Back to Journals » Patient Preference and Adherence » Volume 17
Systematic Evaluation and Nursing Outlook of Clinical Characteristics of 60 Twin Pregnancies with Complete Hydatidiform Mole and a Coexistent Viable Foetus
Authors Yang J, Shi Z, Jia S, Liu J, Jiang L, Zhu Y
Received 30 June 2023
Accepted for publication 14 October 2023
Published 27 October 2023 Volume 2023:17 Pages 2631—2640
DOI https://doi.org/10.2147/PPA.S428330
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Jing Yang,1,* Zhan Shi,1,* Shafeng Jia,1,* Jia Liu,2,* Ling Jiang,2 Yueqin Zhu2
1Department of Obstetrics, Suzhou Municipal Hospital, the Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou, People’s Republic of China; 2Department of Nursing Department, Gusu School, Nanjing Medical University, the Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shafeng Jia, Department of Obstetrics, Suzhou Municipal Hospital, the Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou, 215002, People’s Republic of China, Tel +86-0512-62362039, Email [email protected] Jia Liu, Department of Nursing department, Gusu School, Nanjing Medical University, the Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou, 215002, People’s Republic of China, No. 26, Daoqian Street, Email [email protected]
Objective: To analyse the clinical data of and provide a reference for the care and perinatal health care of twin pregnancy patients with complete hydatidiform mole and a coexistent foetus (CHM & CF).
Methods: We searched the China National Knowledge Infrastructure (CNKI) and Wanfang and VIP databases to comprehensively collect clinical studies on the “clinical characteristics of complete hydatidiform mole and coexisting foetal twin pregnancy”. Patients’ data were extracted from the literature, and 60 patients were divided into Group A (live newborns not delivered, 47) and Group B (live newborns delivered, 13). The clinical characteristics of the two groups were compared to explore the pregnancy outcomes and influencing factors of persistent gestational trophoblastic disease (pGTD) in patients with CHM & CF.
Results: The gestational week of diagnosis (Odd Ratio (OR)=0.203, 95% Confidence Interval (CI)=0.055– 0.753) and number of complications (OR=0.328, 95% CI=0.135– 0.793) were found to be independent influencing factors of pregnancy outcomes in patients with CHM & CF (p < 0.05). Ovulation induction therapy (OR=2.333, 95% CI=0.561– 9.708), preeclampsia (OR=75.000, 95% CI=11.041– 509.486) and the number of complications (OR=4.768, 95% CI=1.914– 11.875) were the independent influencing factors of developing pGTD (p < 0.05).
Conclusion: Pregnancy should not be terminated immediately after the early detection of CHM & CF, and multiple factors should be considered. Preeclampsia may indicate a poor prognosis, and ovulation induction may increase the incidence of pGTD. Targeted nursing and psychological nursing should be carried out according to the clinical symptoms of the patients.
Keywords: twin pregnancy, complete hydatidiform mole and coexistent foetus, persistent gestational trophoblastic disease, clinical characteristics, nursing
Introduction
Hydatidiform mole in pregnancy is rare and includes complete hydatidiform moles (CHM) and partial hydatidiform moles (PHM). Most foetuses with PHM and pregnancy are triploid and often do not survive. CHM with pregnancy has one twin as hydatidiform mole and the other as a normal pregnancy, which is known as CHM and coexistent foetus (CHM & CF) in a twin pregnancy.1 A twin pregnancy with CHM & CF is a rare disease with an incidence of approximately 1/22,000–100,000.2,3 In recent years, with the application of ovulation induction drugs and the development of assisted reproductive technology, its incidence has increased.3 At present, most of them are case reports and small sample clinical reports in China, and the results differ.4–40 Patients with CHM & CF have a higher risk of spontaneous abortion, and about 40% of patients will have a live birth.41 This disease may cause foetal death, massive vaginal bleeding, severe preeclampsia, hyperthyroidism and even persistent gestational trophoblastic disease (pGTD). Further, clinical care is difficult and complex.4–13 To avoid adverse outcomes for pregnant women and infants, early termination of pregnancy is often recommended, which is not universally acceptable.42,43 In recent years, for patients with a strong desire to continue their pregnancy, clinicians tend to take conservative treatment using strict hospital monitoring and follow-ups.44,45 In current medical conditions, most complications can be diagnosed and treated early. Termination of pregnancy is considered in cases of preeclampsia, thyroid crisis and massive vaginal bleeding.46 Because the disease may progress to difficult-to-treat pGTD, clinical decision-making regarding whether to continue pregnancy is a challenge for obstetricians and gynecologists. This study provides a systematic evaluation of the domestic-reported CHM & CF case-related studies, and a statistical analysis was performed in combination with one case from Suzhou Municipal Hospital. It aims to explore the clinical characteristics, factors that may lead to CHM & CF and pGTD, and neonatal outcomes and care points and provide a reference for the prevention, care and perinatal health care of CHM & CF.
Data and Methods
Search Strategy
CNKI, Wanfang Database (WFDB) and VIP Database (WEIPU) were searched. The date range was from the database’s establishment (CNKI: June 1999; Wanfang: 1988; VIP: 2000) to October 2022, and all references of the included articles were traced. References of the included studies were searched for analysis. Clinical studies related to the ‘clinical characteristics of twin pregnancy with complete hydatidiform mole and coexistent foetus’ were comprehensively collected. The literature search strategy adopted the principle of combining subject words and free words. The search terms included the following: twin pregnancy, complete hydatidiform mole and coexistent foetus, persistent gestational trophoblast disease, clinical characteristics and clinical analysis.
Inclusion and Exclusion Criteria
Literature inclusion criteria: ① Related clinical study on clinical characteristics of CHM & CF; ② Clear clinical diagnosis of persistent gestational trophoblast disease; and ③ The “gold standard” for all studies was pathological histology or cytology biopsies.
Literature exclusion criteria: ① Digest, review, lectures, literature reviews, conference papers and dissertations; ② The relevant data cannot be extracted due to incorrect data or incomplete data; ③ There is no clear “gold standard”, or the case group is not confirmed by the “gold standard”; and ④ Repeated publication of the literature.
Data Extraction
Literature information was independently extracted by two investigators, including the study author, publication time, mean age and range, number of cases, diagnostic criteria, histological type, clinical stage, treatment method and prognostic survival. If there was a disagreement, this was discussed with a third investigator to resolve the differences.
The patients’ data were summarized, including their age, pregnancy time, number of induced abortions, conception mode, gestational week of diagnosis, gestational week of termination of pregnancy, clinical characteristics, patients’ willingness to continue pregnancy, pGTD, pregnancy outcome and clinical characteristics of living newborns (gestational week at birth, birth mass, Apgar score, follow-up results).13–38 Patients were divided into two groups based on whether the live newborn was delivered, namely Group A (not delivered, 47 cases) and Group B (delivered, 13 cases).
Quality Evaluation
Two researchers respectively evaluated the quality of the literature, including the following 10 items: ① Whether the number of cases was greater than 30 cases; ② Whether the diagnostic criteria were clear; ③ Whether the baseline characteristics data, such as patient source and average age, were clear; ④ Whether the histological type was clear; ⑤ Whether the clinical stage of the patients was clear; ⑥ Whether the clinical symptoms and data of the patients were complete; ⑦ Whether the treatment of the patients was clear; ⑧ Whether the prognosis and survival data of patients were detailed; ⑨ Whether the study limitations were described; and ⑩ Whether the clinical application value of the research results was elaborated. Each item was 1 point. The higher the score, the better the quality of the literature.
Statistical Analysis
The qualitative data in this study were evaluated using descriptive systematic evaluation methods. Quantitative data were processed using Review Manager and STATA 9.2 software. The extracted data were statistically analysed using SPSS 26.0 software. Measurement data meeting the normal distribution were expressed as the mean ± standard deviation ( ±s), and comparisons between groups were performed using the independent sample t-test. Count data were expressed as the number of cases and percentage (n, %), with χ2 test for the comparison between groups. If the minimum expected frequency in the row × column list was greater than 1 and less than 5, the continuous correction method was used, and p < 0.05 was considered a statistically significant difference. The binary logistic regression model was used for the multivariate analysis with the stepwise regression method. The test level was α =0.05, and p < 0.05 was considered statistically significant.
±s), and comparisons between groups were performed using the independent sample t-test. Count data were expressed as the number of cases and percentage (n, %), with χ2 test for the comparison between groups. If the minimum expected frequency in the row × column list was greater than 1 and less than 5, the continuous correction method was used, and p < 0.05 was considered a statistically significant difference. The binary logistic regression model was used for the multivariate analysis with the stepwise regression method. The test level was α =0.05, and p < 0.05 was considered statistically significant.
Results
Basic Characteristics of the Included Studies
Initially, 105 relevant articles were retrieved, the review articles and letters were excluded and 77 articles were selected, including 72 cases of CHM & CF. These documents were screened strictly according to the inclusion and exclusion criteria, excluding 13 cases of partial hydatidiform mole and coexistent foetuses. A total of 59 patients in 36 articles with CHM & CF met the criteria,5–40 and one patient was collected from Suzhou Municipal Hospital in July 2020, making a total of 60 patients. All included studies provided relatively complete data of clinical characteristics. The literature quality evaluation table of the included studies is shown in Table 1, and the literature search process is shown in Figure 1.
 |
Table 1 Quality Evaluation Form |
 |
Figure 1 Flow chart. |
Comparison of General Data Between the Two Groups
There were no significant differences in age, ovulation induction therapy, history of induced abortion, preeclampsia and pGTD between the two groups (p > 0.05). Willingness to continue the pregnancy cannot be compared. In Group A, the gestational week of diagnosis (14.95 ± 5.13 vs 22.53 ± 6.14), gestational week of termination of pregnancy (15.63 ± 4.41 vs 33.12 ± 3.67) and number of complications (1.81 ± 1.28 vs 2.03 ± 0.41) were all lower than those in Group B, with statistically significant differences (p < 0.05). Please see Table 2 for more details.
 |
Table 2 Comparison of Related Indicators Between the Two Groups |
Comparison of the Clinical Characteristics Between the Two Groups
In Group A, the top three most common clinical symptoms over the course of pregnancy were vaginal bleeding (43/47, 91.49%), preeclampsia (10/47, 21.28%) and lung metastasis (6/47, 12.77%). The top three most common clinical symptoms of Group B over the course of pregnancy were vaginal bleeding (11/13, 84.62%), lung metastasis (4/13, 30.77%) and preeclampsia (3/13, 23.08%). Please see Table 3 for more details.
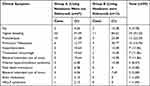 |
Table 3 Comparison of the Clinical Characteristics of the Two Patient Groups |
Analysis of Factors Influencing Pregnancy Outcomes in Patients with CHM & CF
A binary logistic regression analysis was performed with whether to deliver live infants at termination as the dependent variable and with statistically significant variables (gestational week of diagnosis, gestational week of termination of pregnancy and number of complications) in a univariate analysis as the independent variables. The results showed that the gestational week of diagnosis (OR=0.203, 95% CI=0.055–0.753) and number of complications (OR=0.328, 95% CI=0.135–0.793) were independent factors affecting pregnancy outcomes in patients with CHM & CF (p < 0.05). The later the gestational week of diagnosis and the larger the number of complications, the more likely the patient was to deliver a live newborn. Please see Table 4 for more details.
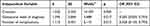 |
Table 4 Multivariate Correlation Analysis of Pregnancy Outcomes in Patients with CHM & CF |
Analysis of the Factors Affecting pGTD in Patients with CHM & CF
A binary logistic stepwise regression analysis was performed with pGTD as the dependent variable and age, ovulation-induction therapy, induced abortion history, number of complications and preeclampsia as the independent variables. The results showed that ovulation induction therapy (OR=2.333, 95% CI=0.561–9.708), preeclampsia (OR=75.000, 95% CI=11.041–509.486) and the number of complications (OR=4.768, 95% CI=1.914–11.875) were the independent influencing factors of pGTD (p < 0.05). Ovulation induction therapy, preeclampsia and an increased number of complications increased the risk of pGTD in patients with CHM & CF. Please see Table 5 for more details.
 |
Table 5 Multivariate Correlation Analysis of the Occurrence of pGTD in CHM & CF Patients |
Outcomes of Newborns Delivered by Pregnant Women in Group B
All the 13 pregnant women in Group B delivered live newborns, including five full-term newborns, eight non-term newborns and five newborns with low birth weight (according to the doctor’s diagnosis). The Apgar scores were all relatively good. The delivery modes were all caesarean sections. The half-year follow-up showed no abnormality (no subsequent reports). Please see Table 6 for more details.
 |
Table 6 Live Neonatal Outcomes in Group B |
Discussion
Pregnancy Outcomes of Patients with CHM & CF and Analysis of Factors Affecting the Occurrence of pGTD
This study analysed the related factors affecting pregnancy outcome and the occurrence of pGTD in patients with CHM & CF. The results showed that the independent factors (influencing factors independent of other factors) affecting pregnancy outcomes included the gestational week of diagnosis and number of complications in patients (p < 0.05), and the factors affecting pGTD in patients with CHM & CF included ovulation induction therapy, concurrent preeclampsia symptoms and number of complications (p < 0.05). Compared with Group B (delivered living newborns), the gestational week of diagnosis and gestation week of termination of pregnancy in Group A (did not deliver living newborns) were earlier than Group B, which may be related to the early detection of such cases and the recommendation of termination of pregnancy. Zhu Honglan and others studied 34 patients with CHM & CF and found that ovulation induction may be a high-risk factor for developing CHM & CF and pGTD.3 This study found that ovulation induction was not an independent influencing factor for CHM & CF but rather for pGTD. This may be related to the fact that ovulation induction treatment usually causes ovarian superovulation and increases the probability of empty eggs.47 The study by Sebire et al showed that there was no obvious relationship between the incidence of pGTD and the increase of gestational weeks, meaning the pregnancy could not be terminated for the sole reason of preventing the risk of pGTD.48
Care of Patients with CHM & CF
Targeted nursing:31,35 The incidence of such patients is very low, with complicated condition and many complications, and there is no fixed nursing routine. Based on the coexistence of complete hydatidiform mole and fetus in twin pregnancy, pregnant women should actively cooperate with doctors to develop relevant nursing plans. Based on a full understanding of CHM & CF, nursing staff should do a good job of monitoring patients’ comprehensive condition, carry out targeted nursing evaluations and make the corresponding nursing plans and measures. Moreover, attention should be paid to the results of ancillary examinations and their dynamic changes, with emphasis on the dynamic changes of serum HCG values. Preeclampsia has an impact on pregnancy outcomes and pGTD, and the development of preeclampsia indicates a poor prognosis, while severe preeclampsia indicates an increased risk of developing pGTD and should focus on preeclampsia signs such as edema, proteinuria and hypertension.
Psychological nursing:24,27 Patients with CHM & CF are faced with the important problem of whether to continue pregnancy after being diagnosed. Nurses should help patients to correctly understand CHM & CF and evaluate the risk of continuing pregnancy. In addition, patients may have negative emotions such as anxiety, fear, and pessimism due to concerns about delivery, family, and other issues. Nursing staff should find out the negative emotions of the patients in time; fully communicate with the patient’s spouse, family members and their relatives and friends; encourage their family members to visit and accompany the patients; and give them more spiritual and emotional care to improve their quality of life.
Perinatal nursing:33,34 CHM & CF is a high-risk pregnancy, and perinatal health care for such patients is crucial.4 Ovulation induction may be a high-risk factor for CHM & CF and pGTD, which should be valued in the high-risk scores for prenatal examination. In addition, attention should be paid to the postpartum follow-up of patients with CHM & CF regarding registration and monitoring. Wee et al49 suggested that patients should have routine blood and thyroid function tests every month, chest X-ray examination every 3 months to exclude metastasis, a close follow-up of blood β -HCG levels until they are normal and follow-ups for 2 years.
There are several limitations in this paper. Due to the uneven methodological quality of the studies included in this systematic evaluation, there are differences in the number of cases, evaluation methods and data statements among the studies. The above conclusions need to be confirmed by more large sample clinical studies.
Conclusion
Early detection should not result in the pregnancy being immediately terminated, and multiple factors should be considered. Preeclampsia may indicate a poor prognosis, and ovulation induction may increase the incidence of pGTD. Targeted nursing and psychological nursing should be carried out according to the clinical symptoms of patients.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The project was supported by the Correlation between psychological stress at different stages of IVF-ET pregnancy and maternal and infant outcomes: a prospective cohort study (GSKY20220402).Funding agencies did not play a role in study design, data collection, analysis and interpretation, and manuscript writing.
Disclosure
Jing Yang and Zhan Shi are co-first authors for this study. Shafeng Jia and Jia Liu are co-correspondence authors for this study. All of the authors had no any personal, financial, commercial, or academic conflicts of interest separately for this work.
References
1. Xiaoqing W, Guiqin M. Complete hydatidiform twin gestation coexisting with fetus term live birth in one case [J]. Family Planning Obstetrics Gynecol China. 2021;13(04):92–94.
2. Niemann I, Sunde L, Petersen LK. Evaluation of the risk of persistent trophoblastic disease after twin pregnancy with diploid hydatidiform mole and coexisting normal fetus. Am J Obstet Gynecol. 2007;197(1):45. e1–5. doi:10.1016/j.ajog.2007.02.038
3. Massardier J, Golfier F, Journet D, et al. Twin pregnancy with complete hydatidiform mole and coexistent fetus obstetrical and oncological outcomes in a series of 14 cases. Eur J Obstet Gynecol Reprod Biol. 2009;143(2):84–87. doi:10.1016/j.ejogrb.2008.12.006
4. Honglan Z. Outcomes of complete hydatidiform mole and a coexistent viable fetus: status in China. Chine J Clin Obstetrics Gynecol. 2015;16(6):523–527.
5. Haojie H, Yang X, Xirun W, et al. Diagnosis and management of respiratory failure secondary to twin pregnancies complicated by a coexisting molar pregnancy metastasizing to the lung. Progress Obstetrics Gynecol. 2006;15:545–546.
6. Baoyan L, Jinqiu S, Min D, et al. A case of one of a twin pregnancy consisting of a complete hydatidiform mole after in vitro fertilization-embryo transfer. Chine J General Practitioners. 2013;12:314–315.
7. Weiwei T, Tao S, Yan W. One case of a twin pregnancy consisting of a complete hydatidiform mole and coexisting fetus. Chine J Obstetrics Gynecol. 2003;38:632.
8. Fulan J, Zhirong L, Xueqiong Z, et al. A case of twin pregnancies complicated by Invasive Hydatidiform Mole metastasizing to the lung. Chine J Obstetrics Gynecol. 2003;38:775.
9. Lizi Z, Shilei B, Qiang S, et al. A case of a twin pregnancy consisting of a complete mole and coexisting fetus. J Dalian Med Univ. 2019;41:92–96.
10. Qingwei Q, Xiangyang HN, et al. Prenatal diagnosis and clinical management of a twin pregnancy consisting of a complete mole and coexisting fetus. Chine J Obstetrics Gynecol. 2003;38:595–598.
11. Min L, Benlian C, Hong Z, et al. one case of ultrasound findings of complete hydatidiform mole and coexisting fetus. Guizhou Med J. 2008;32:904–905.
12. Zubing S, Chen L, Wenying Z, et al. Hydatidiform mole coexisting with the fetus after in vitro fertilization-embryo transplantation in one case. Chine J Reproductive Health. 2007;18:41–42.
13. Bristow RE. One case of survival of one of the twin fetuses with complete hydatidiform mole. Progress Modern Obstetrics Gynecol. 2007;16:344.
14. Xiaoxia W, Ping T. One case of premature survival of twin pregnancy consisting of a complete hydatidiform mole. Chine J Perinatal Med. 2012;15:637–638.
15. Li L. One case of a hydatidiform mole with coexisting fetus diagnosed by ultrasound. Practical J Med Pharmacy. 2006;23:870.
16. Chunqu L, Rongcai X. A case report of a blebbing fetal mass combined with a normal fetus. J Nantong Med Univ. 1986;1:8.
17. Lei X, Yan D. One case of intrauterine pregnancy complicated with hydatidiform mole. Community doctors in China: medical Specialty. Int J Med. 2010;12:156.
18. Rui Z. A case report of double uterine simultaneous pregnancy with residual abortion and hydatidiform mole. Qinghai Med J. 2009;39:43.
19. Qingping J, Shaoyan L, Yuexin Y, et al. Hydatidiform mole with coexisting fetus: a clinicopathologic analysis of 4 cases. Chine J Clin Exp Pathol. 2013;29:850–854.
20. Lei W, Xiaoguang S. Comparison of a twin pregnancy consisting of a complete mole and its twin pregnancy after IVF. Chine J Birth Health Heredity. 2009;17:140–141.
21. Qun L, Xiujing S, Xiaoguang S. A twin pregnancy consisting of a complete mole after infertility treatment: two case reports.Special issue of the sixth National Reproductive Medicine Academic Conference of the Chinese Medical Association. Chine Med Assoc. 2012;46.
22. Tengzi R, Lishuang S, Huamei H, et al. Prenatal diagnosis and management of twin pregnancies complicated by a coexisting molar pregnancy. Chine J Prenatal Diagnosis. 2018;10:10–13.
23. Ding D, Ruijuan F, Suwen C, et al. A twin pregnancy consisting of a complete mole: 2 case report and literature review. Chine J Clinicians. 2015;43:84–85.
24. Shi L, Hui M, Tianfa D, et al. One case of a twin pregnancy consisting of a complete mole with lung metastasis. J Clin Radiol. 2018;37:1232–1235.
25. Ting G, Li L. Coexistence of fetus and hydatidiform placenta after in vitro fertilization-embryo transfer: a case report. Practical Preventive Med. 2009;16:177–179.
26. Lili D, Haiyan N, Cheng Y. Complete hydatidiform mole and fetus coexistence of live birth: a case report. J Clin Exp Pathol. 2018;34:816–819.
27. Qiaowen B, Xiaoli S, Xiping L. Complete hydatidiform mole and coexisting fetus: report of four cases and review of literatures. Chine J Practical Gynecol Obstetrics. 2017;33:955–958.
28. Fang F, Zhexuan G, Huihui L. A Case Report of Complete Hydatidiform Mole in Twin Pregnancy after IVF-ET. Int J Reproductive Health. 2019;38:296–300.
29. Shiyang J, Ping P, Xinyan L. Successful Labor Induction and Vaginal Delivery of Twin Pregnancy with Hydatidiform Mole and a Coexistent Fetus at 16 Weeks of Gestation:A Case Report. Med J Peking Union Med Coll Hospital. 2020;11:309–311.
30. Haixia C, Fang L. A case report of a twin pregnancy consisting of a complete mole and coexisting fetus. Qinghai Med J. 2016;46:62–65.
31. Tong Z, Yuanyuan W, Juncheng W, et al. Clinical analysis on hydatidiform mole with co-existent fetus. Progress Modern Obstetrics Gynecol. 2018;27:661–663.
32. Jinfeng T, Jianhong S, Hongwei S, et al. Analysis of clinical characteristics of 12 cases of multiple pregnancy with hydatidiform mole. Guangdong Med J. 2017;38:3613–3615.
33. Jin’e X, Xiuli J, Jianhua M, et al. A case of twin pregnancy with hydatidiform mole after multifetal pregnancy reduction. Guangdong Med J. 2002;23:241–243.
34. Huili Z, Bai Y, Shan L, et al. twin pregnancy with complete hydatidiform mole and coexisting fetus after IVF-ET. J Practical Obstetrics Gynecol. 2018;34:78–80.
35. Lei Z, Ping G, Qin M. One case of clinical care for coexistence of hydatidiform mole and fetus after IVF-ET. Qilu Nursing J. 2012;18:109–111.
36. Bristow RE. Twin pregnancy with the complete hydatidiform: a case report. Progress Modern Obstetrics Gynecol. 2017;26:879–881.
37. Deying W, Ming L, Lei Y. A case of twin pregnancy with hydatidiform mole after IVF-ET. Chine J Modern Med. 2008;18:2946.
38. Cuiping Y. Hydatidiform mole complicated with a normal fetus: a case report. J Shanxi Coll Traditional Chine Med. 2002;3:13–14.
39. Chuzhao J, Xuedie X, Qinghong S. One case of mature live infant with hydatidiform mole. Chine J Practical Gynecol Obstetrics. 2009;25:724.
40. Ping L, Qin G. A case of cytogenetic analysis of intrauterine pregnancy with complete hydatidiform mole. Nat Med J China. 2005;85:3096–3097.
41. Xiangyang ZJ. Progress in the diagnosis and treatment of gestational trophoblastic disease. Chine J Practical Gynecol Obstetrics. 2017;33(1):14–18.
42. Wax JR, Pinette MG, Chard R, Blackstone J, Cartin A. Prenatal diagnosis by DNA polymorphism analysis of complete mole with coexisting twin. Am J Obstet Gynecol. 2003;188(4):1105–1106. doi:10.1067/mob.2003.151
43. Sui JZ, Sun XF. Genetically identified complete hydatidiform mole coexisting with a normal fetus following IVF-ET. J Med Colleg of PLA. 2009;24(6):360–365. doi:10.1016/S1000-1948(10)60007-X
44. Shazly SA, Ali MK, Abdel Badee AY, et al. Twin pregnancy with complete hydatidiform mole and coexisting fetus following ovulation induction with a non - prescribed clomiphene citrate regimen: a case report. J Med Case Rep. 2012;6(1):95. doi:10.1186/1752-1947-6-95
45. Piura B, Rabinovich A, Hershkovitz R, Maor E, Mazor M. Twin pregnancy with a complete hydatidiform mole and surviving co-existent fetu. Arch Gynecol Obstet. 2008;278(4):377–382. doi:10.1007/s00404-008-0591-x
46. Kushtagi P, Hegde TN. Unusual twins: a case of intrauterine pregnancy with complete molar pregnancy. Int J Gynecol Obstet. 2009;10(2):11.
47. Honglan Z, Yi L. Meta-analysis of the clinical characteristics of complete hydatidiform mole coexisting with normal fetuses in 34 twin pregnancies [J]. Chine Clin J Obstetrics Gynecol. 2015;16(06):523–527. doi:10.13390/j.issn.1672-1861.2015.06.013
48. Sebire NJ, Foskett M, Paradinas FJ, et al. Outcome of twin pregnancies with complete hydatidiform mole and healthy co-twin. Lancet. 2002;359(9324):2165–2166. doi:10.1016/S0140-6736(02)09085-2
49. Wee L, Jauniaux E. Prenatal diagnosis and management of twin pregnancies complicated by a co-existing molar pregnancy. Prenat Diagn. 2005;25(9):772–776. doi:10.1002/pd.1272
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
