Back to Journals » Clinical and Experimental Gastroenterology » Volume 11
Systemic inflammatory response syndrome and model for end-stage liver disease score accurately predict the in-hospital mortality of black African patients with decompensated cirrhosis at initial hospitalization: a retrospective cohort study
Authors Mahassadi AK , Konang Nguieguia JL, Kissi HY , Afum-Adjei Awuah A , Bangoura AD, Doffou SA , Attia AK
Received 28 April 2017
Accepted for publication 6 December 2017
Published 9 April 2018 Volume 2018:11 Pages 143—152
DOI https://doi.org/10.2147/CEG.S140655
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Andreas M. Kaiser
Alassan Kouamé Mahassadi,1 Justine Laure Konang Nguieguia,1 Henriette Ya Kissi,1 Anthony Afum-Adjei Awuah,2 Aboubacar Demba Bangoura,1 Stanislas Adjeka Doffou,1 Alain Koffi Attia1
1Medicine and Hepatogastroenterology Unit, Centre Hospitalier et Universitaire de Yopougon, Abidjan, Côte d’Ivoire; 2Kumasi Centre for Collaborative Research in Tropical Medicine, Kumasi, Ghana
Background: Systemic inflammatory response syndrome (SIRS) and model for end-stage liver disease (MELD) predict short-term mortality in patients with cirrhosis. Prediction of mortality at initial hospitalization is unknown in black African patients with decompensated cirrhosis.
Aim: This study aimed to look at the role of MELD score and SIRS as the predictors of morbidity and mortality at initial hospitalization.
Patients and methods: In this retrospective cohort study, we enrolled 159 patients with cirrhosis (median age: 49 years, 70.4% males). The role of Child–Pugh–Turcotte (CPT) score, MELD score, and SIRS on mortality was determined by the Kaplan–Meier method, and the prognosis factors were assessed with Cox regression model.
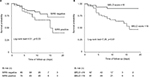
Results: At initial hospitalization, 74.2%, 20.1%, and 37.7% of the patients with cirrhosis showed the presence of ascites, hepatorenal syndrome, and esophageal varices, respectively. During the in-hospital follow-up, 40 (25.2%) patients died. The overall incidence of mortality was found to be 3.1 [95% confidence interval (CI): 2.2–4.1] per 100 person-days. Survival probabilities were found to be high in case of patients who were SIRS negative (log-rank test= 4.51, p=0.03) and in case of patients with MELD score ≤16 (log-rank test=7.26, p=0.01) compared to the patients who were SIRS positive and those with MELD score >16. Only SIRS (hazard ratio (HR)=3.02, [95% CI: 1.4–7.4], p=0.01) and MELD score >16 (HR=2.2, [95% CI: 1.1–4.3], p=0.02) were independent predictors of mortality in multivariate analysis except CPT, which was not relevant in our study. Patients with MELD score >16 experienced hepatorenal syndrome (p=0.002) and encephalopathy (p=0.001) more frequently than that of patients with MELD score ≤16. SIRS was not useful in predicting complications.
Conclusion: MELD score and SIRS can be used as tools for the prediction of mortality in black African patients with decompensated cirrhosis.
Keywords: MELD, SIRS, cirrhosis, mortality, Africa
Introduction
Cirrhosis is a major public health concern which can lead to the death of an individual; its 1-year mortality rate is estimated to be between 3% and 57% during follow-up.1,2 Tissue injury, inflammation, and infections are common complications found in patients with cirrhosis leading to systemic inflammatory response syndrome (SIRS) and death.1–3
To date, various tools have been validated in predicting mortality in patients with cirrhosis mainly in Western and Asian countries.4 In addition to the Child–Pugh–Turcotte (CPT) score, the score of model for end-stage liver disease (MELD) has been assessed as the predictor of survival in case of patients undergoing transjugular portosystemic shunt in the treatment of portal hypertension-related complications.5,6 Furthermore, MELD score has significantly contributed to lower the waiting list mortality prior to liver transplantation by allowing physicians to select patients with decompensated cirrhosis for graft allocation.7
Several studies have demonstrated that SIRS and MELD scores predict the in-hospital mortality accurately in patients with decompensated cirrhosis.8–13 Although patients with cirrhosis may experience recurrent hospitalization when decompensation occurs,14 little is known about the accuracy of SIRS and MELD score in predicting the in-hospital mortality of patients with cirrhosis at initial hospitalization.14
In sub-Saharan Africa, the mortality rate due to cirrhosis is 12 deaths per 100,000 people and is related to the burden of hepatitis B (HBV) and C viruses (HCV). 15–17 More than 55% of patients with cirrhosis are admitted to hospital at the end stage of the disease;18 the delay in hospitalization is mostly related to the cultural beliefs, traditional medicinal practice, poverty, limited medical facilities, and long distance transport to the hospital.19,20 Therefore, in Africa, the in-hospital mortality rate is found to be high at initial hospitalization.21,22 Thus, initial hospitalization can be considered as the cornerstone to implement the measures of resuscitation in patients with decompensated cirrhosis.
Therefore, in this study, we aimed to use SIRS and MELD score to predict in-hospital mortality among black African patients with decompensated cirrhosis at initial hospitalization.
Patients and methods
Patients
This retrospective cohort study was conducted in the Hepatology and Gastroenterology Unit of the Centre Hospitalier et Universitaire de Yopougon, Abidjan (Côte d’Ivoire, West Africa). All medical records of patients admitted from January 2012 to December 2015 were retrieved for the study.
In this study, only black African patients with cirrhosis, not <18 years old, admitted to the unit for the first time, regardless of the reason for admission, were included. Patients admitted to the unit due to the following reasons were excluded from this study: patients with acute hepatitis, chronic hepatitis (viral, alcoholic, or toxic) without cirrhosis, fulminant hepatitis, hepatic schistosomiasis, liver abscess, hepatocellular carcinoma, hepatic metastasis, hepatic disorders related to heart, renal failure, malaria, and hepatic steatosis. In addition to this, those who have had <1 day of stay in the Hepatology and Gastroenterology Unit or referred from another hospital were also excluded. This study was conducted with strict adherence to Good Clinical Practice.23
Methods
Only baseline parameters at initial hospitalization were retrieved including age, sex, temperature, heart rate, respiratory rate, complete blood cell count, prothrombin time or international normalized ratio (INR), urea, serum creatinine, bilirubin, phosphatase alkaline, gammaglutammyl transpeptidase, alanine aminotransferase (ALT), aspartate aminotransferase (AST), natremia, kalemia, ascitic fluid polymorphonuclear (PMN) cells, esophageal varices (EVs), etiology of cirrhosis, and the duration of hospital stay.
Definitions of parameters
The diagnosis of cirrhosis was performed by the mean of clinical and radiological examination showing liver dysmorphy, portal hypertension or ascites, and tests associated with liver function abnormalities (low level of platelet count, albumin, prothrombin time, and elevation of transaminases). In patients with normal or slight abnormalities of liver function tests without radiological signs of cirrhosis, the presence of gastroesophageal varices was suggestive of cirrhosis.1,24
SIRS is defined as two or more of the following variables:25
- fever of >38°C
- heart rate of >90 beats per minute
- respiratory rate of >20 breaths per minute
- white blood cell count of >12000 cells/µL or <4000 cells/μL
MELD score was determined using the previously reported formula:7 3.78 × loge bilirubin (mg/dL) + 11.2 × loge INR + 9.57 × loge serum creatinine (mg/dL) + 6.43.
MELD-Na score formula is defined as MELD+1.59(135-Na).26 To avoid the negative values of MELD-Na, we set all minimal (<120 Meq/L) and maximal values (up to 135 Meq/L) of natremia to 130 and 135 Meq/L, respectively.26
CPT score was assessed using clinical (encephalopathy and ascites) and biological parameters (prothrombin time or INR, bilirubin, and albumin) and according to the scoring process as follows: class A—total score between 5 and 6, class B—total score between 7 and 9, and class C—total score between 10 and15.1
EVs were classified by a semiquantitative and morphological method into three sizes:24
- Small varices (grade A) are EVs minimally elevated above the mucosal surface of the esophagus.
- Medium varices (grade B) are tortuous EVs occupying less than one-third of the lumen of the esophagus.
- Large varices (grade C) are tortuous and confluent EVs occupying more than one-third of the lumen of the esophagus.
Spontaneous bacterial peritonitis is defined as the ascitic PMN cell count of >250 cells/µL.27 Hepatorenal syndrome is defined as the serum creatinine level >1.5 mg/dL or creatinine clearance of <40 mL/min in patients with cirrhosis with ascites without any cause of kidney failure.27,28
Pulmonary and urinary infections or bedsores were defined as the presence of organ injury with clinical or radiological (pulmonary or urinary infections) assessment and fever or elevation of white blood cells or ascitic PMN cells and, if possible, with the evidence of bacteria or fungi in fluid smears.29,30
Hyponatremia and anemia are defined, respectively, as natremia <130 Meq/L and hemoglobin level <10 g/dL.31,32 Dilutional hyponatremia was defined as natremia <130 Meq/L at baseline without any diuretic treatment before hospitalization in patients with ascites.31
Patient management at first hospitalization and follow-up
All patients admitted due to cirrhosis in the Gastroenterology Unit after interrogation and physical examination underwent perfusion of isotonic fluid after venipuncture for blood sample collection. An initial workup was performed comprising complete blood cell count, liver function test, and assessment of serological markers of HBV and HCV, and assessment of Delta hepatitis virus if necessary. Patients with tense ascites underwent paracentesis with a perfusion of artificial colloid solution (Gelatin, Geloplasma®, 500 mL per 2 L fluid evacuated), and ascitic fluid samples were collected for biochemical, bacteriological, and cytological examinations. All patients were then referred for an endoscopy of the upper digestive tract to assess gastroesophageal varices and for an abdominal ultrasound examination for an assessment of radiological signs of liver cirrhosis.1 Patients remained in the hospital until the completion of all medical workup and patients needing urgent care were treated for their complications as follows:
Patients with encephalopathy were treated with lactulose by oral administration or by enema.1,27
In case of variceal bleeding, patients underwent blood transfusion, if necessary, with perfusion of metronidazole (250 mg) and amoxicillin (1 g) twice a day, and patients who were able to purchase the ligation kit, underwent EV band ligation. The others received an intravariceal injection of polidecanol if their bleeding persisted. All of them were treated with propranolol at a starting dose of 40 mg, which was gradually increased to 160 mg if necessary.24
Spontaneous bacterial peritonitis was treated with intravenous injection of cefotaxime (2 g once daily for 5 days) or received an oral administration of norfloxacin at a dosage of 400 mg twice daily for 5 days.26
Patients with hepatorenal syndrome underwent perfusion with artificial colloid solution as previously mentioned with correction of electrolyte imbalance. No vasoactive drugs were used.27,28
Outcome measures
In this study, the primary outcome was death due to any cause occurring in hospital at initial hospitalization. The secondary outcome was the diagnostic accuracy of SIRS and MELD score in the prediction of cirrhosis-related complications.
Ethical consideration
This study was approved by the Direction Médicale et Scientifique du Centre Hospitalier et Universitaire de Yopougon. The collection of informed consent from the subjects was not deemed necessary as the data was retrieved anonymously and retrospectively.
Statistical analysis
Categorical variables were expressed by number and percentage, and continuous variables were expressed by median and range. Mortality rate was calculated as the ratio of the number of deaths divided by the total number of patients at the time of follow-up.33 Two groups of patients were compared (alive and deceased) at initial hospitalization. Continuous variables were compared using a Student’s t-test if the data was normally distributed; otherwise, the data was compared using Mann–Whitney U test. Categorical variables were compared with the chi-square test or with the Fischer’s exact test if appropriate. Survival probabilities were assessed by Kaplan–Meier method and were compared with the log-rank test.34 The date of origin was the date of first admission in the Hepatology and Gastroenterology Unit, and the date of discharge was the date of point. Patients were censored if they were alive at the date of discharge. Cox proportional hazard model was used in the multivariate analysis of variables that were included in the initial model. This included all variables with p<20% in univariate analysis, except those entering in the definition of SIRS, MELD score or CPT score because of the risk of colinearity.34,35 The diagnostic accuracies of MELD and CPT scores were determined by analyzing the area under the receiver operating characteristic (AUROC) curves and compared with the method of Nelson and Allen and by using a macro program described by Mandrekar and Mandrekar.36,37 Cutoff values that maximized sensitivity and specificity were identified for the calculation of sensitivity, specificity, and positive predictive and negative predictive values (PPV and NPV). Furthermore, MELD score and SIRS were used in parallel and in serial testing.38 All statistical analysis were performed with SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) and SAS version 9.2 (SAS Inc., Cary, NC, USA) software with a two-sided significance level set at p<0.05.
Results
Patient characteristics at baseline
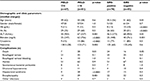
Among 317 patients hospitalized, during the study period, 159 patients (median age: 49 years old, 70.4% males) having cirrhosis were included in this study. Patients excluded were those having hepatocellular carcinoma (n=64), liver metastasis (n=2), liver abscess (n=8), acute viral or toxic hepatitis (n=4), liver schistosomiasis (n=1), upper digestive tract diseases (n=10), diabetes and arterial hypertension (n=9), HIV/AIDS (n=2), discharge at the day of entry (n=14), and incomplete data (n=44). Table 1 presents the baseline characteristics. Among those included, 83% had advanced liver disease (CPT class B=56.6% and class C=26.4%), 49.1% had a MELD score ≤16, and 74 (46.5%) patients met SIRS criteria (second criteria: n=58, third criteria: n=13, and fourth criteria: n=4).
The frequencies of combination of SIRS components were temperature >38°C and heart rate >90 beats per minute (n=25), temperature >38°C and respiratory rate >20 breaths per minute (n=11), temperature >38°C and white blood cells >14000 or <4000/µL (n=11), heart rate >90 beats per minute and respiratory rate >20 breaths per minute (n=36), heart rate >90 beats per minute and white blood cells >14000 or <4000/µL (n=43), and respiratory rate >90 breaths per minute and white blood cells >14000 or <4000/µL (n=26).
The reasons of hospital admission were as follows: edema and ascites (42.1%), digestive tract hemorrhage (14.5%), hepatic encephalopathy (10.7%), and jaundice (5.7%). In addition, 74.2% and 20.1% of the patients had ascites and hepatorenal syndrome, respectively. EV were present in 60 (37.7%) patients with cirrhosis, and of them, 20 (33.3%) had EV bleeding. The primary etiology of cirrhosis was HBV (86.8%) and HCV (5.7%).
Mortality ratios
During a follow-up of 1283 person-days in hospital, 40 (25.2%) patients died. Deceased patients had high MELD score (15 vs 20.8, p=0. 001) and were more SIRS positive (42 vs 60%, p=0.03) than those patients who were alive (Table 1). The overall mortality rate was found to be 3.1 (95% CI: 2.2–4.1) per 100 person-days. Survival probabilities in hospital were found to be high in SIRS-negative patients (log-rank test=4.51, p=0.03) and MELD score ≤16 (log-rank test=7.26, p=0.01) compared to SIRS-positive patients and patients with MELD score >16 (Figure 1). The mortality rates were found to be 1.87 (95% CI: 1.12–2.61) per 100 person-days for SIRS-positive patients and 2.18 (95% CI: 1.37–3.0) per 100 person-days for patients with MELD score>16.
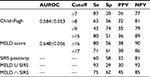
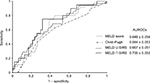
Predictive factors of mortality
In univariate analysis, only ascitic PMN cells were significantly associated with mortality. However, combining with other components of SIRS, SIRS and MELD score were found to be significantly associated with mortality. Multivariate analysis with forced variables showed that SIRS (HR=3.02, [95% CI: 1.4–7.4], p=0.01) and MELD score >16 (HR=2.2, [95%CI: 1.1–4.3], p=0.02) were independent predictive factors of mortality (Table 2). Table 3 shows diagnostic accuracies of SIRS, MELD, and CPT scores in the prediction of mortality. The comparison of AUROC between MELD score and CPT score did not show any significant difference in the prediction of death during hospitalization (0.649 vs 0.634, p=ns). However, with a cutoff of >16, MELD score had a sensitivity of 80% and an NPV of 90% in predicting mortality. With SIRS, the sensitivity and NPV were 60% and 81%, respectively, that were quite similar to that of CPT score at a cutoff of >8 (Table 3). In parallel testing, SIRS and MELD score showed a high sensitivity of 93% and an NPV of 92% for the prediction of mortality (Table 3). Pairwise comparisons did not show any significant difference between AUROC curves (Figure 2).
Baseline characteristics according to SIRS and MELD score
Although serum creatinine and bilirubin levels were high in patients with cirrhosis with MELD >16, we found that patients in this group had hyponatremia (p=0.002) and elevation of ALT compared to those with MELD≤16 (Table 4). In contrast, SIRS-positive patients with cirrhosis were younger (45.5 vs 51 years old, p=0.01) and anemic (Hb level: 8 vs 10 g/dL; p<0.0001) compared to SIRS-negative patients with cirrhosis who were older and had more deteriorated liver function test such as elevation of ALT (46.5 vs 68 IU/L, p=0.01) and bilirubin levels (25 vs 40 mg/L, p=0.001).
Distribution of complications according to SIRS and MELD score
In addition to the prediction of mortality, patients with MELD score >16 experienced greater complications of hepatorenal syndrome (p=0.002) and encephalopathy (p=0.001) than those patients with MELD ≤16. No prediction of complications other than mortality was found with SIRS (Table 4).
Discussion
The primary finding of this study was the ability and accuracy of SIRS and MELD score to predict the in-hospital mortality in black African patients with decompensated cirrhosis at initial hospitalization. Furthermore, patients with MELD score >16 experienced greater complications of hepatorenal syndrome and hepatic encephalopathy.
We have previously demonstrated the ability and accuracy of MELD score in predicting long-term survival in black African patients with cirrhosis.18 However, we have no data for short-term survival in our practice. MELD score and SIRS in patients with cirrhosis are good predictors of short-term survival (<3 months) in Western and Asian patients with cirrhosis8–11 and in our study, even though patients with cirrhosis were enrolled at initial hospitalization. Our study demonstrated that SIRS and MELD score were robust in predicting in-hospital mortality in black African patients with cirrhosis, irrespective of the timing of follow-up, and this was in accordance with previous studies.8–13
The impairment of liver function involves cell injury due to infectious and noninfectious diseases, and a disturbance in the liver metabolism leads to SIRS and mortality.1,9,12,25 In addition to the in-hospital mortality, Cazzaniga et al have also demonstrated that patients with SIRS experienced greater complications of hepatorenal syndrome and hepatic encephalopathy than those without.9 We did not confirm this finding in our study in which SIRS identified only patients at risk of death at initial hospitalization but not those with other complications of cirrhosis as reported by previous authors.8–10 Univariate analysis in our study showed that the level of ascitic PMN cells, one of the component variables of SIRS, was found to be significantly different between patients who are alive compared to those who died, suggesting that infection is a key factor of mortality. In addition, SIRS-positive patients with cirrhosis were found to be younger with anemia (hemoglobin level <10 g/dL) due to bleeding related to portal hypertension or profound impairment of liver function.32 Among 60 patients with EV, 20 had variceal bleeding and 48 patients with cirrhosis were CPT class C. Surprisingly, SIRS-negative patients with cirrhosis were older with slightly higher level of ALT, which might be related to the increased severity in chronic viral hepatitis.39 These patients may experience acute-on-chronic liver failure.40 Thus, they do not develop SIRS when they get an infection because of their compromised immunity.40,41
Moreover, hepatorenal syndrome is the major cause of mortality in patients with cirrhosis.1,2,4 In their large prospective multicenter study, Thabut et al demonstrated that SIRS and MELD score were predictors of mortality in patients with cirrhosis with acute functional renal failure, including hepatorenal syndrome and functional renal failure related to ongoing infections.42 It was not surprising to find out in our study that only patients with cirrhosis with an elevated MELD score (MELD score >16) experienced hepatorenal syndrome as serum creatinine is a component of MELD score.7 However, our study contradicts the results of Thabut et al.42 In this study, SIRS was not relevant in predicting hepatorenal syndrome. This discrepancy could be related to the study design (prospective versus retrospective study in ours) or a selection bias, as we did not use all criteria related to SIRS definition such as partial arterial carbon dioxide pressure.25,33 Furthermore, patients with MELD score >16 had slight hyponatremia in accordance with the findings of Ruf et al.26 Hyponatremia correlates with the level of MELD score and increases the risk of death in patients with cirrhosis.26 However, in our study, we did not find any significant effect of MELD-Na on the outcome. MELD score encompasses hepatic and renal impairments reflecting on prothrombin time and serum creatinine levels.7 Renal impairment is related to renal artery vasoconstriction in patients with cirrhosis, mostly due to splanchnic vasodilatation leading to the intra-abdominal fluid collection and sodium retention that worsens liver function.27,28
CPT score did not appear to have a significant effect on in-hospital mortality, in the final adjusted model, on multivariate analysis. Most patients enrolled were in CPT score class B or C. CPT score is less accurate and may lead to misclassification of patients, as it incorporates two clinical signs.1 In the study by Angermayr et al, CPT was less sensitive in differentiating the survival rate among patients with cirrhosis with CPT score class A or B.6 However, we found that CPT score >8 had a high PPV for in-hospital mortality. In this study, the prediction accuracy of CPT score was not different in comparison with MELD score, which was also reported by other researchers and our team and similar to that of SIRS.6,18 However, the accuracy of CPT score was quite low (AUROC =0.584±0.053), which suggests a biased classification33 or emphasizes the use of other prognostic tools in combination with CPT score to enhance the prediction of mortality in patients with cirrhosis in our practice.
Our study demonstrated that SIRS and MELD score in parallel testing reached high accuracy in identifying black African patients with cirrhosis who are at risk of mortality with high sensitivity and NPV >90%. In addition, the elevated value of MELD score suggested hepatorenal syndrome, which is a life-threatening condition in patients with cirrhosis.28,42 Moreover, SIRS and MELD score are easily obtainable parameters in clinical practice. In Africa, most of the patients consume traditional and herbal medicine that has a well-known deleterious effect on hepatic and renal function before hospital admission.43 MELD score and SIRS could be used as short-term survival predictors at initial hospitalization for cirrhotic decompensation in addition to CPT score.
This study has some limitations. First, it was a retrospective cohort study including only patients who underwent clinical and radiological assessment of cirrhosis at initial hospitalization. This study did not take into account those who have had recurrent hospitalization. Second, SIRS was not accurate in our study to classify patients with cirrhosis with infectious complications as previously reported by Cazzaniga et al, probably related to a classification bias.9,33 Finally, we could not say with high certainty that renal failure at initial hospitalization was related only to cirrhosis decompensation, as before seeking modern treatment, black African patients often use herbal medicine because of their traditional beliefs, which is potentially harmful to renal and hepatic function.19,43
However, this study has some advantages by the epidemiological profile of black African patients with cirrhosis similar to those found in other African countries.15,20 Our study demonstrated the relevant accuracy of MELD score and SIRS in the prediction of in-hospital mortality of black African patients with decompensated cirrhosis as reported in Western and Asian patients.8–13
Finally, our study suggests that MELD score and SIRS can be used as tools in the prediction of mortality (MELD score and SIRS) and the implementation of adequate measures of resuscitation in our practice.
Disclosure
The authors report no conflicts of interest in this work.
References
Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008;371(9615):838–851. | ||
Planas R, Montoliu S, Ballesté B, et al. Natural history of patients hospitalized for management of cirrhotic ascites. Clin Gastroenterol Hepatol. 2006;4(11):1385–1394. | ||
Tandon P, Garcia-Tsao G. Bacterial infection, sepsis and multiorgan failure in cirrhosis. Semin Liver Dis. 2008;28(1):26–42. | ||
D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis. A systematic review of 118 studies. J Hepatol. 2006;44(1):217–231. | ||
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatol. 2000;31(4):864–871. | ||
Angermayr B, Cejna M, Karnel F, et al. Child-Pugh versus MELD score in predicting survival in patients undergoing transjugular intrahepatic portosytemic shunt. Gut. 2003;52(6):879–885. | ||
Kamath PS, Kim RW; Advanced Liver Disease Study Group. The model for end-stage liver disease (MELD). Hepatology. 2007;45(3):797–805. | ||
Botta F, Giannini E, Romagnoli P, et al. MELD scoring system is useful for predicting prognosis in patient with liver cirrhosis and it correlated with residual liver function: a European study. Gut. 2003;52(1):134–139. | ||
Cazzaniga M, Dionigi E, Gobbo G, Fioretti A, Monti V, Salerno F. The systemic inflammatory response syndrome in cirrhotic patients: relationship with their in-hospital outcome. J Hepatol. 2009;51(3):475–482 | ||
Jeong JH, Park IS, Kim DH, et al. CLIF–SOFA score and SIRS are independent prognostic factors in patients with hepatic encephalopathy due to alcoholic liver cirrhosis. Medicine (Baltimore). 2016;95(26):e3935. | ||
Peng Y, Qi X, Guo X. Child-Pugh versus MELD score for the assessment of prognosis in liver cirrhosis. Medicine (Baltimore). 2016;95(8):e2877. | ||
Behroozian R, Bayazidchi M, Rasooli J. Systemic inflammatory response syndrome and MELD score in hospital outcome of patients with liver cirrhosis. Middle East J Dig Dis.2012;4(3):168–172. | ||
Abdel-Khalek EE, El-Fakhry A, Helaly M, Hamed M, Elbaz O. Systemic inflammatory response syndrome in patients with liver cirrhosis. Arab J Gastroenterol. 2011;12(4):173–177. | ||
Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital re-admissions among patients with decompensated cirrhoisis. Am J Gastroenterol. 2012;107(2):247–252. | ||
Mokdad AA, Lopez AD, Shahraz S, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145. | ||
Mendy ME, Welzel T, Lesi OA, et al. Hepatitis B, viral load and risk for liver cirrhosis and hepatocellular carcinoma in the Gambia, West Africa. J Viral Hepat. 2010;17(2):115–122. | ||
Messina JP, Humphreys I, Flaxman A, et al. Global distribution and prevalence of hepatitis C virus genotypes. Hepatology. 2015;61(1):77–87. | ||
Attia KA, Ackoundou-N’guessan KC, Ndri-Yoman AT, et al. Child-Pugh-Turcott versus Meld score for predicting survival in a retrospective cohort of black African cirrhotic patients. World J Gastroenterol. 2008;14(2):286–291. | ||
Chukwuneke FN, Ezeonu CT, Onyire BN, Ezeonu PO. Culture and biomedical care in Africa: the influence of culture on biomedical care in a traditional African society. Niger J Med. 2012;21(3):331–333. | ||
Etyang AO, Munge K, Bunyasi EW, et al. Burden of disease in adults admitted to hospital in a rural region of coastal Kenya: an analysis of data from linked clinical and demographic surveillance systems. Lancet Glob Health. 2014;2(4):e216–e224. | ||
Le S, Spelman T, Chong CP, et al. Could adherence to quality of care indicators for hospitalized patients with cirrhosis-related ascites improve clinical outcomes? Am J Gastroenterol. 2016;111(1):87–92. | ||
Myer L, Smith E, Mayosi BM. Medical inpatient mortality at Groote Schuur hospital, Cape Town, 2002-2009. S Afr Med J. 2013;103(1):28–35. | ||
Vijayananthan A, Nawawi O. The importance of good clinical practice guidelines and its role in clinical trials. Biomed Imaging Interv J. 2008;4(1):e5. | ||
Garcia-Tsao G, Sanyal AJ, Grace ND, Carey WD; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Am J Gastroenterol. 2007;102(12):2086–2102. | ||
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–1655. | ||
Ruf AE, Kremers WK, Chavez LL, Descalzi VI, Podesta LG, Villamil FG. Addition of serum sodium into MELD score predicts waiting list mortality better than MELD alone. Liver Transpl. 2005;11(3):336–343. | ||
European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53(3):397–417. | ||
Ginès P, Schrier RW. Renal failure in cirrhosis. N Engl J Med. 2009;361(13):1279–1290. | ||
Gupta D, Agarwal R, Aggarwal NA, et al. Guidelines for the diagnosis and management of community and hospital acquired pneumonia in adults: joint ICS/NCCP(I) recommendations. Lung India. 2012;29(Suppl 2):S27–S62. | ||
Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of America. Clin Infect Dis. 2016;59(2):e10–e52. | ||
Ginès P, Guevara M. Hyponatremia in cirrhosis: pathogenesis, clinical significance, and management. Hepatol. 2008;48(3):1002–1010. | ||
Gonzales-Casas R, Jones EA, Moreno-Otero R. Spectrum of anemia associated with chronic liver disease. World J Gastroenterol. 2009;15(37):4653–4658. | ||
Bonita R, Beaglehole R, Kjellström T. Basic Epidemiology. 2nd ed. Geneva: World Health Organization; 2006. | ||
Lee ET, Wang J. Statistical Methods for Survival Data Analysis. 2nd ed. Vol. 476. New York: John Wiley & Sons; 2003. | ||
Dormann CF, Elith J, Bacher S, et al. Colinearity: a review of methods to deal with it and a simulation study evaluating their performance. Ecography. 2012;36(1):27–46. | ||
Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148(3):839–843. | ||
Mandrekar JN, Mandrekar SJ. Statistical methods in diagnostic medicine using SAS® software. In: Proceedings of the 30th SAS Users Group International Conference (SUGI); April 10–13; 2005;. Philadelphia, PA. | ||
Zhou XH, McClish DK, Obuchowski NA. Statistical Methods in Diagnostic Medicine. New York: John Wiley & Sons; 2002. | ||
McMahon BJ. The natural history of chronic hepatitis B virus infection. Semin Liv Dis. 2004;24(Suppl 1):17–21. | ||
Arroyo V, Moreau R, Jalan R, Ginès P; EASL-CLIF Consortium CANONIC Study. Acute on chronic liver failure: a new syndrome that will re-classify cirrhosis. J Hepatol. 2015;62(1 Suppl):S131–S143. | ||
Rolando N, Wade J, Davalos M, Wendon J, Philpott-Howard J, Williams R. The systemic inflammatory response syndrome in acute liver failure. Hepatology. 2000;32(4 Pt 1):734–739. | ||
Thabut D, Massard J, Gangloff A, et al. Model for end stage liver disease and systemic inflammatory response are major prognostic factors in patients with cirrhosis and acute functional renal failure. Hepatology. 2007;46(6):1872–1882. | ||
Kamsu-Foguem B, Foguem C. Adverse drug reactions in some African herbal medicine: literature review and stakeholders interview. Integr Med Res. 2014;3(3):126–132. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.