Back to Journals » Clinical Ophthalmology » Volume 18
Switching to Brimonidine/Ripasudil Fixed Combination from Brimonidine + Ripasudil
Authors Inoue K, Shiokawa M, Kunimatsu-Sanuki S, Tomita G , Ishida K
Received 27 October 2023
Accepted for publication 19 January 2024
Published 7 February 2024 Volume 2024:18 Pages 423—430
DOI https://doi.org/10.2147/OPTH.S446962
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Kenji Inoue,1 Minako Shiokawa,1 Shiho Kunimatsu-Sanuki,2 Goji Tomita,1,3 Kyoko Ishida3
1Inouye Eye Hospital, Tokyo, Japan; 2Nishikasai Inouye Eye Hospital, Tokyo, Japan; 3Department of Ophthalmology, Toho University Ohashi Medical Center, Tokyo, Japan
Correspondence: Kenji Inoue, Inouye Eye Hospital, 4-3 Kanda-surugadai, Chiyoda-ku, Tokyo, 101-0062, Japan, Tel +813-3295-0911 ; Fax +813-3295-0917, Email [email protected]
Purpose: A fixed-combination eye drop has several advantages over combination therapy, however, the intraocular pressure (IOP)-lowering efficacy and safety of the newly available brimonidine + ripasudil fixed-combination (BRFC) eye drops after switching from brimonidine + ripasudil is yet to be established. Therefore, this study aimed to retrospectively investigate the 6-month safety, usability, and IOP-lowering efficacy of BRFC switched from brimonidine and ripasudil.
Patients and Methods: Overall, 69 patients with primary open-angle glaucoma (69 eyes) receiving brimonidine + ripasudil were enrolled in this study. Brimonidine + ripasudil was discontinued, and treatment was switched to BRFC without a washout period. The IOP was compared before and at 3 and 6 months after switching to BRFC. The side effects, discontinued cases, and usability (a questionnaire survey) were also investigated.
Results: The IOP was not significantly different after switching to BRFC (15.1 ± 3.3 mmHg at baseline, 15.9 ± 3.6 mmHg after 3 months, and 14.6 ± 3.3 mmHg after 6 months). Adverse reactions occurred in four patients (5.8%): allergic conjunctivitis, two patients; irritation, one patient; and blurred vision, one patient. Treatment was discontinued in five (7.2%) patients owing to allergic conjunctivitis, two patients; increased IOP, two patients; and blurred vision, one patient. In the questionnaire survey, 68 patients with eye pain, 67 with itching, 64 with conjunctival hyperemia, 64 with irritation, and 62 with blurred vision reported no change or improved conditions. Additionally, in response to the question regarding preferences for pre-treatment and fixed combinations, 14 participants (20.2%) favored pre-treatment, while 53 (76.8%) preferred fixed combinations.
Conclusion: The IOP was maintained for 6 months, with satisfactory safety and comfort of use, with BRFC switched from brimonidine and ripasudil.
Keywords: adverse reactions, brimonidine/ripasudil, intraocular pressure, fixed combination, switching, usability
Introduction
A fixed-dose combination of latanoprost/timolol for the treatment of glaucoma became available in Japan in 1999. Combination eye drops are highly convenient, and thus, are used increasingly.1 By 2019, seven compounded eye drops became available, all containing β-blockers. Subsequently, brimonidine/brinzolamide without β-blockers was introduced in June 2020, and its indications were expanded to include patients with respiratory and cardiovascular diseases.2–4 The brimonidine + ripasudil fixed-combination (BRFC) eye drops containing brimonidine5 and ripasudil6,7 is the second type of fixed-combination eye drops without β-blockers. It has strong intraocular pressure (IOP)-lowering effects, high safety and has been available since December 2022. Moreover, clinical trials8 and studies9 on normal subjects conducted in Japan have reported favorable results regarding the efficacy and safety of BRFC eye drops.
The advantages of using a fixed-combination eye drop over combination therapy include a reduction in the number of bottles, frequency of eye drop use and improved adherence owing to a reduced incidence of adverse reactions.10 Nevertheless, these advantages are meaningless if the fixed-combination eye drops have inferior IOP-lowering effect. A previous study reported no change in the IOP and satisfactory safety and usability when brimonidine + brinzolamide was changed to brimonidine/brinzolamide fixed-combination eye drops.11 However, reports on the IOP-lowering efficacy and safety of the newly available BRFC eye drops after switching from brimonidine + ripasudil are scarce.
Therefore, this study aimed to retrospectively investigate the 6-month IOP-lowering efficacy, safety, and comfort of the BRFC eye drops after switching from brimonidine + ripasudil in patients with primary open-angle glaucoma (POAG).
Materials and Methods
This retrospective study included 69 patients with POAG (including normal-tension glaucoma (NTG)) who had been taking brimonidine + ripasudil for > 1 month at the Inouye Eye Hospital between December 2022 and February 2023. The patient inclusion and exclusion criteria are presented in Table 1. The medication was switched to BRFC eye drops without washout from the concomitant use of brimonidine (AIFAGAN®; Senju Pharmaceutical Co., Ltd., Osaka, Japan or brimonidine tartrate ophthalmic solution [SEC], Santen Pharmaceutical Co., Ltd., Osaka, Japan) and ripasudil (GLANATEC®; Kowa Company Ltd., Aichi, Japan). All other medications (Table 2) were continued. The IOP was determined using a Goldmann applanation tonometer before and at 3 and 6 months after switching to BRFC eye drops. Changes in IOP were classified into three groups: 1) a decrease by ≥ 2 mmHg; 2) a change of within 2 mmHg; and 3) an increase by ≥ 2 mmHg. At the first visit after switching to BRFC, an overview of the study was explained to eligible patients. Questionnaires were administered to patients regarding the use of fixed combinations and previous medications (Table 3). Additionally, we investigated the adverse reactions and immediately discontinued administration, as required, after switching to BRFC.
 |
Table 1 Patient Selection Criteria |
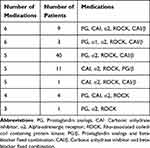 |
Table 2 Medications Before Switching to Brimonidine/Ripasudil Fixed Combination |
 |
Table 3 Questionnaire Survey of the Usability of Brimonidine/Ripasudil Fixed Combination |
POAG (Primary open-angle glaucoma) is a subtype of primary open-angle glaucoma (broad) in which IOP exceeds the statistically determined normal value during the developmental process of glaucomatous optic neuropathy, and an abnormal increase in IOP is strongly suspected to be involved in the development of optic neuropathy.12 NTG (Normal-tension glaucoma) is a subtype of primary open-angle glaucoma (broad) in which the IOP always remains within the statistically determined normal range during the developmental process of glaucomatous optic neuropathy.12
The IOP change was analyzed using ANOVA and Bonferroni/Dunn tests. The Wilcoxon signed-rank test was employed to compare and analyze the IOP reduction range and rate. The comparison and analysis of the IOP reduction range was performed using the χ2 test. The fixed-combination eye drops were treated as two separate medications in the analysis. Statistical analyses were conducted using IBM SPSS Statistics for Windows, version 22 (IBM Corp., Armonk, NY, USA). Differences were considered statistically significant at P < 0.05.
The study protocol was approved by the ethics committee of Inouye Eye Hospital (approval number: 202305–2). The signature on the questionnaires administered was considered as consent. Moreover, the need for written informed consent was waived by the committee due to the retrospective study design. Participants were provided with study information and given the opportunity to decline participation.
Results
The patients included 42 men and 27 women, with a mean age of 65.5 ± 11.2 years (range, 39–88 years). Among them, 62 had POAG, and seven had NTG. The medications used before the switch included AIfagan in 31 patients and Brimonidine Tartrate ophthalmic solution [SEC] in 37 patients, with one patient not providing this information. The average number of medications before switching was 5.0 ± 0.6 (range, 3–6) and details of the medications are presented in Table 2. Overall, 64 patients (92.8%) used prostaglandin/β fixed combinations or carbonic anhydrase inhibitor (CAI)/β fixed combinations. The IOP was evaluated in 69 patients before switching, 69 patients at 3 months after switching, and 65 patients at 6 months after switching. The mean IOP was as follows: 15.1 ± 3.3 mmHg before switching, 15.9 ± 3.6 mmHg at 3 months after switching, and 14.6 ± 3.3 mmHg at 6 months after switching, with no significant change from baseline (p=0.0531, analysis of variance, Figure 1). At 3 months after switching, IOP had decreased by ≥ 2 mmHg, changed within 2 mmHg, and increased by ≥ 2 mmHg from before switching in 13 (18.8%), 46 (66.7%), and 10 (14.5%) patients, respectively (Figure 2). At 6 months after switching, IOP had decreased by ≥ 2 mmHg, changed within 2 mmHg, and increased by ≥ 2 mmHg in 20 (30.8%), 34 (52.3%), and 11 (16.9%), respectively.
 |
Figure 1 IOP before and after switching to brimonidine/ripasudil fixed combination. |
 |
Figure 2 Changes in IOP after switching to brimonidine/ripasudil fixed combination. |
Adverse reactions occurred in four patients (5.8%) after switching, with two patients experiencing allergic conjunctivitis (after 6 months), one reporting irritation (after 4 months), and one describing blurred vision (after 4 months). Treatment was discontinued or additional treatment was administered in five patients (7.2%) due to allergic conjunctivitis (two patients, after 6 months), increased IOP (two patients, after 3 months), and blurred vision (one patient, after 4 months). One of the two patients with increased IOP was treated with selective laser trabeculoplasty, and the other returned to the previous medication. Additionally, there was one case of interrupted visits that occurred 4 months after switching.
In the questionnaire survey (Figure 3.), for Question 1–1 “Did you have conjunctival hyperemia after switching?” 22 out of 69 (31.9%) patients responded”, “less than before”, and 42 out of 69 (60.9%) responded “no difference”. For Question 1–2 “Did you have irritation after switching?” 46 out of 69(66.7%) responded “no difference”. For Question 1–3 “Did you have itching after switching?” 50 out of 69(72.5%) responded “no difference”. For Question 1–4 “Did you have pain after switching?” 56 out of 69 (81.2%) responded “no difference”. For Question 1–5 “Did you have blurring after switching?” 52 out of 69 (75.4%) responded “no difference”. For Question 2–1 “Do you prefer the eye drop before or after switching ? 53 out of 69 (76.8%) patients responded “after switching”. For Question 2–2 “The reason for patients who preferred the eye drop after switching”, 59 out of 69 (85.5%) responded, “better usability of container”.
 |
Figure 3 Results of the questionnaire survey. |
Discussion
In this study, we examined the IOP reduction, safety, and user comfort associated with BRFC over 6 months following the switch from brimonidine + ripasudil. The IOP-lowering effect was maintained with satisfactory safety and comfort during the 6 months. To our knowledge, there have been no such reports on drug switching in the past. In a Japanese clinical trial, patients taking brimonidine after at least 4 weeks were randomly categorized into the switched to BRFC (113 patients), continued brimonidine (113 patients), and brimonidine + ripasudil (56 patients) groups.8 Each group was treated for 8 weeks, and the IOP was compared 2 h after eye drop application at weeks 2, 4, 6, and 8 and 7 h after eye drop application at weeks 4 and 8. The IOPs in the BRFC and brimonidine + ripasudil groups were significantly lower at all time points than before the switch; however, the IOP-lowering effect was not significantly different between the two groups. Additionally, the IOP was not significantly different before and after switching from brimonidine + ripasudil to BRFC. This indicates that the IOP-lowering effect of BRFC is equivalent to that of brimonidine + ripasudil.
BRFC is a combination eye drop that does not contain β-blockers. We previously investigated the IOP-lowering efficacy and safety of brimonidine/brinzolamide combination eye drops after switching from brimonidine + brinzolamide in 102 patients.11 At 3 months after switching, the IOP had decreased by ≥ 2 mmHg in 15.8% patients, changed within 2 mmHg in 61.4% patients, and increased by ≥ 2 mmHg in 22.8% patients. At 6 months after switching, the IOP had decreased by ≥ 2 mmHg in 14.5% patients, changed within 2 mmHg in 69.8% patients, and increased by ≥ 2 mmHg in 15.6% patients. In the current study, the IOP at 3 months after switching had decreased by ≥ 2 mmHg in 13 (18.8%) patients, changed within 2 mmHg in 46 (66.7%) patients, and increased by ≥ 2 mmHg in 10 (14.5%) patients. Further, at 6 months after switching, the IOP had decreased by ≥ 2 mmHg in 20 (30.8%) patients, changed within 2 mmHg in 34 (52.3%) patients, and increased by ≥ 2 mmHg in 11 (16.9%) patients. Thus, the changes in IOP showed a similar trend to that of previous studies. Particularly, the IOP was not significantly different before and after treatment in all patients, although each patient responded differently and required careful follow-up after switching. In cases where IOP increased after drug switching, the interval between visits was narrowed to take account of IOP fluctuations.
For all 11 cases with increased IOP after 6 months of drug switching, there was subsequently one patient received additional drug treatment, one underwent selective laser trabeculoplasty and one surgery performed.
In a previous Japanese clinical trial,8 adverse reactions occurred in 57.5% of the patients in the BRFC group. These adverse events included conjunctival hyperemia (55.8%), eye irritation (5.3%), blepharitis (1.8%), conjunctival hemorrhage (1.8%), conjunctivitis (0.9%), abnormal sensations (0.9%), and arthralgia (0.9%). In contrast, 57.1% of the patients in the brimonidine/ripasudil group had adverse reactions. These events included conjunctival hyperemia (57.1%), eye irritation (8.9%), and conjunctivitis (5.4%). Similarly, in this study, adverse reactions occurred in four patients (5.8%): allergic conjunctivitis in two patients, irritation in one patient, and blurred vision in one patient. In the previous study, the frequency of adverse drug reactions was lower than that after switching to BRFC.8 The incidence of conjunctival hyperemia was also lower, partly due to the change between the same ingredients, brimonidine, and ripasudil. Additionally, side effects such as allergic conjunctivitis, irritation, and blurred vision were also reported.8 In this study, 7.2% of the cases of discontinuation were due to changes in the same ingredients.
Most patients reported no difference with respect to the changes in eye symptoms before and after switching. Further, the majority reported an improvement in each survey category, indicating that the effect of the new eye drops combination was mostly satisfactory. With respect to the preferred eye drops, the majority (53 patients, 76.8%) of the patients opted for BRFC. The most common reason for this was because it was easier to use a single bottle (fewer eye drops) (59, 85.5%) and it did not sting (6, 8.7%). We previously conducted a survey of other eye drop combinations when patients switched from two single-agents of the same ingredients to a combination of eye drops.13–15 Overall, 68.0% patients preferred tafluprost/timolol combination eye drops,13 82.1% preferred latanoprost/timolol combination eye drops,14 and 54.8% preferred travoprost/timolol combination eye drops.15 Their primary reason for preferring compounded eye drops was a reduction in the total number of eye drops required. Similarly, BRFC eye drops are also comfortable to use, which is expected to improve adherence. Nonetheless, this study had some limitations. The follow-up period was only 6 months; therefore, further long-term follow-up studies are required to validate our results. Moreover, the concomitant medications were not identical which may result in different effects. Therefore, it would be ideal to consider cases in which the only two-drug combination of brimonidine and ripasudil was changed to BRFC. However, in actual clinical practice, such cases are rare. Additionally, we also evaluated cases in which other eye drops were used concomitantly.
Conclusion
In patients with POAG, the IOP-lowering effect of switching from brimonidine + ripasudil eye drops to BRFC is maintained, and safety and comfort of use is satisfactory within 6 months.
Abbreviations
BRFC, brimonidine + ripasudil fixed-combination; IOP, intraocular pressure; POAG¸primary open-angle glaucoma; NTG, normal-tension glaucoma.
Data Sharing Statement
The participant data that support the findings of this study are available for 5 years after publication from the corresponding author, K.I., upon reasonable request.
Ethics Approval and Informed Consent
The study protocol was approved by the Ethics Committee of Inouye Eye Hospital and adhered to the principles of the Declaration of Helsinki. Study information was provided by the hospital, and participants had the opportunity to refuse to participate in the study.
Acknowledgments
We would like to thank Editage for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, including in the conception, study design, execution, acquisition of data, analysis and interpretation; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Disclosure
Kenji Inoue received lecture fees from Senju, Otsuka, Kowa, Santen, Allergan Japan, K.K., Novartis, HOYA, Pfizer Japan Inc., Viatris, Rohto Nitten, and Chugai. Minako Shiokawa received lectures from Otsuka. Shiho Kunimatsu-Sanuki has received lecture fees from Santen, Viatris, Otsuka, Kowa, Senju, Nitto Medic, Novartis, and Rohto. Kyoko Ishida received lecture fees from Santen, Senju, Otsuka, Kowa, Wakamoto, and Nitto Medicine. Goji Tomita received a grant from Senju and lecture fees from Kowa pharmaceutical, TOPCON, Viatris, and Nitto Medics. The authors report no other conflicts of interest in this work.
References
1. Inoue K, Komori R, Kunimatsu-Sanuki S, Ishida K, Tomita G. Frequency of use of fixed-combination eye drops by patients with glaucoma at multiple private practices in Japan. Clin Ophthalmol. 2022;16:557–565. doi:10.2147/OPTH.S345944
2. Onoe H, Hirooka K, Nagayama M, et al. The efficacy, safety, and satisfaction associated with switching from brinzolamide or brimonidine to brinzolamide/brimonidine in open-angle glaucoma patients. J Pers Med. 2022;12(12):2057. doi:10.3390/jpm12122057
3. Aoki R, Terao E, Dote S, et al. Efficacy and safety of a fixed combination of 1% brinzolamide and 0.1% brimonidine as treatment for glaucoma: a retrospective study focusing on the number of ingredients. BMJ Open Ophthalmol. 2022;7(1):e001200. doi:10.1136/bmjophth-2022-001200
4. Sharma S, Trikha S, Perera SA, Aung T. Clinical effectiveness of brinzolamide 1%-brimonidine 0.2% fixed combination for primary open-angle glaucoma and ocular hypertension. Clin Ophthalmol. 2015;9:2201–2207. doi:10.2147/OPTH.S72380
5. Krupin T, Liebmann JM, Greenfield DS, Ritch R, Gardiner S; Low-Pressure Glaucoma Study Group. A randomized trial of brimonidine versus timolol in preserving visual function: results from the low-pressure glaucoma treatment study. Am J Ophthalmol. 2011;151(4):671–681. doi:10.1016/j.ajo.2010.09.026
6. Tanihara H, Kakuda T, Sano T, Kanno T, Kurihara Y. Long-term intraocular pressure-lowering effects and adverse events of ripasudil in patients with glaucoma or ocular hypertension over 24 months. Adv Ther. 2022;39(4):1659–1677. doi:10.1007/s12325-021-02023-y
7. Sakamoto E, Ishida W, Sumi T, et al. Evaluation of offset of conjunctival hyperemia induced by a Rho-kinase inhibitor; 0.4% Ripasudil ophthalmic solution clinical trial. Sci Rep. 2019;9(1):3755. doi:10.1038/s41598-019-40255-9
8. Tanihara H, Yamamoto T, Aihara M, et al. Ripasudil–brimonidine fixed-dose combination vs ripasudil or brimonidine: two Phase 3 randomized clinical trials. Am J Ophthalmol. 2023;248:35–44. doi:10.1016/j.ajo.2022.11.017
9. Tanihara H, Yamamoto T, Aihara M, et al. Crossover randomized study of pharmacologic effects of ripasudil-brimonidine fixed-dose combination versus ripasudil or brimonidine. Adv Ther. 2023;40(8):3559–3573. doi:10.1007/s12325-023-02534-w
10. Djafari F, Lesk MR, Harasymowyczet J, Desjardins D, Lachaine J. Determinants of adherence to glaucoma medical therapy in a long-term patient population. J Glaucoma. 2009;18(3):238–243. doi:10.1097/IJG.0b013e3181815421
11. Inoue K, Kunimatsu-Sanuki S, Ishida K, Tomita G. Intraocular pressure-lowering effects and safety of brimonidine/brinzolamide fixed combination after switching from other medications. Jpn J Ophthalmol. 2022;66(5):440–446. doi:10.1007/s10384-022-00930-3
12. Kikuchi Y, Inoue T, Shoji N, Nakamura M, Tanito M. The Japan glaucoma society guidelines for glaucoma. Jpn J Ophthalmol. 2023;67(2):189–254. doi:10.1007/s10384-022-00970-9
13. Inoue K, Kawashima T, Katakura S, et al. Switching from concomitant therapy to tafluprost/timolol fixed combination. Clin Ophthalmol. 2018;12:549–554. doi:10.2147/OPTH.S150595
14. Inoue K, Okayama R, Higa R, Wakakura M, Tomita G. Assessment of ocular hypotensive effect and safety 12 months after changing from an unfixed combination to a latanoprost 0.005% + timolol maleate 0.5% fixed combination. Clin Ophthalmol. 2012;6:607–612. doi:10.2147/OPTH.S30611
15. Inoue K, Setogawa A, Higa R, Moriyama R, Wakakura M, Tomita G. Ocular hypotensive effect and safety of travoprost 0.004%/timolol maleate 0.5% fixed combination after change of treatment regimen from β-blockers and prostaglandin analogs. Clin Ophthalmol. 2012;6:231–235. doi:10.2147/OPTH.S29062
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
