Back to Journals » Infection and Drug Resistance » Volume 15
Supplementary Role of Immunological Indicators in the Diagnosis and Prognosis of Pneumocystis Pneumonia in Non-HIV Immunocompromised Patients
Authors Cao Y, Chen J , Dong L
Received 28 April 2022
Accepted for publication 6 August 2022
Published 21 August 2022 Volume 2022:15 Pages 4675—4683
DOI https://doi.org/10.2147/IDR.S372427
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Yaoqian Cao,* Jiayue Chen,* Lixia Dong
Department of Respiratory and Critical Care Medicine, Tianjin Medical University General Hospital, Tianjin, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Lixia Dong, Department of Respiratory and Critical Care Medicine, Tianjin Medical University General Hospital, Tianjin, People’s Republic of China, Tel +86 13001385918, Email [email protected]
Background: Pneumocystis pneumonia (PCP) has a high mortality in HIV-negative immunocompromised patients. The occurrence and development of PCP are believed to be correlated with the level of lymphocytes and their subsets. The aim of this study was to determine if the levels of lymphocyte subpopulations and immunoglobulin are associated with PCP.
Methods: A total of 74 immunocompromised patients were enrolled in this single-center cohort study. Diagnosis of PCP was based on the relevant pulmonary symptoms and radiological imaging, and the detection of Pneumocystis jirovecii in BAL fluid or biopsy tissue by metagenomic next-generation sequencing (mNGS). All patients were divided into two groups (PCP group and non-PCP group) and the patients in PCP group were then divided into two groupsbased on the outcome of the disease during the hospitalization.
Results: We observed a significant lower level of IgG (p=0.000) and B lymphocyte counts (p=0.017) in the PCP group comparing to that in the non-PCP group. CD4+ T cell counts, as well as the ratio of CD4+/CD8+ T cells in circulation and BAL fluid were also lower in the PCP group comparing to those in the non-PCP group. Lactate dehydrogenase (LDH) in the PCP group was significantly higher than that in the non-PCP group (p=0.029). In the PCP group, a lower level of total lymphocytes (p=0.004), T cells (p=0.001), CD4+ cells (p=0.001), and CD8+ cells (p=0.007), as well as the proportion of lymphocytes in BAL fluid (p=0.000) were found in deceased patients comparing to those in the survived group.
Conclusion: Our study revealed an important role of humoral immunity in the infection of Pneumocystis jirovecii. The level of B cells and IgG could be used as a supplement to predict the occurrence of PCP. The level of CD4+ and CD8+ lymphocytes was significantly correlated with the outcome of PCP.
Keywords: Pneumocystis jirovecii pneumonia, immunosuppression, HIV-negative, lymphocytes, immunoglobulin
Introduction
Pneumocystis jirovecii pneumonia (PCP) caused by Pneumocystis jirovecii is a life-threatening opportunistic fungal disease in immunocompromised patients. The overall mortality of PCP is estimated to be 20–30%1 and the in-hospital mortality rate is 32–65.6% in HIV-negative patients.2–5 The incidence of PCP is increasing significantly among non-HIV subjects due to the use of corticosteroids or immunosuppressants. The exact pathophysiology of PCP remains unclear, but it is believed that lymphocytes play a critical role in the disease development. A previous study suggested that CD4 + T lymphocyte counts might be a useful clinical marker to evaluate the risk for PCP in immunosuppressed patients.6 When the count of CD4+ T cells is below 200 cells/μL, the risk of PCP is significantly increased.7 High levels of CD8+ Tc1, low proportion of effector CD8+ T cells in blood1 and a high frequency of CD4+ Th1 cells in blood1 or bronchoalveolar lavage (BAL) fluid8 could be protective against PCP. In contrast, CD8+ Tc9 in BAL fluid could be detrimental to PCP patients.8
Even though cell-mediated immunity is more frequently emphasized, humoral immunity also plays an important role in the defense against Pneumocystis infection. B lymphocytes can produce antibodies and elicit T-cell immunity in patients with PCP.9–11 Previous studies have shown that PCP can occur in patients receiving anti-CD20 antibody (such as rituximab) therapy.12 Patients with severe hypogammaglobulinemia were predisposed to a higher incidence of opportunistic infections.13 The immunoglobulin production may be altered due to the changes in the B cells’ functions. The aim of this study was to determine if the levels of lymphocyte subpopulation and immunoglobulin are associated with the occurrence and severity of PCP in HIV-negative immunocompromised patients.
Methods
A total of 74 immunocompromised patients in Tianjin Medical University General Hospital were enrolled between August 2019 and February 2022. The inclusion criteria were as follows: (1) patients older than 18 years old; (2) ICU admission due to respiratory insufficiency; (2) negative serum HIV tests; (3) patients with one or more known causes of immunosuppression (chemotherapy for solid or hematologic cancer, bone marrow or solid organ transplantation, Immunosuppressive or corticosteroid therapies for autoimmune disease).
Patients were divided into PCP (n=44) and non-PCP (n=30) groups. Diagnosis of PCP was based on (1) the presence of relevant pulmonary symptoms (progressive dyspnea, fever, and/or cough); (2) radiological imaging consistent with PCP (ground glass opacities or abnormalities of interstitial lung tissue); and (3) detection of Pneumocystis jirovecii in BAL fluid or biopsy tissue by Metagenomic next-generation sequencing (mNGS) test. mNGS was performed within 24 h after the sample was obtained. DNA was extracted from of BAL fluid samples and lung tissue samples. DNA libraries were constructed through a process of DNA fragmentation, end-repair, adapter ligation, and PCR amplification. Agilent 2100 was used for quality control of the DNA libraries. The connector sequences, low-quality sequences and sequences from human genome were removed. The remaining sequences were aligned to the microbial genome database including genome sequences from 16,834 microbes (7982 bacteria, 7811 viruses, and 124 parasites).14 Patients diagnosed with PCP were then divided into survived group (n=31) and deceased group (n=13) according to the outcome of the disease during hospitalization.
The clinical data of patients including age, sex, and medical history were collected. The illness score was obtained by the Sequential Organ Failure Assessment (SOFA) on the day of admission. BAL fluid and blood samples were collected on the day of the diagnosis of PCP. Lymphocytes in BAL fluid and blood were characterized by flow cytometry following routine procedure. CD45-PerCP, CD19-APC, CD16-PE, CD56-PE, CD3-FITC, CD4-APC, and CD8-PE monoclonal antibodies were used according to the manufacturer’s instructions. Patients’ EDTA blood samples were stained by incubating with antibodies for 15 min. After lysis of erythrocyte and PBS washes, the samples were resuspended and measured on the flow cytometer (CytoFLEX, BECKMAN COULTER, USA). Analyses were performed by using CytExpert software (BECKMAN COULTER, USA). T lymphocytes were identified as CD3+/CD45+. B lymphocytes were identified as CD19+CD3-/CD45+. NK lymphocytes were identified as CD16+56+CD3-/CD45+.15 The gating strategies of phenotype analysis of lymphocytes were shown in Figure 1.
 |
Figure 1 The gating strategies of phenotype analysis of lymphocytes. |
Statistical analyses were performed using the IBM SPSS Statistics version 25. The distribution normality of all continuous variables was assessed by the Shapiro–Wilk test. Variables with normal distribution were presented as means ± standard deviation and analyzed by the Student’s t-test, otherwise as medians (with interquartile ranges) and analyzed by the Mann–Whitney U-test. Categorical variables were presented as percentages of the total and analyzed by the Chi-square test or Fisher’s exact test. A two-tailed P-value of <0.05 was considered statistically significant. The best thresholds for covariates with P < 0.05 were evaluated by receiver operating characteristic (ROC) curves and areas under the ROC curves (AUCs). For parameters that were significant based on univariate analyses, we used stepwise, forward logistic regression to test the influence of independent variables. A two-tailed P<0.05 was used to indicate statistically significant.
Results
Among the 74 immunocompromised patients, 44 patients were diagnosed with PCP, while the remaining 30 patients were included in the non-PCP group (Table 1). There was no significant difference in age, sex, underlying immunosuppressive diseases, the use of immunosuppressive agents, or the SOFA score between the PCP group and non-PCP group.
 |
Table 1 Clinical Characteristics and Laboratory Indicators in PCP and Non-PCP Groups |
Results of routine blood examination were also not significantly different between the two groups. The level of lactate dehydrogenase (LDH) in the PCP group was significantly higher than that in the non-PCP group (433.32±191.88 VS 326.83±209.34 U/L, p=0.029). The level of immunoglobulin (IgG) in the PCP group was significantly lower than that in the non-PCP group (667.22 VS 1117.75mg/dL, p=0.000). We then analyzed the subpopulations of lymphocytes and the results showed that B lymphocyte counts (p=0.017), CD4+ T cell counts (p=0.014), and the ratio of CD4+/CD8+ T cells (0.83 VS 1.24, p=0.014) in the circulation of PCP group was significantly lower than those in the non-PCP group. In BAL fluid, we also observed a significantly lower ratio of CD4+/CD8+ (0.87 VS 1.25, p=0.016) in PCP group comparing to the non-PCP group. ROC curves were performed to determine the best cut-off for all parameters that were statistically significant between PCP and non-PCP groups (Table 2 and Figure 2). An IgG level of 713.5mg/dL provided the best overall accuracy with an AUC of 76.4%. The positive predictive value (PPV) was 79.3% and the negative predictive value (NPV) was 62.9%. The other thresholds were LDH > 307.5U/L, B cells counts < 17cells/µL, CD4+ cell counts < 290.86cells/µL, CD4+/CD8+ ratio in blood< 0.56, and CD4+/CD8+ ratio in BAL fluid < 0.67. CD4+ cell counts had the highest specificity with a NPV of 68.2%. CD4+/CD8+ ratio in BAL fluid had the highest PPV, but the NPV was only 52%. We then conducted a stepwise logistic regression to identify the independent associations between PCP and variables. The results showed that IgG < 713.5mg/dL, CD4+/CD8+ ratio in BAL fluid< 0.67, LDH > 307.5U/L could be independent risk factors for PCP (Table 3). Within the PCP group, 31 (70.45%) patients survived, while the other 13 (29.55%) patients died during the hospitalization (Table 4). More males failed to survive the infection (45.16% VS 84.62%, p=0.016) comparing to females. SOFA score in the deceased group was significantly higher than that in the survived group. Other demographics were not significantly different between the deceased group and the survived group. As for the laboratory parameters, we observed that deceased patients had a significantly higher level of LDH and a lower level of total lymphocytes, T cells, CD4+ cells, and CD8+ cells, and the proportion of lymphocytes in BAL fluid.
 |
Table 2 Accuracy and Predictive Values of ROC Curve Analysis |
 |
Table 3 Stepwise, Forward Regression Analysis with All Possible Confounders |
 |
Table 4 Clinical Characteristics and Laboratory Indicators in the Survived and Deceased Groups |
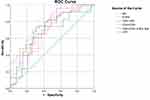 |
Figure 2 ROC curves for the performance of different parameters for PCP. |
Discussion
PCP is often severe and with high mortality. HIV-negative patients with PCP are usually associated with worse outcomes. Previous studies focused more on cell-mediated immunity in patients with PCP.1,8,16 In this study, we determined the differences in the proportion of subpopulations of lymphocytes and the level of immunoglobulin between PCP and non-PCP patients as well as between the survived and deceased PCP patients. Consistent with previous study, we showed that LDH in the PCP group was significantly higher than that in the non-PCP group, which could be due to the lung injury.17 However, we showed that there was no significant difference in the counts of total lymphocytes, CD3+ lymphocytes, and CD8+ lymphocytes between PCP and non-PCP groups. In contrast, we observed that patients with PCP were associated with a significant decrease of CD4+ T cells in blood and CD4+/CD8+ ratio in both circulation and BAL. Previous results on the association of CD4+ and CD8+ T cells with PCP remained controversial. Struijk et al18 revealed a significant reduction of CD4+ cells in non-HIV PCP cases. Li et al19 revealed a lower level of CD8+ cell counts in the PCP group. Tang et al17 showed that both CD4+ and CD8+ cells were decreased in non-HIV PCP patients. Ling et al showed that a decrease in CD4+/CD8+ ratio could predict PCP in non-HIV children.20 However, other studies showed that the level of CD4+, CD8+ cells, and CD4+/CD8+ ratio could not predict the infection of Pneumocystis jirovecii.1,8,21 Such inconsistency might be due to the different effects of specific CD8+ cell subpopulations, which is warranted for further investigations.
Previous studies showed that severe hypogammaglobulinemia was correlated with a higher incidence of opportunistic infections among patients receiving renal22 or heart13 transplantation. We showed that the patients with PCP were associated with a lower level of immunoglobulin G (IgG), and a level of IgG being lower than 713.5mg/dL could be a strong factor for the diagnosis of PCP. IgG is one of the most abundant serum proteins secreted by B lymphocytes and plays an important role in the adaptive immune response.23 A lower IgG level predisposes to a higher rate of serious infection events (SIE).24 Given that IgG level is decreased in patients following anti-CD20 antibody therapy,25,26 we hypothesized that the level of IgG is decreased due to the alteration of B-cell functions. Our results showed that B-cell counts were significantly reduced in patients with PCP, which is consistent with previous studies showing that a count of B cell <40 cells/µL was more frequent in patients with PCP.1,7 The cut-off for B cell count in our study was 17 cells/µL. In an animal model, similar results were observed. B cell-deficient mice showed more severe lung damage after infection with Pneumocystis.7 Although our results cannot determine whether the lack of B cells and hypogammaglobulinemia preceded the infection or developed after PCP, humoral immunity, especially the low level of B cells and IgG should be taken into consideration during the diagnosis and treatment of PCP.
We also showed that total lymphocytes in deceased patients were lower than those in the survived patients, which was consistent with previous studies.3,19,27 CD3+ lymphocytes include all types of T-lymphocytes and our results showed that the counts of CD3+ cells in deceased patients were significantly lower than those in the survived patients, which is consistent with previous studies.19 Another report suggested that a count of CD3+ cells < 300 × 10^6 cells/L was correlated with recurrent severe infections.28
With regard to the subpopulations of T lymphocytes, we found a significant reduction of CD4+ and CD8+ cells in the deceased patients comparing to those in the survived patients. CD4+ cells were believed to be critical for Pneumocystis jirovecii clearance.29 Several studies have suggested that lower CD4+ T cell counts are associated with poor outcomes in patients with PCP.27,30 CD8+ cells were also found to have a positive effect during the infection.19 Fan et al30 found that CD8+ counts ≤300 cells/μL were associated with a significantly higher in-hospital mortality. In murine models, CD8+ lymphocytes were believed to be a protective factor in response to Pneumocystis jirovecii during the depletion of CD4+ lymphocytes.31 During the infection, high number of CD8+ lymphocytes was recruited to the lung and may provide a potent protective effect by increasing the level of interferon-gamma (IFN-γ).31,32 However, some other animal studies showed a dual role of CD4+ and CD8+ cells during the infection.29,33 This may be explained by the different effects of particular subpopulations of CD4+ and CD8+ cells. Previous studies suggested that CD4+ Th11,34 and CD8+ Tc11,35 play a protective role in PCP. However, a higher level of CD8+ Tc98 in the lung could be detrimental. Therefore, further studies with the subsets of CD4+ and CD8+ cells are needed to identify the exact effects of different subsets of CD4+ and CD8+ on PCP. Our results indicated that the level of CD3+, CD4+, and CD8+ lymphocytes could be associated with the outcome of PCP.
There were several limitations in our study. First, our study was performed on a small number of patients. The results need to be verified by larger cohorts. Second, we did not examine the subpopulations of CD4+ and CD8+ lymphocytes. Further mechanistic studies are needed to determine the exact role of the subsets of T cells. Third, as a retrospective study, we could not determine whether the difference between groups precede the infection or the difference is caused by PCP. Thus, prospective studies with a larger patient cohort on a multi-center are needed to differentiate these two possibilities.
Conclusion
Collectively, we revealed that the level of B cells and IgG could be used as a supplement for the diagnosis of PCP, which also indicated an important role of humoral immunity during the infection. Monitoring of B cell number and IgG level can complement with other indicators in the assessment of PCP risk in non-HIV patients. Additionally, the data of our study suggested that there is a correlation between the level of T lymphocytes, especially CD4+ and CD8+ lymphocytes and the outcome of PCP. However, the role of the subsets of CD4+ and CD8+ cells in patients with PCP needs further investigation.
Data Sharing Statement
The data will be available on a reasonable request from the corresponding author.
Ethical Approval
All procedures performed in our study were in accordance with the ethical standards of the Medical Ethics Committee of Tianjin Medical University General Hospital and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. As the study design was retrospective, we used the currently existing samples collected during routine medical care and did not pose any additional risks to the patients. Thus the informed consent was waived by Medical Ethics Committee of Tianjin Medical University General Hospital.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Charpentier E, Marques C, Ménard S, et al. New insights into blood circulating lymphocytes in human pneumocystis pneumonia. J Fungi. 2021;7(8):652. doi:10.3390/jof7080652
2. Chen M, Tian X, Qin F, et al. Pneumocystis pneumonia in patients with autoimmune diseases: a retrospective study focused on clinical characteristics and prognostic factors related to death. PLoS One. 2015;10(9):e0139144. doi:10.1371/journal.pone.0139144
3. Wang Y, Huang X, Sun T, Fan G, Zhan Q, Weng L. Non-HIV-infected patients with Pneumocystis pneumonia in the intensive care unit: a bicentric, retrospective study focused on predictive factors of in-hospital mortality. Clin Respir J. 2022;16:152–161. doi:10.1111/crj.13463
4. Roblot F, Le Moal G, Godet C, et al. Pneumocystis carinii pneumonia in patients with hematologic malignancies: a descriptive study. J Infect. 2003;47(1):19–27. doi:10.1016/S0163-4453(03)00038-0
5. Ko Y, Jeong BH, Park HY, et al. Outcomes of Pneumocystis pneumonia with respiratory failure in HIV-negative patients. J Crit Care. 2014;29(3):356–361. doi:10.1016/j.jcrc.2013.12.005
6. Mansharamani NG, Balachandran D, Vernovsky I, Garland R, Koziel H. Peripheral blood CD4 + T-lymphocyte counts during Pneumocystis carinii pneumonia in immunocompromised patients without HIV infection. Chest. 2000;118(3):712–720. doi:10.1378/chest.118.3.712
7. Rong HM, Li T, Zhang C, et al. IL-10-producing B cells regulate Th1/Th17-cell immune responses in Pneumocystis pneumonia. Am J Physiol Lung Cell Mol Physiol. 2019;316(1):L291–l301. doi:10.1152/ajplung.00210.2018
8. Zhang NN, Huang X, Feng HY, et al. Circulating and pulmonary T-cell populations driving the immune response in non-HIV immunocompromised patients with Pneumocystis jirovecii pneumonia. Int J Med Sci. 2019;16(9):1221–1230. doi:10.7150/ijms.34512
9. Lund FE, Hollifield M, Schuer K, Lines JL, Randall TD, Garvy BA. B cells are required for generation of protective effector and memory CD4 cells in response to Pneumocystis lung infection. J Immunol. 2006;176(10):6147–6154. doi:10.4049/jimmunol.176.10.6147
10. Hoyt TR, Dobrinen E, Kochetkova I, Meissner N, Deepe GS. B cells modulate systemic responses to Pneumocystis murina lung infection and protect on-demand hematopoiesis via T cell-independent innate mechanisms when type I interferon signaling is absent. Infect Immun. 2015;83(2):743–758. doi:10.1128/IAI.02639-14
11. Rapaka RR, Ricks DM, Alcorn JF, et al. Conserved natural IgM antibodies mediate innate and adaptive immunity against the opportunistic fungus Pneumocystis murina. J Exp Med. 2010;207(13):2907–2919. doi:10.1084/jem.20100034
12. Martin-Garrido I, Carmona EM, Specks U, Limper AH. Pneumocystis pneumonia in patients treated with rituximab. Chest. 2013;144(1):258–265. doi:10.1378/chest.12-0477
13. Yamani MH, Avery RK, Mawhorter SD, et al. Hypogammaglobulinemia following cardiac transplantation: a link between rejection and infection. J Heart Lung Transplant. 2001;20(4):425–430. doi:10.1016/S1053-2498(00)00331-4
14. Zhang XQ, Lei Y, Tan XL, et al. Optimization of early antimicrobial strategies for lung transplant recipients based on metagenomic next-generation sequencing. Front Microbiol. 2022;13:839698. doi:10.3389/fmicb.2022.839698
15. van de Geijn GJ, van Rees V, van Pul-Bom N, et al. Leukoflow: multiparameter extended white blood cell differentiation for routine analysis by flow cytometry. Cytometry Part A. 2011;79(9):694–706.
16. Iriart X, Witkowski B, Courtais C, et al. Cellular and cytokine changes in the alveolar environment among immunocompromised patients during Pneumocystis jirovecii infection. Med Mycol. 2010;48(8):1075–1087. doi:10.3109/13693786.2010.484027
17. Tang G, Tong S, Yuan X, et al. Using routine laboratory markers and immunological indicators for predicting Pneumocystis jiroveci pneumonia in immunocompromised patients. Front Immunol. 2021;12:652383. doi:10.3389/fimmu.2021.652383
18. Struijk GH, Gijsen AF, Yong SL, et al. Risk of Pneumocystis jiroveci pneumonia in patients long after renal transplantation. Nephrol Dialysis Transplant. 2011;26(10):3391–3398. doi:10.1093/ndt/gfr048
19. Li Y, Ghannoum M, Deng C, et al. Pneumocystis pneumonia in patients with inflammatory or autoimmune diseases: usefulness of lymphocyte subtyping. Int J Infect Dis. 2017;57:108–115. doi:10.1016/j.ijid.2017.02.010
20. Ling C, Qian S, Wang Q, et al. Pneumocystis pneumonia in non-HIV children: a 10-year retrospective study. Clin Respir J. 2018;12(1):16–22. doi:10.1111/crj.12467
21. Weng L, Huang X, Chen L, et al. Prognostic factors for severe Pneumocystis jiroveci pneumonia of non-HIV patients in intensive care unit: a bicentric retrospective study. BMC Infect Dis. 2016;16(1):528. doi:10.1186/s12879-016-1855-x
22. Braun WE, Avery R, Gifford RW, Straffon RA. Life after 20 years with a kidney transplant: redefined disease profiles and an emerging nondiabetic vasculopathy. Transplant Proc. 1997;29(1–2):247–249. doi:10.1016/S0041-1345(96)00082-6
23. Vidarsson G, Dekkers G, Rispens T. IgG subclasses and allotypes: from structure to effector functions. Front Immunol. 2014;5:520. doi:10.3389/fimmu.2014.00520
24. van Vollenhoven RF, Emery P, Bingham CO, et al. Long-term safety of rituximab in rheumatoid arthritis: 9.5-year follow-up of the global clinical trial programme with a focus on adverse events of interest in RA patients. Ann Rheum Dis. 2013;72(9):1496–1502. doi:10.1136/annrheumdis-2012-201956
25. Parmentier C, Delbet JD, Decramer S, Boyer O, Hogan J, Ulinski T. Immunoglobulin serum levels in rituximab-treated patients with steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2020;35(3):455–462. doi:10.1007/s00467-019-04398-1
26. Colucci M, Carsetti R, Serafinelli J, et al. Prolonged impairment of immunological memory after anti-CD20 treatment in pediatric idiopathic nephrotic syndrome. Front Immunol. 2019;10:1653. doi:10.3389/fimmu.2019.01653
27. Freiwald T, Büttner S, Cheru NT, et al. CD4(+) T cell lymphopenia predicts mortality from Pneumocystis pneumonia in kidney transplant patients. Clin Transplant. 2020;34(9):e13877. doi:10.1111/ctr.13877
28. Shearer WT, Dunn E, Notarangelo LD, et al. Establishing diagnostic criteria for severe combined immunodeficiency disease (SCID), leaky SCID, and Omenn syndrome: the Primary Immune Deficiency Treatment Consortium experience. J Allergy Clin Immunol. 2014;133(4):1092–1098. doi:10.1016/j.jaci.2013.09.044
29. Bhagwat SP, Gigliotti F, Xu H, Wright TW. Contribution of T cell subsets to the pathophysiology of Pneumocystis-related immunorestitution disease. Am J Physiol Lung Cell Mol Physiol. 2006;291(6):L1256–66. doi:10.1152/ajplung.00079.2006
30. Jin F, Xie J, Wang HL. Lymphocyte subset analysis to evaluate the prognosis of HIV-negative patients with pneumocystis pneumonia. BMC Infect Dis. 2021;21(1):441. doi:10.1186/s12879-021-06124-5
31. Beck JM, Newbury RL, Palmer BE, Warnock ML, Byrd PK, Kaltreider HB. Role of CD8+ lymphocytes in host defense against Pneumocystis carinii in mice. J Lab Clin Med. 1996;128(5):477–487. doi:10.1016/S0022-2143(96)90044-X
32. Ruan S, Samuelson DR, Assouline B, Morre M, Shellito JE. Treatment with interleukin-7 restores host defense against pneumocystis in CD4+ T-lymphocyte-depleted mice. Infect Immun. 2016;84(1):108–119. doi:10.1128/IAI.01189-15
33. Gigliotti F, Crow EL, Bhagwat SP, Wright TW. Sensitized CD8+ T cells fail to control organism burden but accelerate the onset of lung injury during Pneumocystis carinii pneumonia. Infect Immun. 2006;74(11):6310–6316. doi:10.1128/IAI.00668-06
34. Myers RC, Dunaway CW, Nelson MP, Trevor JL, Morris A, Steele C. STAT4-dependent and -independent Th2 responses correlate with protective immunity against lung infection with Pneumocystis murina. J Immunol. 2013;190(12):6287–6294. doi:10.4049/jimmunol.1300431
35. McAllister F, Steele C, Zheng M, et al. T cytotoxic-1 CD8+ T cells are effector cells against pneumocystis in mice. J Immunol. 2004;172(2):1132–1138. doi:10.4049/jimmunol.172.2.1132
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
