Back to Journals » Journal of Pain Research » Volume 14
Surgical Outcomes of Minimally Invasive Transforaminal Lumbar Interbody Fusion for Highly Migrated Lumbar Disc Herniation
Received 28 January 2021
Accepted for publication 19 May 2021
Published 4 June 2021 Volume 2021:14 Pages 1587—1592
DOI https://doi.org/10.2147/JPR.S303930
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Erika Petersen
Anqi Wang, Zhengrong Yu
Department of Orthopedics, Peking University First Hospital, Beijing, People’s Republic of China
Correspondence: Zhengrong Yu
Department of Orthopedics, Peking University First Hospital, XiShiku Street No. 8, XiCheng District, Beijing, People’s Republic of China
Tel +86-10-8357-2655
Email [email protected]
Objective: To describe minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) for highly migrated lumbar disc herniation (LDH) and assess its clinical outcomes.
Patients and Methods: This research retrospectively assessed 25 patients who were diagnosed with one-segmental highly migrated LDH and underwent MIS-TLIF in Peking University First Hospital from June 2015 to September 2019. Demographic data, perioperative parameters, complications, recurrence, and surgical outcomes were assessed.
Results: Twelve males and 13 females, with a mean age of 56.68 years old, were involved and the follow-up period was at least one year. The mean operation time was 222.16 minutes, the mean intraoperative hemorrhage was 250.00 mL, and the mean post-operative hospitalization was 5.76 days. The improvements in visual analog scale (VAS) and Oswestry disability index (ODI) were statistically significant. In addition, based on the MacNab criteria, 22 patients (88.0%) acquired satisfactory (good or excellent) results. One patient underwent post-operative epidural hematoma and recovered after evacuation of the hematoma. No recurrence was found.
Conclusion: MIS-TLIF is safe and effective and it can provide satisfactory clinical outcomes for highly migrated LDH.
Keywords: minimally invasive transforaminal lumbar interbody fusion, highly migrated lumbar disc herniation, clinical outcomes
Introduction
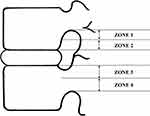
With a reported prevalence of 1–3%, lumbar disc herniation (LDH) is a prevalent spinal degenerative disease leading to surgery.1 Among LDH cases, migrated disc herniation refers to disc herniation either below the superior endplate level of the lower vertebral body or above the inferior endplate level of the upper vertebral body. As Lee et al.2 report, disc migration can be divided into four zones based on the orientation and distance from the disc space (Figure 1). Far-downward and far-upward migrations are defined as highly migrated LDH. Highly migrated LDH is more often associated with severe radicular symptoms or cauda equina syndrome compared with common LDH cases, because of the massive herniated disc pressing on nerve roots or cauda equina, which makes it hard to achieve satisfactory outcomes with conservative treatments.3 Hence, highly migrated LDH is more prone to surgery, and choosing an optimal operation approach is undoubtedly important.
Conventional open lumbar fusion surgery, with the advantages of wide view, easy accessibility to the target fragment, thorough discectomy and attainable vertebral stability, has been confirmed effective for highly migrated LDH.4 However, it requires prolonged paraspinal muscle retraction and extensive subperiosteal dissection, which inevitably results in muscle denervation and atrophy.5 First reported by Foley in 2003,6 minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) has become an ideal choice for the treatment of LDH; it is better than conventional open fusion surgeries in the aspects of decreased invasion to back muscles and bony structures, providing faster rehabilitation.7–14
Undeniably, highly migrated LDH cases were challenging for minimally invasive spine surgeries because of inadequate exposure and difficulty to touch and grasp the large and separated disc fragments.15,16 With the development of surgical equipment and techniques, several previous studies focused on the effectiveness and outcomes of some novel minimally invasive surgical approaches for migrated LDH.17–19 However, we are not aware of any previous study evaluating the surgical outcomes of MIS-TLIF for highly migrated LDH. Therefore, the purpose of the current study was to describe MIS-TLIF for a one-segmental highly migrated LDH case series and assess its surgical outcomes.
Patients and Methods
Research Subjects and Grouping
The medical data of 30 patients complaining of back and leg pain resulting from highly migrated LDH who received one-level MIS-TLIF by one surgeon (Y.Z.R.) in Peking University First Hospital from June 2015 and September 2019 were retrospectively reviewed and enrolled in the study. The surgeon presented a detailed written informed consent to the patients preoperatively. All participants provided informed consent to have their data used in this study. Patient data were collected independently from participants, and data were blindly analyzed. This study was approved by the Human Subjects Institutional Review Board at Peking University First Hospital.
The inclusion criteria were as follows: patients who (1) complained of severe low back pain and lower extremity symptoms associated with the migrated disc; (2) showed hypoesthesia and decreased muscle tone of lower limbs, positive straight-leg raising test and augmentation test; (3) had symptoms agreed with preoperative magnetic resonance imaging (MRI); (4) underwent unsatisfactory conservative treatment for at least 3 months; (5) had one-segmental far-upward/downward migrated disc herniation confirmed by MRI.
The exclusion criteria were as follows: patients who (1) had multi-segmental LDH; (2) had central stenosis or lateral recess stenosis on MRI; (3) had L1/2 or L2/3 disc herniation; (4) had near-upward/downward migrated disc herniation; (5) had lumbar spondylolisthesis and spondylolysis; (6) scoliosis (Cobb’s angle>15°); (7) life-threatening medical disease; (8) had undergone lumbar spine surgery before; (9) had deformities requiring correction, fractures, infections, tumors, etc.
Based on these criteria, 25 of the 30 patients were eventually included in the current research. Patients were well informed of the details about optional surgical procedures, complications, as well as the cost of the surgical methods, and the final choice was made by the patients.
Surgical Technique and Post-operative Management
C-arm machine and Quadrant System were prepared, and all the patients received general anesthesia before the surgery. Each patient was placed in the prone position on a radiolucent operating bed. A self-made locator confirmed the targeted level under C-arm fluoroscopy. We marked the pedicle positions (approximately 3.0 cm off midline) and the intervertebral spaces on the patient’s body surface according to the spatial relationship. Then we made a 2–3 cm skin incision on the more severe pathology side indicated by preoperative MRI, along the line between the outer portions of ends pedicles. The zygapophysis could be confirmed after splitting and retracting the paravertebral muscles laterally to the outer edge of the facet joint. Quadrant System was placed after inserting expansion tube. Repeated X-ray examination was necessary to reconfirm the target segments and the location of Quadrant System. Decompression was conducted by removing the inferior portion of the lamina, hypertrophied articular processes, as well as ligamenta flava. Then, the migrated disc was removed with grasping forceps. A suitable bullet-type interbody cage packed with autologous bone was knocked into the center of the intervertebral space the space was enlarged. Following these, under fluoroscopic guidance, we inserted ipsilateral percutaneous pedicle screws through the same skin incision, and contralateral percutaneous pedicle screws were inserted through a mirror incision. Then two titanium rods were symmetrically inserted and tightened on both sides (Figure 2). Finally, closure in layers was performed after adequate hemostasis and placing an incision drainage tube with negative pressure drainage.
Patients were allowed to take off-bed activities with a waist support 24 hours after the operation. The drainage tube could be removed when drainage fluid was less than 30 mL within one day.10 The patients were permitted to undertake non-manual work 2 weeks after the operation, and then return to full activity 3 months post-operatively. We encourage safe and sufficient rehabilitation activities with the protection of waist support within 3 months after operation.
Clinical Assessment
The demographic characteristics including age, sex, body mass index (BMI), herniation level, and conservative time from the participants were evaluated.
The perioperative parameters (operation time, intraoperative hemorrhage, and post-operative hospitalization), complication, and recurrence were also assessed.
Surgical outcomes, collected 1, 6, and 12 months post-operatively and compared with preoperative baseline, evaluated the improvement of back and leg pain according to visual analog scale (VAS), and the level of disability assessed with the Oswestry disability index (ODI) version 2.0. Clinical satisfaction was assessed based on the MacNab criteria20 by an independent surgeon at the 12-month post-operative follow-up. Excellent and good outcomes were rated as clinical satisfaction, which means at most occasional paresthesia or pain existed with no need for medication, and no restriction of daily activities.
Statistical Analysis
SPSS Statistics (Version 12, SPSS, Chicago, IL) was used to analyze the collected data. The statistics were illustrated as mean ± SD. Independent Student’s t-test and Chi-square test were used to compare the differences between preoperative and postoperative parameters. P < 0.05 was regarded as statistically significant.
Results
Demographic Characteristics of the Patients
Twelve males and 13 females, with a mean age of 56.68 (range 42–69) years old and a mean BMI of 25.89 kg/m2 were involved. The L4/5 was the most common herniation level (15 cases, 60.0%) followed by L5/S1 (6 cases, 24.0%) and L3/4 (4 cases, 16.0%). The mean conservative time was 7.44 months (Table 1). All the participants underwent one-segmental MIS-TLIF, and then were followed up for at least one year.
 |
Table 1 Demographic Characteristics (N = 25) |
Perioperative Outcomes, Complications, and Recurrence Condition
The mean operation time was 222.16 minutes, the mean intraoperative hemorrhage was 250.00 mL, and the mean post-operative hospitalization was 5.76 days (Table 2).
 |
Table 2 Perioperative Parameters, Complications, and Recurrence |
One patient suffered from post-operative complication of epidural hematoma and later recovered after evacuation of the hematoma. No recurrence occurred in 12 months post-operatively (Table 2).
Clinical Outcomes
VAS scores for back and leg pain, and ODI scores were significantly improved at 1, 6 and 12-month follow-ups compared with preoperative baselines (P<0.01). Based on the MacNab criteria, surgical satisfaction accounted for 88.0% of the involved patients (Table 3).
 |
Table 3 Clinical Outcomes |
Discussion
Highly migrated LDH is still a challenge for minimally invasive spine surgeries due to limited view and accessibility to the target fragment.21 With the development of endoscopic surgical equipment, several novel approaches of micro-discectomy were reported.3,17,18,21 However, non-fusion surgery resulted in a higher recurrence rate compared with interbody fusion surgery in our clinical practice and according to previous studies.22–24 The more aggressive removal of residual intervertebral disc fragments may reduce the risk of reherniation,25 but the degree of intervertebral disc degeneration in highly migrated cases is often higher than that in general LDH cases, thus residual disc may still exist for recurrence even though the volume of the removed herniation is large. In addition, large damage to the integrity of annulus fibrosus and posterior longitudinal ligament in highly migrated cases might alter the interlaminar shear stress, which makes the residual nucleus pulposus more prone to prolapse. The patients involved in the current study undertook physical labor with strong intensity in daily life and they had high demand for lumbar stability in their future life and work. Besides, to avoid stretch injury of nerve root, bone resection for the wide removal of the large migrated disc almost inevitably involves the articular process during the surgical procedure. The patients were well informed of these details and they preferred fusion surgery, so in this study we selected MIS-TLIF as a fusion surgical approach for highly migrated LDH and no recurrence case was found during postoperative follow-ups.
In this study, the operation time seemed relatively long, this might relate to the intricate operating steps and restricted visual scope of MIS-TLIF. Patients could acquire relatively short post-operative hospitalization and fast recovery of waist strength, due to minimal damage to spinous process ligaments and adjacent vertebral tissues.10,26,27
We found MIS-TLIF improved VAS scores of the back and leg pain, and decreased ODI at 1-, 6- and 12-month follow-ups. Referring to the MacNab criteria, 88.0% of the patients acquired surgical satisfaction, indicating that the MIS-TLIF was effective for highly migrated LDH.
In our study, the unilateral approach for bilateral decompression was performed to one case and this patient suffered from epidural hematoma post-operatively. When dealing with far-migrated disc fragments, iatrogenic injury to adjacent nerve roots, blood vessels or dural sac is more likely.15,28 Than et al.16 reported that the risks of dural laceration and cerebrospinal fluid leak might increase during the unilateral approach for bilateral decompression. Similarly, factors including tissue or scar adhesion around the spinal dural sac, limited intra-operative view, inadequate hemostasis, and obstructed drainage might associate with post-operative epidural hematoma. Additionally, the steep learning curves of the surgeon should be considered,29–31 experience accumulation and adequate knowledge of spine anatomy are key points to avoid these complications.
The present study has some limitations. First, the sample size is relatively small, and the follow-up period is relatively short. A prospective and multicenter study with more participants is needed to explore the long-term surgical outcomes. Furthermore, some other parameters including lumbar spine and adjacent degeneration stability need to be evaluated. Second, surgical choice in this research is limited and the control group was absent; it would be meaningful to compare the outcomes among more novel approaches such as PELD, micro-endoscopic discectomy (MED), open TLIF, posterior lumbar intervertebral fusion (PLIF) for highly migrated LDH in future studies. Third, there may be a bias resulting from the specific learning curves of the same experienced surgeon who performed all the operations.
Conclusions
MIS-TLIF is a safe and effective surgical choice and it can provide satisfactory clinical outcomes to patients with one-segmental highly migrated LDH.
Ethics
This study complied with the Declaration of Helsinki. All the participants provided informed consent to have their data used in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Frymoyer JW. Lumbar disk disease: epidemiology. Instr Course Lect. 1992;41:217–223.
2. Lee S, Kim SK, Lee SH, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation: classification of disc migration and surgical approaches. Eur Spine J. 2007;16(3):431–437. doi:10.1007/s00586-006-0219-4
3. Liu C, Chu L, Yong HC, Chen L, Deng ZL. Percutaneous endoscopic lumbar discectomy for highly migrated lumbar disc herniation. Pain Physician. 2017;20(1):E75–E84.
4. Ruan W, Feng F, Liu Z, Xie J, Cai L, Ping A. Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: a meta-analysis. Int J Surg. 2016;31:86–92. doi:10.1016/j.ijsu.2016.05.061
5. Mobbs RJ, Sivabalan P, Li J. Minimally invasive surgery compared to open spinal fusion for the treatment of degenerative lumbar spine pathologies. J Clin Neurosci. 2012;19(6):829–835. doi:10.1016/j.jocn.2011.10.004
6. Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976). 2003;28(15 Suppl):S26–35. doi:10.1097/01.BRS.0000076895.52418.5E
7. Sheng SR, Geng YB, Zhou KL, Wu AM, Wang XY, Ni WF. Minimally invasive surgery for degenerative spondylolisthesis: transforaminal or oblique lumbar interbody fusion. J Comp Eff Res. 2020;9(1):45–51. doi:10.2217/cer-2019-0055
8. Chen YC, Zhang L, Li EN, et al. An updated meta-analysis of clinical outcomes comparing minimally invasive with open transforaminal lumbar interbody fusion in patients with degenerative lumbar diseases. Medicine (Baltimore). 2019;98(43):e17420. doi:10.1097/MD.0000000000017420
9. Lin GX, Park CK, Hur JW, Kim JS. Time course observation of outcomes between minimally invasive transforaminal lumbar interbody fusion and posterior lumbar interbody fusion. Neurol Med Chir (Tokyo). 2019;59(6):222–230. doi:10.2176/nmc.oa.2018-0194
10. Yang Y, Liu ZY, Zhang LM, et al. Microendoscopy-assisted minimally invasive versus open transforaminal lumbar interbody fusion for lumbar degenerative diseases: 5-year outcomes. World Neurosurg. 2018;116:e602–e610. doi:10.1016/j.wneu.2018.05.049
11. Karikari IO, Isaacs RE. Minimally invasive transforaminal lumbar interbody fusion: a review of techniques and outcomes. Spine (Phila Pa 1976). 2010;35(26 Suppl):S294–301. doi:10.1097/BRS.0b013e3182022ddc
12. Parker SL, Adogwa O, Witham TF, Aaronson OS, Cheng J, McGirt MJ. Post-operative infection after minimally invasive versus open transforaminal lumbar interbody fusion (TLIF): literature review and cost analysis. Minim Invasive Neurosurg. 2011;54(1):33–37. doi:10.1055/s-0030-1269904
13. Mayer HM, Brock M. Percutaneous endoscopic lumbar discectomy (PELD). Neurosurg Rev. 1993;16(2):115–120. doi:10.1007/BF00258242
14. Peng CW, Yeo W, Tan SB. Percutaneous endoscopic lumbar discectomy: clinical and quality of life outcomes with a minimum 2 year follow-up. J Orthop Surg Res. 2009;4(1):20. doi:10.1186/1749-799X-4-20
15. Choi G, Lee SH, Lokhande P, et al. Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope. Spine (Phila Pa 1976). 2008;33(15):E508–515. doi:10.1097/BRS.0b013e31817bfa1a
16. Than KD, Mummaneni PV. Unilateral approach for bilateral decompression with MIS TLIF. World Neurosurg. 2014;82(5):646–647. doi:10.1016/j.wneu.2014.08.024
17. Du J, Tang X, Jing X, Li N, Wang Y, Zhang X. Outcomes of percutaneous endoscopic lumbar discectomy via a translaminar approach, especially for soft, highly down-migrated lumbar disc herniation. Int Orthop. 2016;40(6):1247–1252. doi:10.1007/s00264-016-3177-4
18. Wu X, Fan G, Gu X, Guan X, He S. Surgical outcome of two-level transforaminal percutaneous endoscopic lumbar discectomy for far-migrated disc herniation. Biomed Res Int. 2016;2016:4924013. doi:10.1155/2016/4924013
19. Zhao Y, Fan Y, Yang L, et al. Percutaneous Endoscopic Lumbar Discectomy (PELD) via a transforaminal and interlaminar combined approach for very highly migrated Lumbar Disc Herniation (LDH) between L4/5 and L5/S1 level. Med Sci Monit. 2020;26:e922777. doi:10.12659/MSM.922777
20. Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971;53(5):891–903. doi:10.2106/00004623-197153050-00004
21. Kim CH, Chung CK, Woo JW. Surgical outcome of percutaneous endoscopic interlaminar lumbar discectomy for highly migrated disk herniation. Clin Spine Surg. 2016;29(5):E259–266. doi:10.1097/BSD.0b013e31827649ea
22. Wang Y, Ning C, Xu F, et al. Recurrent lumbar disc herniation recurrence after percutaneous endoscopic lumbar discectomy: a case report. Medicine (Baltimore). 2018;97(34):e11909. doi:10.1097/MD.0000000000011909
23. Kim JM, Lee SH, Ahn Y, Yoon DH, Lee CD, Lim ST. Recurrence after successful percutaneous endoscopic lumbar discectomy. Minim Invasive Neurosurg. 2007;50(2):82–85. doi:10.1055/s-2007-982504
24. Yao Y, Zhang H, Wu J, et al. Comparison of three minimally invasive spine surgery methods for revision surgery for recurrent herniation after percutaneous endoscopic lumbar discectomy. World Neurosurg. 2017;100:641–647 e641. doi:10.1016/j.wneu.2017.01.089
25. Carragee EJ, Spinnickie AO, Alamin TF, Paragioudakis S. A prospective controlled study of limited versus subtotal posterior discectomy: short-term outcomes in patients with herniated lumbar intervertebral discs and large posterior anular defect. Spine (Phila Pa 1976). 2006;31(6):653–657. doi:10.1097/01.brs.0000203714.76250.68
26. Adogwa O, Parker SL, Bydon A, Cheng J, McGirt MJ. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech. 2011;24(8):479–484. doi:10.1097/BSD.0b013e3182055cac
27. Lee KH, Yue WM, Yeo W, Soeharno H, Tan SB. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2012;21(11):2265–2270. doi:10.1007/s00586-012-2281-4
28. Kim JS, Choi G, Lee SH. Percutaneous endoscopic lumbar discectomy via contralateral approach: a technical case report. Spine (Phila Pa 1976). 2011;36(17):E1173–1178. doi:10.1097/BRS.0b013e3182264458
29. Lau D, Lee JG, Han SJ, Lu DC, Chou D. Complications and perioperative factors associated with learning the technique of minimally invasive transforaminal lumbar interbody fusion (TLIF). J Clin Neurosci. 2011;18(5):624–627. doi:10.1016/j.jocn.2010.09.004
30. Lee DY, Lee SH. Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir (Tokyo). 2008;48(9):383–388; discussion 388–389. doi:10.2176/nmc.48.383
31. Wang H, Huang B, Li C, et al. Learning curve for percutaneous endoscopic lumbar discectomy depending on the surgeon’s training level of minimally invasive spine surgery. Clin Neurol Neurosurg. 2013;115(10):1987–1991. doi:10.1016/j.clineuro.2013.06.008
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.