Back to Journals » Risk Management and Healthcare Policy » Volume 16
Sustained Improvement of Appropriateness in Surgical Antimicrobial Prophylaxis with the Application of Quality Control Circle
Authors Zou J, Zhong JY, Liu YX, Liu Y, Huang D, Xu BT, Li XW, Gong WJ, Tao J
Received 22 November 2022
Accepted for publication 1 March 2023
Published 9 March 2023 Volume 2023:16 Pages 347—356
DOI https://doi.org/10.2147/RMHP.S398692
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Jian Zou,* Jia-Yun Zhong,* Yan-Xin Liu, Yu Liu, Dan Huang, Bian-Tiao Xu, Xi-Wen Li, Wen-Jun Gong, Jia Tao
Department of Clinical Pharmacy, The People’s Hospital of Pengzhou, Chengdu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jian Zou, The People’s Hospital of Pengzhou, No. 255 Second Section of South Third Ring Road, Chengdu, People’s Republic of China, Tel +86 28 86239898, Email [email protected]
Purpose: Quality control circle (QCC) has acquired success in many fields in healthcare industry as a process management tool, whereas its efficacy in surgical antimicrobial prophylaxis (SAP) remains unknown. This study aimed to implement QCC interventions to improve the appropriateness of SAP.
Methods: A QCC activity team was established to grasp the current situation of SAP in clean surgery procedure, set target, formulate corresponding countermeasures and implement and review them in stages. The plan-do-check-act (PDCA) method was cyclically applied.
Results: The appropriateness of antibiotic prophylaxis before (January to December 2020) and after (January to December 2021) the implementation of QCC activities were evaluated based on relevant international and Chinese SAP guidelines. The overall SAP appropriateness was significantly improved from 68.72% before QCC to 93.7% post QCC implementation (P< 0.01). A significant improvement (P< 0.05) was also determined for each category: selection (from 78.82% to 96.06%), duration (from 90.15% to 96.46%), indication (from 94.09% to 97.64%), timing of first dose (from 96.55% to 99.21%), antimicrobial usage (from 96.8% to 99.41%), re-dosing of antimicrobial (from 96.55% to 99.21%).
Conclusion: Implementation of a QCC program can optimize the use of antibiotics and improve the appropriateness of SAP and is of practical importance to their standardization.
Keywords: surgical antimicrobial prophylaxis, quality control circle, appropriateness
Introduction
Antimicrobial resistance (AMR) is a global threat to human health and well-being.1 AMR has generated an unprecedented amount of global attention, this increase in attention around AMR has coincided with a rise in focus on this topic at various multilateral organizations and international fora.2 Microorganisms resistance is the main causative element of hospital acquired infections (HAIs), of which surgical site infections (SSIs) are considered to be a major cause of morbidity and mortality related to HAIs.3 SSIs are one of the most common and severe clinical complications after surgeries, often causes prolonged hospitalization and delayed postoperative therapy, and substantially increase the health-care costs.4,5 Clean surgery is defined as uninfected operative wound, where no inflammation is encountered and the respiratory, alimentary, and genital of uninfected urinary track are not opened.6,7 Although the principles of surgical antimicrobial prophylaxis (SAP) are clearly established and relevant guidelines have been published.8,9 However, unnecessary or suboptimal prescriptions of antimicrobial prophylaxis is a common phenomenon worldwide, including excessive use of antibiotics, inappropriate selection or dosages, prolonged duration or incorrect timing of first dose, which may result in antibiotic resistance and higher healthcare costs.10
Quality control circle (QCC) is a process management and problem-solving technique founded in 1962 by Dr Kaoru Ishikawa of Japan, which is viewed as a powerful tool to solve the problems in work and improve the complex work flow by the joint efforts of all members composed of staff from the same or similar complementary workplaces.11 Until 2001, QCC activities was introduced to healthcare industry in China, and numerous studies have revealed that the application of QCC could effectively raise the quality of medical service and ensure the safety of patients.12–14 Despite the extensive application of QCC in healthcare industry, few studies have formally determined its association with SAP. In this study, a QCC program was carried out to optimize the use of antibiotics and improve the appropriateness of SAP.
Methods
Clinical Materials
A QCC program was launched in the People’s Hospital of Pengzhou, a tertiary hospital in Chengdu, China. Our study was approved by the ethical committee of the People’s Hospital of Pengzhou and the data was anonymized or maintained with confidentiality. This study complied with the tenets of the Declaration of Helsinki and was based on the standard for quality improvement reporting excellence (SQUIRE, version 2.0). Retrospective data of 1092 patients who had undergone clean surgical procedures from January to December 2020 at our hospital was included (before QCC). In addition, 1142 patients who underwent clean surgical procedures from January to December 2021 were regarded as the intervention group (after QCC).
Formation of QCC and Theme Selection
We carried out the activities strictly in accordance with four stages and 10 steps of QCC (as shown in Figure 1): identification of a problem, developing an action plan, status analysis of the problem, goal setting, cause effect analysis, generating solutions, implementation of solutions, result confirmation, standardization, and review. A total of 8 members QCC team was established, a pharmacist was appointed as leader, responsible for program management and outcomes, the circle members includes surgeon, clinical pharmacist, infectious diseases physician, nurse, anesthetist, clinical microbiologist and infection control practitioners.
 |
Figure 1 A flow diagram illustrating the ten QCC steps beside the PDCA workflow. |
Developing an Action Plan
Gantt chart was adopted to draw up the activities and duration of the separate steps of the implementation plan according to the processes and the theme of QCC, the person in charge of each step was confirmed.
Status Analysis and Goal Setting
A total of 1092 patients who underwent clean surgery from January to December 2020 were investigated, of which 406 patients received antimicrobial, while 686 patients did not. The appropriateness of SAP was assessed based on relevant national guidelines and Chinese national guidelines available at the time of assessment.8,9 The rate of the appropriate utilization of SAP was analyzed by a Pareto chart for improvement and a checklist for irrational prescriptions, the overall appropriate rate was 68.72%. According to the 80/20 rule, we determined the 3 major deficiencies, which were incorrect antibiotics selection, over-extended duration and no indication of prophylaxis, they accounted for 84.70% of the total defects, as shown in Figure 2. According to the formula of the target value,15 the target value =current value-(current value×value of focus×ability of circle) = 68.72%-(68.72%×84.7%×80%)=22.16%, the target value was to improve the appropriate rate of SAP by 22.16% so as to achieve the appropriate rate of SAP in 90.88%.
 |
Figure 2 The key problems of the inappropriate implementation of SAP in clean surgery that need to be improved. |
Cause Effect Analysis
Based on the current situation investigation, a brainstorming method was conducted by QCC members to analyze the cause of SAP inappropriateness from the perspectives of people, equipment, materials, management and environment, a Fishbone diagram was constructed (Figure 3). Subsequently, a questionnaire regarding the causes of inappropriateness in antimicrobial prophylaxis prescribing practices was conducted among antimicrobial prescribing surgeons of our hospital to assess hospital staff’s perceptions of SAP. According to the 80/20 principle, Pareto chart was adapted to demonstrate the essential causes of the SAP inappropriateness that need to be improved are fear of SSI, lack of professional training, inadequate supervision, lack of standardized process and insufficient assessment, as shown in Figure 4.
 |
Figure 3 Analysis of the root causes of inappropriate implementation of SAP in clean surgery by Fishbone diagram. |
 |
Figure 4 Pareto chart demonstrates the essential causes of the inappropriate administration of SAP in clean surgery that need to be improved. |
Solutions Generating and Implementation
According to the three key problems that can be solved, the final improvement strategies were implemented following brainstorming based on the comprehensive evaluation of the feasibility, autonomy and ability of QCC members. The leader of the QCC summarizes and evaluates the various methods, and then analyzes and modifies the methods through quality control tools. The specific methods are as follows:
Training and Education
We invited microbiologists and anti-infective specialists to interpret the guidelines related to SAP, and provided related knowledge training and regular management for surgeons. In addition, various forms of publicity and training were carried out among surgeons, nurses, standard-trained doctors and new physicians. Furthermore, a booklet documented the standard operating procedure of SAP for various clean procedures according to the established criteria was distributed to each surgeon.
Monitor and Intervention
Clinical pharmacists participate in the formulation of prescriptions and conduct a real-time supervision on the whole process of SAP by using a computerized system. Clinical pharmacist should remind the surgeons through the computerized hospital system to modify the prescription immediately when inappropriate antimicrobial prophylaxis were prescribed. If the opinions of pharmacist with surgeons are inconsistent, the pharmacist should consider the doctor’s appeal and suggestions, and check the rationality of the prescription again, revising the evaluation standard if necessary.
Evaluation and Reporting
Data on the characteristics of the surgical patients were collected from the hospital information system, the rationality of the SAP was evaluated by clinical pharmacists according to the established criteria. Clinical pharmacists summarized and analyzed the information of the use of antimicrobial prophylaxis, and reported to prescribers and hospital leadership every week. Furthermore, in view of some common problems of inappropriate application of SAP, hierarchical training were conducted by clinical pharmacists for key departments to elevate the professional knowledge of medical staff.
Effect Evaluation
The effects of QCC intervention were evaluated and other data were recorded, including the occurrence of SSIs, other surgical complications and antibiotic-associated side effects. Appropriate use of antibiotic prophylaxis in terms of correct indication, antibiotic choice, dose, timing of first dose, frequency and duration were determined after comparing with standard protocols as per evaluation criteria in the footnotes of Table 2.6,7,9 The differences of appropriate rate of SAP and the incidence of SSIs, other surgical complications and antibiotic-associated side effects before and after QCC intervention were compared.
Statistical Analysis
Data were represented as means ± SEM. Statistical analyses were performed by using the SPSS 20.0 software (SPSS Inc.; IL, USA). Statistical comparisons between two groups were conducted by using one-way analysis of variance (ANOVA) followed by Bonferroni post hoc test. Enumeration data were analyzed using the χ2-test. Difference between groups were considered statistically significant when a value of P<0.05.
Results
Tangible Results
The types of surgeries in pre- and post-QCC interventions are summarized in Table 1, there was no significant difference in types of surgeries between the two groups. As shown in Table 2, the overall appropriateness was significantly increased from 68.72% before QCC to 93.7% post QCC interventions (P<0.01), and a significant improvement was also promoted for each indicator: selection (from 78.82% to 96.06%), duration (from 90.15% to 96.46%), indication (from 94.09% to 97.64%), timing of first dose (from 96.55% to 99.21%), antimicrobial usage (from 96.8% to 99.41%), re-dosing of antimicrobial (from 96.55% to 99.21%), all the differences above were statistically significant (P<0.05). After the QCC intervention, the setting goal was achieved. Target reach rate = (improvement value−current value)/(target value−current value)×100%=(93.7%−68.72%) / (90.88%−68.72%) = 112.73%, progress rate = (improvement value−current value)/current value×100% = 36.35%. These results demonstrated that QCC interventions could significantly optimized the use of antibiotics and improved the appropriateness of SAP. Furthermore, we also compared the incidence of SSI, other surgical and antibiotic-related complications between the two groups. As shown in Table 3, there was no significant difference in SSI, other surgical and antibiotic-related complications in pre and post-QCC interventions.
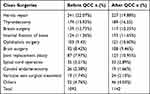 |
Table 1 Type of Surgical Procedures |
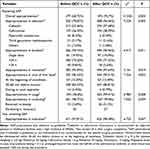 |
Table 2 SAP Appropriateness Before and After QCC Intervention |
 |
Table 3 Surgical and Antibiotic-Related Complications After Clean Surgery in Two Groups |
Intangible Results
A self-evaluation questionnaire concerning self-confidence, responsibility, team-work spirit and commitment, problem-solving capability, communication skills and skills of quality control of circle members were completed, with the highest score of 5 and the lowest score of 1 for each item. The result is plotted as a radar map. As shown in Figure 5, all aspects above mentioned of circle members were significantly improved after the QCC activities.
 |
Figure 5 Analysis of the circle capability by radar diagram. |
Standardization
After the continuous improvement of the QCC intervention, a standardized operation flow for the appropriate prescriptions of prophylactic antibiotics in clean incision operations was established.
Discussion
Statement of Principal Findings
Antimicrobial misuse and overuse play a key role in the emergence of AMR, creating an urgency to improve antimicrobial prescribing. In the current study, we retrospective evaluated the use of antimicrobial prophylaxis in patients who underwent clean surgery procedures, only 68.72% of antimicrobial prophylaxis were deemed to be appropriate. After the QCC interventions, the overall appropriateness of antimicrobial prophylaxis improved to 93.7%. In addition, the indication of antimicrobial prophylaxis, antibiotics selection and dosage, prophylaxis duration, timing of first dose and re-dosing of antibiotics were significantly optimized, suggested the effectiveness of QCC interventions.
Strengths and Limitations
There are several strengths and limitations in our study. Strengths include that QCC activity significantly improve the appropriateness of SAP. Moreover, QCC interventions effectively promote the surgeon’s perceptions of SAP and thereby improve the appropriateness of selection, duration, indication, timing of first dose, dosage and re-dosing of antimicrobial prophylaxis. Finally, QCC interventions could effectively promote the self-confidence, problem-solving capability and skills of quality control of medical staff, and deserved application in medical quality improvement activities.
However, several limitations of our study should be born in mind. This was a single-center study, relatively small number of observations, and inclusion of only those who underwent clean surgical procedures. In the future, we will expand the sample and make continuous quality improvements to more accurately reflect the sustainability of the QCC program to provide more clinically meaningful and valuable results.
Interpretation Within the Context of the Wider Literature
Antimicrobial misuse and overuse are leading causes in the emergence of antimicrobial-resistant bacteria.16 Although the availability of consensus guidelines for antimicrobial prophylaxis in surgery clearly demonstrated the SAP indication, antimicrobial selection, timing of first dose, antimicrobial usage, duration of prophylaxis and re-dosing of antimicrobial and all the parameters for clean surgical operations.9 However, significant discrepancies between clinical practice of SAP and the guidelines in clean surgical procedures were founded before QCC in our hospital. Previous studies reported that lack of sufficient and effective education among surgeons seems to be the main barrier to adherence with SAP guidelines,17 surgeons prescribe antimicrobial according to their own principle that they trained in a wrong way in the past and it was counterintuitive for them to accept the new clinical practice guidelines about SAP.17 Surgeons were accustomed to prescribe antimicrobial prophylaxis and prolonged use of antimicrobial in cases, as they falsely believed that maintaining antimicrobial in the bloodstream of a post-operative patient was an effective precaution against SSIs.18 Thus, testing the compliance and acceptance of clinical guidelines among surgeons is of great significance for their effective implementation.
One of the most crucial issues for appropriate SAP depending on possible contaminating bacteria and their susceptibility to antimicrobial, whether antimicrobial can reach an effective concentration at the surgical site.19 In accordance with the international and native guidelines, first- or second- generation cephalosporin was appropriately selected and administered than other classes of antimicrobial, cefazolin and cefuroxime were the first antimicrobial of choice for majority of the surgical procedures, according to the guidelines composed by China Ministry of Health. In our study, although the most frequently prescribed antimicrobial were cefazolin and cefuroxime, antimicrobial selection was found to be inappropriate in 21.18% of cases before QCC intervention. Lower rates of appropriateness were demonstrated where broad-spectrum antimicrobial such as third-generation cephalosporins, piperacillin/tazobactam, etc., were prescribed, as they are associated with increased emergence of extended-spectrum β-lactamases and Clostridioides difficile strains. The selection of appropriate antimicrobial agents in the present study pre QCC intervention (78.82%) was higher to that of a recent study (55.3%),20 but lower to that reported by Pittalis (84.5%).21 While after the QCC intervention almost 96% received the appropriate antimicrobial agents for their surgical procedure.
Current antimicrobial prophylaxis in surgery guidelines recommend that the duration of SAP should not beyond 24 h after incision for clean procedures.22 However, in almost 10% of the procedures in our study, the duration of SAP exceeded this time limit. Previous studies demonstrated that prolonged SAP can alter the institutional antibiogram and an individual’s microbiome, which can lead to the emergence of bacterial resistance and may increase the incidence of antimicrobial-associated complications. Other studies revealed that a single intravenous dose or within 24 h administration of antimicrobial is enough to prevent postoperative infection in clean operations.23 In line with prior studies, our results showed that QCC intervention has no effect on the incidence of SSI, other surgical complications and antimicrobial-related ADR.
According to the international and native guidelines, some clean surgeries (such as breast and thyroid surgery, inguinal without a mesh, vascular vessel angiography, physical ablation of the tumor), antimicrobial prophylaxis was not recommended. However, in almost 6% of the procedures have no indication to use antimicrobial prophylaxis in our study. Antimicrobial overuse is the leading cause of antimicrobial resistance, and more than 30% of prescriptions are unnecessary according to the estimates of the United States Centers for Disease Control and Prevention.24 While after the QCC intervention, 99% of the antimicrobial prophylaxis have indication. Our findings highlight the importance of limiting antimicrobial use in SAP.
Implications for Policy, Practice and Research
Present study has implications for policy, practice and research into SAP. It highlights the reliability of the QCC activity in improving the appropriateness of SAP, supporting the use of quality management tools to carry out continuous quality improvement activities. Moreover, QCC activities cannot only acquire tangible results but also obtain several intangible results. Firstly, our present QCC activities enhanced the problem-solving capability of the circle members through regularly meet to identify, analyse and solve problems by integrating various quality management tools. Secondly, cross-professional cooperation is the ideal way to solve the problem in healthcare institutions. QCC activities allow multi-disciplinary teamwork to participate together, which is helpful to cultivate the team spirit during the implementation process of QCC, and brings greater benefits.
Conclusions
In conclusion, the QCC activity has achieved good results in promoting the appropriateness of SAP in patients undergoing clean surgery. Moreover, QCC activities could effectively improve the self-confidence, problem-solving capability and skills of quality control of medical staff, and deserved application and promotion in medical quality improvement activities.
Data Sharing Statement
Datasets used and/or analysed during the present study are available from the corresponding author on reasonable request.
Funding
This work was supported by the grants from the project of Chengdu Municipal Health Commission (No.2020106 and 2022236), and the project of Sichuan Hospital Management and Development Research Center (No.SCYG2022-03).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Rawson TM, Wilson RC, O’Hare D, et al. Optimizing antimicrobial use: challenges, advances and opportunities. Nat Rev Microbiol. 2021;19(12):747–758. doi:10.1038/s41579-021-00578-9
2. Glover RE, Knight GM, Chandler CIR. Antimicrobial resistance at the G7. BMJ. 2021;373:n1417. doi:10.1136/bmj.n1417
3. Maleknejad A, Dastyar N, Badakhsh M, et al. Surgical site infections in Eastern Mediterranean region: a systematic review and meta-analysis. Infect Dis. 2019;51:719–729. doi:10.1080/23744235.2019.1642513
4. Fields AC, Pradarelli JC, Itani KMF. Preventing surgical site infections: looking beyond the current guidelines. JAMA. 2020;323:1087–1088. doi:10.1001/jama.2019.20830
5. Dior UP, Kathurusinghe S, Cheng C, et al. Effect of surgical skin antisepsis on surgical site infections in patients undergoing gynecological laparoscopic surgery: a double-blind randomized clinical trial. JAMA Surg. 2020;155:807–815. doi:10.1001/jamasurg.2020.1953
6. Melling AC, Ali B, Scott EM, et al. Effects of preoperative warming on the incidence of wound infection after clean surgery: a randomised controlled trial. Lancet. 2001;358:876–880. doi:10.1016/S0140-6736(01)06071-8
7. Stefanou A, Worden A, Kandagatla P, et al. Surgical wound misclassification to clean from clean-contaminated in common abdominal operations. J Surg Res. 2020;246:131–138. doi:10.1016/j.jss.2019.09.001
8. Decker BK, Nagrebetsky A, Lipsett PA, et al. Controversies in perioperative antimicrobial prophylaxis. Anesthesiology. 2020;132:586–597. doi:10.1097/ALN.0000000000003075
9. China NHaFPCo. Principles of clinical use of antimicrobials [in Chinese]. 2015. Available from: http://www.gov.cn/xinwen/2015-08/27/content_29207.99.htm.
10. Muliani N, Herawati F, Yulia R, et al. Quantity and quality profiles of antibiotics pre, on, and post surgery in a hospital setting. Int J Clin Pharm. 2021;43:1302–1310. doi:10.1007/s11096-021-01251-0
11. Munchus G. Employer-employee based quality circles in Japan: human resource policy implications for American firms. Acad Manage Rev. 1983;8:255–261. doi:10.2307/257753
12. Zhang D, Yan Y, Liu TF. Key factors influencing the effectiveness of hospital quality management tools: using the quality control circle as an example-across-sectional study. BMJ Open. 2022;12:e049577. doi:10.1136/bmjopen-2021-049577
13. Liu Y, Lin B. Application of quality control circle in the treatment of moderate cancer pain in inpatients. Jpn J Clin Oncol. 2020;50:581–585. doi:10.1093/jjco/hyz214
14. Li J, Xu Q, Chen H, et al. Pharmacist-led quality control circle in sustained reduction of carbapenem-resistance at a Chinese tertiary teaching hospital. Ann Palliat Med. 2021;10:11558–11565. doi:10.21037/apm-21-2644
15. Zhong X, Xiao LH, Wang DL, et al. Impact of a quality control circle on the incidence of catheter-associated urinary tract infection: an interrupted time series analysis. Am J Infect Control. 2020;48:1184–1188. doi:10.1016/j.ajic.2020.01.006
16. Dimopoulou A, Kourlaba G, Psarris A, et al. Perioperative antimicrobial prophylaxis in pediatric patients in Greece: compliance with guidelines and impact of an educational intervention. J Pediatr Surg. 2016;51:1307–1311. doi:10.1016/j.jpedsurg.2015.11.017
17. Tourmousoglou CE, Yiannakopoulou E, Kalapothaki V, et al. Adherence to guidelines for antibiotic prophylaxis in general surgery: a critical appraisal. J Antimicrob Chemother. 2008;61:214–218. doi:10.1093/jac/dkm406
18. Gyssens IC. Preventing postoperative infections: current treatment recommendations. Drugs. 1999;57:175–185. doi:10.2165/00003495-199957020-00004
19. Alshehhi HS, Ali AA, Jawhar DS, et al. Assessment of implementation of antibiotic stewardship program in surgical prophylaxis at a secondary care hospital in Ras Al Khaimah, United Arab Emirates. Sci Rep. 2021;11:1042. doi:10.1038/s41598-020-80219-y
20. Bianchini S, Morini C, Nicoletti L, et al. Surgical antimicrobial prophylaxis in patients of neonatal and pediatric age subjected to eye surgery: a RAND/UCLA appropriateness method consensus study. Antibiotics. 2022;11:561.
21. Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70:195–283. doi:10.2146/ajhp120568
22. Miranda D, Mermel LA, Dellinger EP. Perioperative antibiotic prophylaxis: surgeons as antimicrobial stewards. J Am Coll Surg. 2020;231:766–768. doi:10.1016/j.jamcollsurg.2020.08.767
23. Zhang W, Meng H, Mao C, Hu Y. Utilization of neurosurgical perioperative antimicrobial prophylaxis in a Chinese teaching hospital. Int J Clin Pharm. 2021;43:1191–1197. doi:10.1007/s11096-021-01233-2
24. Park SY, Moon SM, Kim B, et al. Appropriateness of antibiotic prescriptions during hospitalization and ambulatory care: a multicentre prevalence survey in Korea. J Glob Antimicrob Resist. 2022;29:253–258. doi:10.1016/j.jgar.2022.03.021
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
