0.20 mm). These disparities may again be explained by the subjective differences between examiners when conducting the digital analysis and by the differences in digital analysis techniques.
In this study, we also used the Pentacam preoperatively to measure full corneal thickness up to 2 months before surgery and compared that to the measurement with the on-board pachymeter of the EX500 immediately prior to creating the flap. This would allow assessment of any corneal thickness changes occurring in the months prior to surgery versus the day of surgery. Our results indicated that there was no clinical difference between these 2 methods of measurement and that both are reliable for surgical planning.
When flaps are created using a microkeratome, preoperative full corneal thickness may influence achieved flap thickness.15,16 To assess if this is also true in femtosecond laser flaps, a regression analysis was conducted to compare preoperative full corneal thickness to the actual achieved flap thickness. We observed no correlation, suggesting that the achieved flap thickness is not affected by the preoperative corneal thickness.
A limitation of this study was the subjectivity in the digital analysis used to measure flap diameter. The examiner uses their own judgement for the measurement tool, which could introduce bias. An objective measurement without human judgement may be more robust. However, the digital analysis method may be more accurate than other measurement techniques, such as a standard caliper.17
In conclusion, the overall results of this study suggest that the WaveLight FS200 laser is reliable for LASIK flap thickness and diameter and accurately created flaps at the intended thickness and the intended diameter.
Acknowledgement
This paper was presented at the 2023 American Society of Cataract and Refractive Surgery (ASCRS) Annual Meeting as a conference talk with interim findings.
Funding
This study was supported with an investigator-initiated study grant (73058121) from Alcon Vision LLC, Fort Worth, TX, USA.
Disclosure
Stephen Wexler reports consulting fees from Alcon. Brad Hall reports that he has received consulting fees from Ace Vision Group outside of the submitted work.
References
1. Durairaj VD, Balentine J, Kouyoumdjian G., et al. The predictability of corneal flap thickness and tissue laser ablation in laser in situ keratomileusis. Ophthalmology. 2000;107(12):2140–2143. doi:10.1016/S0161-6420(00)00407-3
2. Koch DD. The riddle of iatrogenic keratectasia. J Cataract Refract Surg. 1999;25(4):453–454. doi:10.1016/S0886-3350(99)80027-3
3. Vaddavalli PK, Yoo SH. Femtosecond laser in-situ keratomileusis flap configurations. Curr Opin Ophthalmol. 2011;22(4):245–250. doi:10.1097/ICU.0b013e3283479ebd
4. Denoyer A, Landman E, Trinh L, Faure JF, Auclin F, Baudouin C. Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology. 2015;122(4):669–676. doi:10.1016/j.ophtha.2014.10.004
5. Zhou Y, Zhang J, Tian L, Zhai C. Comparison of the Ziemer FEMTO LDV femtosecond laser and moria M2 mechanical microkeratome. J Refract Surg. 2012;28(3):189–194. doi:10.3928/1081597X-20120208-01
6. Cummings AB, Cummings BK, Kelly GE. Predictability of corneal flap thickness in laser in situ keratomileusis using a 200 kHz femtosecond laser. J Cataract Refract Surg. 2013;39(3):378–385. doi:10.1016/j.jcrs.2012.10.041
7. Kanellopoulos AJ, Asimellis G. Three-dimensional LASIK flap thickness variability: topographic central, paracentral and peripheral assessment, in flaps created by a mechanical microkeratome (M2) and two different femtosecond lasers (FS60 and FS200). Clin Ophthalmol. 2013;7:675–683. doi:10.2147/OPTH.S40762
8. Parafita-Fernandez A, Garcia-Gonzalez M, Gros-Otero J, Alvarez-Rementeria Capelo L, Blazquez Sanchez V, Teus M. Evolution of visual acuity, flap thickness, and optical density after laser in situ keratomileusis performed with a femtosecond laser. J Cataract Refract Surg. 2020;46(2):260–266. doi:10.1097/j.jcrs.0000000000000008
9. Zheng Y, Zhou Y, Zhang J, Liu Q, Zhai C, Wang Y. Comparison of laser in situ keratomileusis flaps created by 2 femtosecond lasers. Cornea. 2015;34(3):328–333. doi:10.1097/ICO.0000000000000361
10. Zhang J, Zhang SS, Yu Q, Wu JX, Lian JC. Comparison of corneal flap thickness using a FS200 femtosecond laser and a moria SBK microkeratome. Int J Ophthalmol. 2014;7(2):273–277. doi:10.3980/j.issn.2222-3959.2014.02.14
11. Mifflin MD, Mortensen XM, Betts BS, Gross C, Zaugg B. Accuracy of Alcon WaveLight((R)) EX500 optical pachymetry during LASIK. Clin Ophthalmol. 2017;11:1513–1517. doi:10.2147/OPTH.S138459
12. Kanellopoulos J, Asimellis G. Digital analysis of flap parameter accuracy and objective assessment of opaque bubble layer in femtosecond laser-assisted LASIK: a novel technique. Clin Ophthalmol. 2013;343. doi:10.2147/OPTH.S39644
13. Mifflin MD, Mortensen XM. Intraoperative optical pachymetry in photorefractive keratectomy. J Cataract Refract Surg. 2019;45(4):495–500. doi:10.1016/j.jcrs.2018.11.033
14. Moshirfar M, Brown TW, Heiland MB, Rosen DB, Ronquillo YC, Hoopes PC. Comparative analysis of LASIK flap diameter and its centration using two different femtosecond lasers. Med Hypothesis Discov Innov Ophthalmol. 2019;8(3):241–249.
15. Yildirim R, Aras C, Ozdamar A, Bahcecioglu H, Ozkan S. Reproducibility of corneal flap thickness in laser in situ keratomileusis using the Hansatome microkeratome. J Cataract Refract Surg. 2000;26(12):1729–1732. doi:10.1016/S0886-3350(00)00639-8
16. Giledi O, Mulhern MG, Espinosa M, Kerr A, Daya SM. Reproducibility of LASIK flap thickness using the Hansatome microkeratome. J Cataract Refract Surg. 2004;30(5):1031–1037. doi:10.1016/j.jcrs.2003.09.070
17. Pietila J, Huhtala A, Makinen P, Uusitalo H. Laser in situ keratomileusis enhancements with the Ziemer FEMTO LDV femtosecond laser following previous LASIK treatments. Graefes Arch Clin Exp Ophthalmol. 2013;251(2):597–602. doi:10.1007/s00417-012-2110-9
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
