Back to Journals » OncoTargets and Therapy » Volume 9
Survival prognostic factors for patients with synchronous brain oligometastatic non-small-cell lung carcinoma receiving local therapy
Authors Bai H, Xu J, Yang H, Jin B, Lou Y , Wu D, Han B
Received 19 February 2016
Accepted for publication 7 May 2016
Published 11 July 2016 Volume 2016:9 Pages 4207—4213
DOI https://doi.org/10.2147/OTT.S106696
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Min Li
Hao Bai,1,* Jianlin Xu,1,* Haitang Yang,2,* Bo Jin,1 Yuqing Lou,1 Dan Wu,3 Baohui Han1
1Department of Pulmonary, 2Department of Pathology, 3Central Laboratory, Shanghai Chest Hospital, Shanghai Jiao Tong University, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Introduction: Clinical evidence for patients with synchronous brain oligometastatic non-small-cell lung carcinoma is limited. We aimed to summarize the clinical data of these patients to explore the survival prognostic factors for this population.
Methods: From September 1995 to July 2011, patients with 1–3 synchronous brain oligometastases, who were treated with stereotactic radiosurgery (SRS) or surgical resection as the primary treatment, were identified at Shanghai Chest Hospital.
Results: A total of 76 patients (22 patients underwent brain surgery as primary treatment and 54 patients received SRS) were available for survival analysis. The overall survival (OS) for patients treated with SRS and brain surgery as the primary treatment were 12.6 months (95% confidence interval [CI] 10.3–14.9) and 16.4 months (95% CI 8.8–24.1), respectively (adjusted hazard ratio =0.59, 95% CI 0.33–1.07, P=0.08). Among 76 patients treated with SRS or brain surgery, 21 patients who underwent primary tumor resection did not experience a significantly improved OS (16.4 months, 95% CI 9.6–23.2), compared with those who did not undergo resection (11.9 months, 95% CI 9.7–14.0; adjusted hazard ratio =0.81, 95% CI 0.46–1.44, P=0.46). Factors associated with survival benefits included stage I–II of primary lung tumor and solitary brain metastasis.
Conclusion: There was no significant difference in OS for patients with synchronous brain oligometastasis receiving SRS or surgical resection. Among this population, the number of brain metastases and stage of primary lung disease were the factors associated with a survival benefit.
Keywords: non-small-cell lung carcinoma, oligometastases, brain, stereotactic radiosurgery, surgery
Introduction
Worldwide, lung cancer is the most frequently diagnosed cancer and the leading cause of cancer-related deaths.1 Among newly diagnosed patients, almost half are diagnosed with distant metastases. Brain metastasis represents one of the most common forms of distant metastases2,3 and are discovered in up to 10% of patients at initial diagnosis of non-small-cell lung carcinoma (NSCLC).4 The prognosis of patients with brain metastasis is poor, with a median survival of 1–2 months without any treatment.5 According to a previous research, selected patients who present with synchronous brain-only oligometastases might have a better survival rate than expected.6 For this population, treatment of metastatic locations with surgery or stereotactic radiosurgery (SRS) has been proven to be an effective local therapy. However, clinical evidence in this distinct subset of the population is controversial. Some experts hold the view that neurosurgery provides longer survival time than SRS,7 while other studies demonstrated that SRS alone can result in similar benefits compared with neurosurgery plus whole-brain radiation therapy (WBRT).8–10 Furthermore, some studies showed that resection of the primary lung tumor might provide better survival benefits for synchronous brain oligometastases in patients receiving effective local therapy such as neurosurgery or SRS.10 In this study, we summarized the clinical data of this population of patients with brain metastases in our institution to analyze survival results and prognostic factors.
Methods
Study design and patients
The study was approved by the Institutional Review Board of Shanghai Chest Hospital which waived the need to obtain patient consent. All patients were diagnosed at Shanghai Chest Hospital between September 1995 and July 2011. Inclusion criteria were as follows: 1) patients with identifiable primaries, 1–3 synchronous brain metastases by computed tomography, magnetic resonance imaging, or positron emission tomography, and no other evidence of distant metastatic disease confirmed by computed tomography, bone scan, or positron emission tomography and 2) patients underwent SRS or surgical resection as initial treatment for local control. Baseline clinical characteristics included age at diagnosis, tumor histology, smoking history, stage of primary tumor, and number of brain metastases. Patients without survival and therapy details were excluded from the analysis. Clinical follow-up exams included a physical examination, an imaging examination, and routine laboratory tests, which were performed every 4–8 weeks. Overall survival (OS) was defined as beginning from the date of diagnosis until the date of death or last follow-up visit.
Statistical methods
For descriptive purposes, demographic and clinical data were summarized as medians with ranges for continuous variables and categorical variables by means of absolute and percentage numbers. Survival results were summarized as median values and two-sided 95% confidence interval (CI), and were analyzed using Kaplan–Meier technique. The log-rank test was used for comparisons among subgroups. Multivariable adjusted hazard ratios (HRs) for all-cause mortality by patient and treatment pattern were estimated using Cox regression analysis. HRs were calculated along with their corresponding 95% CIs as measurements of association. Statistical significance was defined as a P-value of less than 0.05. SPSS statistical software, version 22 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
Results
A total of 76 patients (22 underwent brain surgery as the primary treatment and 54 received SRS) were available for survival analysis. Among the 76 patients who received SRS or brain surgery as an initial treatment for local control, 21 underwent resection of the primary tumor, while 54 did not. Patient identification flowcharts are illustrated in Figure S1. Demographic data of all patients are shown in Table 1.
OS for patients treated with SRS and brain surgery as the primary treatment were 12.6 months (95% CI 10.3–14.9) and 16.4 months (95% CI 8.8–24.1), respectively (adjusted hazard ratio (HR) =0.59, 95% CI 0.33–1.07, P=0.08) (Figure 1). Comparison of baseline characteristics of the brain surgery cohort and the SRS cohort is shown in Table S1. During the course of their disease, five patients (22.7%) in the brain surgery cohort developed new brain metastasis and 13 (24.1%) patients in the SRS group had distant brain failure (P=0.90). The 1-year local tumor control rates for the brain surgery group and the SRS group were 81.8% and 88.9%, respectively (P=0.408).
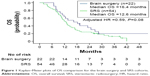  | Figure 1 Kaplan–Meier plots of OS comparison for the brain surgery and SRS cohorts. |
Among the 76 patients treated with SRS or surgical resection, factors associated with improved OS included stage I–II of the primary lung tumor (adjusted HR =0.53, 95% CI 0.29–0.98, P=0.042) and solitary brain metastases (adjusted HR =0.46, 95% CI 0.26–0.80, P=0.006) (Table 2). Patients who underwent resection of the primary tumor failed to experience a significantly improved OS (16.4 months, 95% CI 9.6–23.2) compared with those who did not undergo primary tumor resection (11.9 months, 95% CI 9.7–14.0) (Figure 2). Comparison of baseline characteristics of the thoracic surgery cohort and the no thoracic surgery cohort is shown in Table S2.
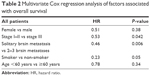  | Table 2 Multivariate Cox regression analysis of factors associated with overall survival |
  | Figure 2 Kaplan–Meier plots of OS comparison for thoracic surgery and no thoracic surgery cohorts. |
Discussion
Several prospective randomized trials have established surgical resection followed by WBRT or SRS as the standard local therapy for patients with synchronous brain oligometastatic NSCLC.11–14 However, this topic remains controversial. In this study, we summarized clinical data of patients with synchronous brain oligometastatic NSCLC in our institution to explore the prognostic factors associated with better survival in this population. The results demonstrated that surgical resection of brain metastasis and SRS appeared to provide a similar survival benefit. Among patients receiving SRS or brain surgery as local therapy, the number of brain metastases and stage of lung disease were the factors associated with a survival benefit. OS for patients undergoing primary tumor resection appeared to be longer than those who did not. However, after adjusting for age, stage, initial brain therapy, and number of brain metastasis, this difference was not found to be statistically significant.
Previous clinical trials compared survival outcomes for patients treated with SRS versus SRS + WBRT, and the results suggested that the addition of WBRT did not provide a survival advantage.14,15 Patchell et al11 showed that surgical resection followed by consolidative WBRT is better than surgery alone for local control of brain metastases. However, clinical evidence regarding surgical resection + WBRT versus SRS is limited. In a Phase III study, distant tumor control was less frequently achieved in the radiosurgery group compared with the microsurgery + WBRT group;8 and the treatment results did not differ in terms of survival (P=0.8). In another randomized trial, OS for radiosurgery + WBRT and surgery + WBRT were 6.2 and 2.8 months, respectively (P=0.20).16 However, both of those clinical trials were stopped early due to slow patient accrual. A retrospective study collected clinical data of patients with solitary brain metastasis, and demonstrated that radiosurgery alone can result in distant tumor control rates and OS comparable to that of surgery plus WBRT in selected patients.17 Similar results were also achieved in another retrospective study, which demonstrated no significant difference between surgical resection (SR) and SRS groups in terms of local control. The 6-, 12-, and 18-month local control rates were 84%, 73%, and 63% for patients in the SR group and 91%, 66%, and 66% for patients in the SRS group, respectively.18 In the present study, the 1-year local tumor control rates after surgery and SRS were 81.8% and 88.9%, respectively. There was no significant difference between brain surgery and SRS with regard to recurrence of brain metastasis. The OS appeared to be longer in the brain surgery cohort versus the SRS cohort. However, in the brain surgery cohort, 45.5% patients were stage I–II, while 72.7% patients had a solitary metastasis. Meanwhile, in the SRS cohort, 31.5% of patients were stage I–II and 59.3% patients had a solitary metastasis. Furthermore, patients in the brain surgery group appeared to be younger. After adjusting for these factors, OS in the brain surgery and SRS cohorts failed to achieve a statistical significant difference. The limitation of small sample size in this distinct population subset might partly explain the discrepancy of results in different studies. Recently, a system review summarized the clinical evidence in patients with single brain metastasis from NSCLC who underwent surgical resection and SRS.19 The results were consistent with those of the present study, which demonstrated comparable local control of brain metastases and OS benefits.
Li et al20 demonstrated that patients undergoing resection of brain metastasis and stage I and II NSCLC patients (34.9 months) had a significantly longer survival compared with stage III patients (8.9 months). Similarly, in the present study, favorable outcomes were associated with patients with stage I–II primary lung cancer. In the current study, multivariate analysis showed that the number of brain metastases was one of the most important factors to affect survival. Similarly, Wroński et al21 retrospectively collected survival data of patients undergoing surgical treatment of brain metastases; patients with single metastatic lesion survived longer than those with multiple metastases (11.1 vs 8.5 months, P<0.02). Another meta-analysis that summarized the data of three clinical trials demonstrated that patients with a single metastasis had significantly better survival rates compared with patients with 2–4 metastases.13
Previously, several studies demonstrated that primary lung tumor resection might be an option for synchronous oligometastatic NSCLC patients undergoing effective local therapy for distant metastasis.22,23 Hanagiri24 showed that selected patients who undergo surgical resection for the primary tumor and effective local therapy for metastatic lesions still have a chance to achieve long-term survival. Another prospective study demonstrated that clinical T1-2 N0-1 lung cancer with a single-organ metastatic lesion was appropriate for surgical resection. A 5-year survival rate of ~40% can be expected, which is comparable to that of stage II NSCLC.25 In the current study, OS for patients undergoing resection of the primary tumor also appeared to be longer than for patients who did not. After adjusting for age, stage, initial brain therapy, and number of brain metastasis, OS in the brain surgery and SRS cohorts failed to achieve a statistically significant difference. These results were different from previous reports, which demonstrated that aggressive therapy including resection of the primary lung tumor can help patients with synchronous brain oligometastases to significantly improve survival. The different characteristics of patients might partly explain the discrepancy of the results. In the current study, of the 21 patients who underwent brain surgery, only two patients did not have abnormal mediastinal lymph nodes. According to a previous study, the survival benefit of surgical treatment for lung cancer was significant if no abnormal mediastinal lymph nodes were found.26
This study has several limitations, including its retrospective nature. Also, the small sample size in each cohort might have affected the statistical analysis. A treatment selection bias may be present, affected mainly by initial clinical presentation and brain metastasis characteristics. What is more, the imbalance of additional WBRT therapy in different cohorts can cause a bias.
Conclusion
There was no significant difference in OS for patients with synchronous brain oligometastasis receiving SRS or surgical resection as local therapy. Among these, thoracic surgery appeared to result in a longer OS; however, after adjusting for baseline characteristics, this difference was not found to be statistically significant. The most important factors associated with a survival benefit are the number of brain metastases and stage of the primary lung disease.
Acknowledgments
This work was supported by Key Projects of the Biomedicine Department, Science and Technology Commission of Shanghai Municipality (Project No 11411951200). The funders played no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. | ||
Sørensen JB, Hansen HH, Hansen M, Dombernowsky P. Brain metastases in adenocarcinoma of the lung: frequency, risk groups, and prognosis. J Clin Oncol. 1988;6(9):1474–1480. | ||
Petrovich Z, Yu C, Giannotta SL, O’Day S, Apuzzo ML. Survival and pattern of failure in brain metastasis treated with stereotactic gamma knife radiosurgery. J Neurosurg. 2002;97(5 Suppl):499–506. | ||
Quint LE, Tummala S, Brisson LJ, et al. Distribution of distant metastases from newly diagnosed non-small cell lung cancer. Ann Thorac Surg. 1996;62(1):246–250. | ||
Richards P, McKissock W. Intracranial metastases. Br Med J. 1963;1(5322):15–18. | ||
Niibe Y, Chang JY. Novel insights of oligometastases and oligo-recurrence and review of the literature. Pulm Med. 2012;2012:261096. | ||
Bindal AK, Bindal RK, Hess KR, et al. Surgery versus radiosurgery in the treatment of brain metastasis. J Neurosurg. 1996;84(5):748–754. | ||
Muacevic A, Wowra B, Siefert A, Tonn JC, Steiger HJ, Kreth FW. Microsurgery plus whole brain irradiation versus gamma knife surgery alone for treatment of single metastases to the brain: a randomized controlled multicentre phase III trial. J Neurooncol. 2008;87(3):299–307. | ||
Schöggl A, Kitz K, Reddy M, et al. Defining the role of stereotactic radiosurgery versus microsurgery in the treatment of single brain metastases. Acta Neurochir (Wien). 2000;142(6):621–626. | ||
O’Neill BP, Iturria NJ, Link MJ, Pollock BE, Ballman KV, O’Fallon JR. A comparison of surgical resection and stereotactic radiosurgery in the treatment of solitary brain metastases. Int J Radiat Oncol Biol Phys. 2003;55(5):1169–1176. | ||
Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990;322(8):494–500. | ||
Andrews DW, Scott CB, Sperduto PW, et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet. 2004;363(9422):1665–1672. | ||
Sahgal A, Aoyama H, Kocher M, et al. Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. Int J Radiat Oncol Biol Phys. 2015;91(4):710–717. | ||
Kocher M, Soffietti R, Abacioglu U. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol. 2011;29(2):134–141. | ||
Aoyama H, Shirato H, Tago M, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA. 2006;295:2483–2491. | ||
Roos DE, Smith JG, Stephens SW. Radiosurgery versus surgery, both with adjuvant whole brain radiotherapy, for solitary brain metastases: a randomised controlled trial. Clin Oncol (R Coll Radiol). 2011;23(9):646–651. | ||
Muacevic A, Kreth FW, Horstmann GA, et al. Surgery and radiotherapy compared with gamma knife radiosurgery in the treatment of solitary cerebral metastases of small diameter. J Neurosurg. 1999;91(1):35–43. | ||
Bougie E, Masson-Côté L, Mathieu D. Comparison between surgical resection and stereotactic radiosurgery in patients with a single brain metastasis from non–small cell lung cancer. World Neurosurg. 2015;83(6):900–906. | ||
Qin H, Wang C, Jiang Y, Zhang X, Zhang Y, Ruan Z. Patients with single brain metastasis from non-small cell lung cancer equally benefit from stereotactic radiosurgery and surgery: a systematic review. Med Sci Monit. 2015;21:144–152. | ||
Li Z, Zhang X, Jiang X, et al. Outcome of surgical resection for brain metastases and radical treatment of the primary tumor in Chinese non–small-cell lung cancer patients. Onco Targets Ther. 2015;8:855–860. | ||
Wroński M, Arbit E, Burt M, Galicich JH. Survival after surgical treatment of brain metastases from lung cancer: a follow-up study of 231 patients treated between 1976 and 1991. J Neurosurg. 1995;83(4):605–616. | ||
Cheufou DH, Welter S, Chalvatzoulis E, Christof D, Theegarten D, Stamatis G. Surgery of primary lung cancer with oligometastatic m1b synchronous single brain metastasis: analysis of 37 cases. Thorac Cardiovasc Surg. 2014;62(7):612–615. | ||
Bella MJ, Kowalewski J, Dancewicz M, et al. Results of surgical treatment of primary lung cancer with synchronous brain metastases. Kardiochir Torakochirurgia Pol. 2015;12(1):14–17. | ||
Hanagiri T, Takenaka M, Oka S, et al. Results of a surgical resection for patients with stage IV non–small-cell lung cancer. Clin Lung Cancer. 2012;13(3):220–224. | ||
Endo C, Hasumi T, Matsumura Y, et al. A prospective study of surgical procedures for patients with oligometastatic non-small cell lung cancer. Ann Thorac Surg. 2014;98(1):258–264. | ||
Bonnette P, Puyo P, Gabriel C, et al. Surgical management of non-small cell lung cancer with synchronous brain metastases. Chest. 2001;119:1469–1475. |
Supplementary materials
  | Figure S1 Flow diagram of patients studied. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



