Back to Journals » Psychology Research and Behavior Management » Volume 16
Suicidal Behaviors Among Active-Duty US Service Members: Data from the 2018 Health-Related Behaviors Survey
Authors Ahmed AE , Yim MH , Dawood J, Olsen CH, Waters AJ, Singer DE, Mancuso JD
Received 28 July 2023
Accepted for publication 31 October 2023
Published 7 November 2023 Volume 2023:16 Pages 4599—4615
DOI https://doi.org/10.2147/PRBM.S432835
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Igor Elman
Anwar E Ahmed,1 Michael H Yim,1 Jimmy Dawood,2 Cara H Olsen,1 Andrew J Waters,3 Darrell E Singer,1 James D Mancuso1
1Department of Preventive Medicine & Biostatistics, Uniformed Services University of the Health Sciences, Bethesda, MD, 20814, USA; 2School of Medicine, Uniformed Services University of the Health Sciences, Bethesda, MD, 20814, USA; 3Department of Medical and Clinical Psychology, Uniformed Services University of the Health Sciences, Bethesda, MD, 20814, USA
Correspondence: Anwar E Ahmed, Department of Preventive Medicine & Biostatistics, Uniformed Services University of the Health Sciences, Bethesda, MD, 20814, USA, Email [email protected]
Background: This study aimed to 1) determine the prevalence of past-year suicidal ideation (SI) and attempts (SA) among active-duty SMs; 2) determine whether differences exist by age, sex, and race; and 3) assess whether prevalence estimates vary by risk profiles of mental health conditions and substance use.
Methods: Data were from the 2018 Health-Related Behavior Survey (HRBS), a cross-sectional survey of active-duty SMs (n = 17,166). We used the logistic model to identify the factors of SI and SA and latent class analysis (LCA) to identify the risk profiles.
Results: Among active duty SMs, 8.26% had SI and 1.25% had SA in the past year. Gender and age have been shown to influence how race might contribute to suicidal behaviors. Mental health conditions were associated with higher odds of SI and SA, as were younger ages; LGB identity; being separated, divorced, or widowed; use of e-cigarettes, dual use of e-cigarettes and cigarettes, or drugs; and history of deployment of less than 12 months. Frequencies of cigarette and e-cigarette use were also associated with SI and SA, indicating the odds were increasing by 0.3% for every additional cigarette or e-cigarette used. Five risk profiles were identified: class 1 (illegal drug use), class 2 (mental health needs with tobacco and alcohol use), class 3 (mental health conditions only), class 4 (“low risk” SMs with low levels of illegal drug use, mental health visits, tobacco use, and alcohol use), and class 5 (alcohol use). Compared to class 4 (“low risk”), all other risk profiles were associated with increased odds of suicidal behaviors.
Conclusion: Despite the resources and increased access provided for mental health support, the prevalence of SI among active-duty SMs is greater than in the general population of the same age, likely due to additional military exposures and stressors.
Keywords: suicide, ideation, attempts, mental health, e-cigarette, active-duty service member
Introduction
Suicide was the second-leading cause of death among the 25–34 year old age group and the tenth-leading cause of death for all age groups in the US population between 2000 and 2020.1 Similarly, from 2006 to 2021, suicide, or self-inflicted death, represented 25.4% of deaths among US military active-duty servicemembers (SMs) and was second only to accidental (unintentional) as a cause of death.2 Between 2000 and 2012, suicide rates among SMs doubled; since 2012 there have been no appreciable changes in the annual rate of approximately 19.74 deaths per 100,000 service members. The rate of suicide in the civilian population was 14.2 per 100,000 in 2018, decreasing to 13.5 in 2020 and increasing to 14.0 in 2021.3 While the unadjusted rate among enlisted US military service members (SMs) is significantly higher than the US civilian population estimate,4 the age- and sex-adjusted military rate may be similar to the US adult population.5 Service in the military is voluntary and the demographic distribution among the US military is not representative of the US general population,6 and rates vary by model. Suicides and suicidal behaviors are preventable.7 Suicidal behaviors such as suicidal ideation (SI), suicide plans (SP), and suicide attempts (SA) represent key indicators for prevention efforts to reduce suicide-related deaths.8 Survey studies provide valuable self-reported information on the burden of suicidal behaviors among a population. It is common that survey studies use a single-item assessment of SI, SP, and SA to measure the presence or absence of each behavior during three timeframes (eg, lifetime, past year, and past month). For example, the lifetime prevalence estimates of SA, SP, and SI among military personnel are 2.4%, 5.3%, and 13.9%, respectively.8 A recent representative survey of Army members during their basic combat training reported similar estimates of SI (13.0%) and SA (1.7%).9 In contrast, a one-year study in the Air Force reported a lower prevalence of suicidal ideation of 3% among males and 5.5% among females, and 8.7% of the ideators reported SA.10 Suicidal behaviors during deployment have been of particular concern, although the estimates of medically documented SA among deployed SMs was low (0.4%).11 This indicates that estimates from medically documented records or administrative data might be lower than those obtained from surveys. We proposed this study to estimate the prevalence of suicidal behaviors using a survey because it represents an appropriate source for this estimation. In addition, most of the studies that assessed risk factors of suicidal behaviors among SMs were based on medically documented records or administrative data.12–15 In this vulnerable population, suicidal behaviors have been associated with demographic variables including young age,12 female gender,12–14 white race,14–16 marital status,10 high-school education or less,13,14 the first four years in service,13 and enlisted ranks.10 These studies have shown inconsistent findings as suicide remains to be a serious problem among non-White males in middle age and later life.17 This conflicting evidence warrants further investigation using an intersectional approach, as the contribution of race might depend on gender or age groups. To our knowledge, there has been no research assessing such associations in active-duty SMs. We aimed to address this gap to improve risk stratification of suicidal behaviors in clinical settings, particularly in the general medical practice and specialty clinics. Finally, studies among active-duty SMs have documented the association between suicidal behaviors and mental health conditions, including anxiety,16 depression,18 posttraumatic stress disorder,18 and having received a mental health diagnosis.18 These factors represent traditional risk factors for suicidal behaviors in the military and non-military populations.18,19 In this study, we 1) explored data-driven mental health conditions and substance use profiles in SMs, and 2) evaluated hypothesized relationships by assessing how different risk profiles correlate with suicidal behaviors. The Department of Defense (DoD) Survey of Health-Related Behaviors (HRBS) has been an important source of health behavior information for the military by surveying both active-duty and reserve components periodically since 1980.6,20 Research on suicidal behaviors is lacking in HRBS respondents. This study utilizes data from the 2018 HRBS of active-duty service members to 1) estimate the prevalence of Suicidal behaviors (SI and SA) among active-duty SMs; 2) determine whether differences exist by age, sex, and race; and 3) assess whether prevalence estimates vary by risk profiles of mental health conditions and substance use. We hypothesized that the latent class analysis would identify distinct groups of illegal drug users and mental health needs and that these groups would increase the odds of suicidal behaviors. We also hypothesized that sex and age might modify race differences in reporting suicidal behaviors.
Methods
Sample
Data were utilized from the 2018 DoD Health-Related Behavior Survey (HRBS). The sample analyzed consists of 17,166 active-duty SMs from the Army, Navy, Air Force, Marine Corps, and Coast Guard service branches. The 2018 HRBS’s response rate was 9.6%.20 The Institutional Review Board of the Uniformed Services University of the Health Sciences approved the study.
Measures
Suicidal Behavior Assessment
The HRBS uses a single-item assessment of past-year SI, SP, and SA to measure the presence or absence of each behavior. Respondents were classified as having SI if they selected “yes” for either of the following questions: At any time in the PAST 12 MONTHS, did you seriously think about trying to kill yourself?” and “During the PAST 12 MONTHS, did you make any plans to kill yourself?” SA were qualified with one question: “During the PAST 12 MONTHS, did you try to kill yourself?” Answer choices were limited to “no” and “yes”. We further explored past-year ideators to assess the burden of suicide attempts in this vulnerable group.10,21,22
Health Behaviors
We evaluated data on mental health conditions including mental health visits in the last year, perceived unmet mental health needs (yes/no), psychological distress in the past 12 months using the Kessler (K6) Psychological Distress Scale, and posttraumatic stress disorder in the past month as defined by the Primary Care Post Traumatic Stress Disorder (PC-PTSD) Screen for DSM-5. We assessed the reliability and validity of K6 and PC-PTSD-5 subscales among SMs. The reliability and predictive power of K6 and PC-PTSD-5 were determined using Cronbach’s alpha and areas under (AUC) the receiver operating characteristic curves. An optimal cutpoint was determined for each subscale using Youden’s index. Both subscales were reliable for use in this population; the Cronbach’s alpha was 0.90 for K6 and 0.81 for PC-PTSD-5. The validity assessment confirmed that both subscales were valid to assess SA and SI. The predictive ability of SA using K6 and PC-PTSD-5 was 0.83 and 0.69, respectively. The predictive ability of SI using K6 and PC-PTSD-5 was 0.81 and 0.70, respectively. For SA, K6 had an optimal cutpoint of 17.5, and PC-PTSD-5 had 3.5. For SI, K6 had an optimal cutpoint of 12.5, and PC-PTSD-5 had 3.5. We further evaluated the dimensionality of these two subscales using confirmatory factor analysis (CFA). With eigenvalue greater than one, the CFA analysis resulted in a single-factor dimension for K6 (accounting for 66.6%) and PC-PTSD-5 (accounting for 57.0%). The factor loading ranges between 0.73 and 0.89 for K6 and 0.72 to 0.81 for PC-PTSD-5. We assessed data on substances such as heavy alcohol use (yes/no); prescription drug misuse (stimulant, sedative, or pain medications—as measured by yes/no); and tobacco use status over the past 30 days (none, cigarettes only, e-cigarettes only, and dual use of e-cigarettes and cigarettes). Heavy alcohol use was defined as drinking 1–2 days, 3–4 days, 5–6 days, or about every day a week during the past 30 days.20 We examined the number of cigarettes smoked/day during the past 30 days and the number of e-cigarettes during the past 30 days. Respondents who skipped these two questions were recorded as no use or “0”. We also assessed the associations between the length of previous deployment and SI and SA. For latent class analysis (LCA), we evaluated specific substance use (1 = yes, 0 = no), including past 12 month use of: marijuana or hashish; other illegal drugs; cocaine; lysergic acid diethylamide (LSD); ecstasy; prescription stimulants or attention enhancers; prescription sedatives, tranquilizers, muscle relaxers, or barbiturates; prescription pain relievers; mental health visit; unmet mental health needs; cigarette use; e-cigarette use; cigar use; pipe/hookah use; heavy drinkers; binge drinking; any alcohol consequences; risky drinking and driving behaviors; PTSD-5; and K6.
Sociodemographic Variables
Each health behavior was analyzed in the context of sociodemographic characteristics that include the following: sex, race (Non-Hispanic White, Non-Hispanic Black, Hispanic, and Other), age groups (17–24, 25–34, 35–44, and 45 years and above), education (high school or less, some college, bachelor’s degree or more), marital status (married, cohabiting, never married, and separated, divorced, widowed), obesity (body mass index ≥30 kg/m2), lesbian, gay, or bisexual (LGB) (yes/no), service branch (Air Force, Army, Marine, Navy, and Coast Guard), and rank (officers or enlisted).
Statistical Analysis
Data analysis was performed using SAS 9.4 (TS1M7) (SAS Institute Inc., Cary, NC, USA). Sampling weights were used in all analyses. Sample characteristics were summarized by an overall weighted percent (%) estimates (Table 1). Weighted prevalence estimates of past-year SI, suicide plans, SA, and SA among SMs reporting SI (Table 2) were summarized by percent (%) and corresponding standard error (SE). The authors treated PC-PTSD-5 and K6 as continuous rather than dichotomous variables in all analysis. To assess intersectionality, we performed stratified analysis of SI and SA by age, sex, and race and ethnic group using the F-test. The crude and adjusted odd ratios of SI and SA were presented by sociodemographic characteristics (Table 3). However, to avoid multicollinearity, each health behavior and mental health condition was then assessed as a separate exposure after adjusting for sociodemographic variables using weighted logistic models (Table 4). The strength of the association was assessed by the odds ratio (OR) and 95% lower and upper confidence limits of (95% CI: LCL and UCL). The test is considered significant if the 95% CI does not contain the value 1.0. To detect unobserved heterogeneity and identify qualitatively different subgroups within the population based on patterns of covariate responses, we used LCA within a social determinant of health framework.23 LCA analysis was performed in Mplus (Version 8.8), and the LCA model included twenty items on substances and mental health conditions. The number of classes were selected based on goodness-of-fit statistics such as the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). LCA syntax in Mplus can be found in Appendix 1. We explored the association between suicidal behaviors and risk profiles by using the Rao-Scott chi-square test.
 |
Table 1 Characteristics of Study Respondents (n = 17,166) |
 |
Table 2 Weighted Prevalence Estimates by the Sample Characteristics and Health Behaviors |
 |
Table 3 Unadjusted/Adjusted Odds Ratio Estimates of Past-Year SI and SA by Socio-Demographic Characteristics |
 |
Table 4 Unadjusted/Adjusted Odds Ratio Estimates of Past-Year SI and SA by Health Behaviors |
Results
Table 1 demonstrates the prevalence estimates and sociodemographic characteristics of the population. Table 2 illustrates the overall prevalence estimates and across subgroups. The overall past-year prevalence estimates included: SI was found among 8.3% (95% CI: 7.50–9.02%), suicide plans 2.7% (95% CI: 2.31–3.15%), and SA among 1.2% (95% CI: 0.90–1.59%). SA among SMs reporting SI was found among 14.2% (95% CI: 10.46–17.92%). Differences in prevalence patterns were observed by demographic data, mental health conditions, substance use, and risk profiles (Table 2). For instance, prevalence of SI decreased with increasing age (11.1% among ages 17–24, 7.3% among ages 25–35, 5.6% among ages 35–44, and 3.1% among ages 45+ (F317163= 24.9, P < 0.0001)); as did SA (2.5% among ages 17–24, 0.5% among ages 25–35, 0.6% among ages 35–44, and 0.3% among ages 45+ (F317163=6.9, P = 0.0001)).
We found no association between SI and SA and race and ethnicity. However, we did observe differences in these outcomes by sex, age, and race and ethnicity (Figure 1). For example, among younger women (ages 17–24), the prevalence of SI was significantly higher among White women 16.6% (SE = 2.1) (F1,991=10.9, P = 0.001) and Hispanic women 16.4% (SE = 3.5) (F1,543=6.2, P = 0.013) than among Black women 5.8% (SE = 2.4). In contrast, among older women aged 45 years or more, the prevalence of SI was significantly higher in Black women 9.0% (SE = 3.7) than among White women 1.6% (SE = 0.8) (F1,301=4.4, P = 0.037). The intermediate prevalence of SI found among Hispanic women (5.9%, SE = 4.2) was not statistically different from either Black women (F1,94= 0.32, P = 0.575) or White women (F1,258= 1.0, P = 0.307).
 |
Figure 1 Weighted prevalence (%) of past-year suicide ideation (SI) (y-axis) among active-duty SMs by race/sex (x-axis) and age groups. Error bars represent 95% CIs. |
Table 3 shows that several sociodemographic factors were associated with increased adjusted odds of both SI and SA, including: younger age; lower education level; being divorced, separated, or widowed; LGB; enlisted rank; and service in the Army or Navy.
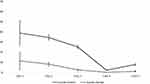
Table 4 presents the unadjusted associations between SI and SA and health behaviors and mental health history, as well as their associations after adjusting for the sociodemographic variables shown in Table 3. This shows a significant association between both SI and SA and the number of cigarettes/days for the past 30 days, number of e-cigarettes for the past 30 days, number of mental health visits, unmet mental health needs, PC-PTSD-5 scale, K6 scale, and history of deployment of less than 12 months. The only covariate associated with increased adjusted odds of SI but not SA was cigarette only (without e-cigarette) use. SI and SA were strongly associated with drug misuse, e-cigarettes only, and dual use of e-cigarettes and cigarettes. Figure 2 illustrates latent classes of substance use and mental health profiles. A five-class solution was chosen (BIC = 164,392.7, AIC = 163,586.6, entropy = 0.81, and Log-likelihood P < 0.0001). Class 4 (“low risk”, 64.84%) consisted of the majority of SMs and had low levels of illegal drug use, mental health visits, tobacco use, and alcohol use. Class 1 (“illegal drug use”, 0.63%) had the smallest proportion of SMs and was characterized by high levels of illegal drug use, as well as having high levels of mental health needs, tobacco use, and heavy alcohol use. Class 2 (“mental health needs with tobacco and alcohol use”, 6.45%) was similar to class 1 but without the illegal drug use. Class 3 (“mental health needs only”, 12.22%) had high levels of mental health needs but otherwise had low risk behaviors similar to class 4. Class 5 (“alcohol use”, 15.86%) was also similar to class 4 but had the highest levels of alcohol use and moderate levels of tobacco use. Prevalence estimates of SI and SA significantly varied by classes (Figure 3). For instance, class 1 (”drug use”, 38.9% and 11.4%), class 2 (”mental health needs with tobacco and alcohol use”, 34.5% and 8.2%), and class 3 (”mental health conditions only”, 25.2% and 2.7%) had significantly higher prevalence estimates of SI and SA than class 4 (”low risk”, 2.2% and 0.2%), respectively. Compared to those of class 4 ‘low risk’, class 1, 2, and 3 SMs were more likely to report past-year SI and SA (Table 4).
Discussion
We analyzed the representative DoD survey to estimate the prevalence of SI and SA and their associated factors among active-duty SMs. We found that one in twelve (8.26%) and one in eighty (1.25%) SM reported past year SI and SA, respectively.
We found that sociodemographic factors associated with increased adjusted odds of both SI and SA included younger age; lower education level; being divorced, separated, or widowed; LGB; enlisted rank; and service in the Army or Navy. Among the mental health and health behavior covariates, we found strong associations between both SI and SA and serious distress, mental health visits, PTSD, and unmet mental health needs. SI and SA were strongly associated with drug misuse, e-cigarettes only, and dual use of e-cigarettes and cigarettes.
SMs were clustered into five classes based on their substance use and mental health conditions. SMs with class 1 characteristics of “illegal drug use” were most likely to have both SI and SA. Those with characteristics of class 2 “mental health needs with tobacco and alcohol use” and class 3 “mental health conditions only” also had high levels of SI but progressively lower levels of SA.
While the prevalence of SI among 18–25 years old in the general US population was 3.4% in 2018,24 our study discovered a significantly higher prevalence of 11.1% (95% CI: 9.5–12.7%) among SMs in this same age range (or category). In contrast, the prevalence of SA among 18–25 years old in the general population was 1.9%,24 which was consistent with 2.45% (95% CI: 1.6–3.3%) among SMs of the same age. Snarr et al reported a past-year SI estimate in a sample limited to the Air Force SMs and found 3.8%.10 This is consistent with our past-year SI estimate when we limited our sample to the Air Force SMs of 4.8%. Our estimate of the proportion of SMs with SA (12%) among those who had SI was also slightly higher than that reported previously (8.7%) among Air Force SMs.10 Demographic factors, mental health conditions, and health behaviors associated with SI and SA were also consistent with the literature. SI and SA have been found to be associated with posttraumatic stress disorder, intermittent explosive disorder, panic disorder, and depression among Army soldiers,8 similar to our findings that both SI and SA were strongly associated with mental health conditions. Our study revealed that substance use such as drug misuse, e-cigarettes use, and dual use of e-cigarettes and cigarettes have been identified as risk factors for SI and SA. Similarly, Naifeh et al reported substance use associated with an increased risk of SA,25 and Campbell-Sills et al noted associations between nicotine dependence and increased odds of SI and SA among a sample of Army soldiers.26 We found consistent evidence that the number of cigarettes/day for the past 30 days and number of e-cigarettes for the past 30 days were both significantly associated with SI and SA, indicating the odds increasing by 0.3% for every additional cigarette or e-cigarette used. Mental health counselors or psychiatrists might consider screening for the level of tobacco dependence of an adolescent, and adolescent should, therefore, be carefully assessed as part of the psychiatric evaluation and management.
Naifeh et al also found that enlisted SMs deployed within the first 12 months of service have the highest risk of SA,27 and Ursano et al reported higher odds of SA among enlisted soldiers in the sixth month of deployment.18 These are similar to our findings of higher SI and SA prevalence among SMs deployed for less than 12 months and among younger and enlisted SMs.
Several studies have reported significantly higher prevalence of reporting suicidal behaviors among servicewomen12–14 and among the white race.14–16 In our study, suicidal behaviors did not differ by gender or race but did differ by their intersectional identities when stratified by age groups. For instance, young White servicewomen had a higher prevalence of SI when compared to young Black servicewomen. Contrastingly, White servicewomen aged 45+ had a lower prevalence of SI when compared to Black servicewomen aged 45+. These findings improve our understanding on how race, gender, and age may relate to suicidal behaviors and can help identify SMs at high risk.
Limitations
The data obtained for this study was obtained through a confidential web-based cross-sectional survey as opposed to anonymous, allowing for administrative data to be linked to responses. The remainder of the data included self-reported assessments of exposures and outcomes. The cross-sectional design precludes a causal interpretation of the associations found in this study due to the uncertain temporal relationship between exposures and outcomes. Self-reported assessments may have resulted in information bias due to perceived social desirability of responses, as well as possibly recall bias for those who had the outcomes. Although K6 and PC-PTSD-5 were reliable and valid to measure SA and SI in SMs, their optimal cutpoints might depend on psychiatric diagnosis and the population under study. There was no information about the type of mental illness, syndromic level, chewing tobacco, and snuff use. The low response rate likely resulted in non-response bias. However, we applied survey weights in all analyses to correct for the low survey response and selection bias. The results of this study may only apply to the US military population, as this population receives full direct care in the Military Health System and wider accessibility to behavioral and mental health clinics.28
Conclusions
The burden of SI is large among active-duty SMs compared to the general US population, particularly among younger SMs. This may be due to military stressors such as combat trauma, non-combat trauma, bullying, sexual assault, legal problems, relationship problems, or other factors.15 It is also noteworthy that 47% to 58% of those with suicidal behaviors first occurred prior to entry into military service.8 Nevertheless, this large burden of SI among active-duty SMs suggests the need for intensive interventions to detect, mitigate, and prevent these conditions. Our and other study findings suggest that SI and SA among SMs are associated with mental health conditions, health disparities and certain demographic groups, and health behaviors.
A large burden of mental health conditions in the US military population has been reported,29 with increased awareness of and demand for mental health services among SMs. Despite the resources and increased access to mental health support, the prevalence of SI among active-duty SMs appears greater than in the general population of the same age, likely due to additional military exposures and stressors. This study suggests that since mental health conditions are most strongly associated with SI and SA, the identification of these conditions is a critical element in the prevention and control of SI and SA. These study findings further highlight the magnitude of the public health challenge associated with SI and SA in the DoD and support the need for new strategies with high efficacy that are aimed at mitigating SI and SA. These strategies include evidence-based clinical mental health assessments using standardized and validated interviews and measures; evidence-based interventions such as dialectical behavior and cognitive therapies; and evidence-based prevention such as means restriction, provider and community-based education, and establishing a culture which promotes mental health and physical safety.19
This study also highlights the need for targeted effective prevention methods to address disparities in suicidal behaviors, including the higher prevalence of SI and SA among those of enlisted rank or with LGB identity. These groups have been suggested as priority populations for DoD health equity efforts.30 These and other demographic factors may also be used to identify and target interventions to those at highest risk, including not only enlisted and LGB SMs but also those who are younger, less educated, serve in the Army or Navy, or are divorced, separated, or widowed. This study also suggests that other co-occurring health behaviors are important factors which may influence SI and SA, including the use of drugs, alcohol, and e-cigarettes or dual-tobacco products. These health behaviors not only have other negative physical health effects which require their own public health and medical interventions but they also may be useful in identifying and targeting interventions to prevent and control the burden of SI and SA. Many of these behaviors were seen to be quite common in this study, and e-cigarette use and dual product use have been noted to be increasing in the military population.31 Mental health specialists should also consider these health behaviors as part of their mental health assessments and risk stratification for suicidal behaviors.
Data Sharing Statement
The data that support the findings of this study are available from the Defense Health Agency, however restrictions apply to the availability of these data, which were used under license for the current study, and thus are not publicly available.
Ethics Approval and Consent to Participate
The Health-Related Behavior Survey (HRBS) was conducted by the Defense Health Agency. The 2018 HRBS version has been updated and administered by the RAND Corporation. The final survey, the sampling plan, all communication with potential respondents, and the data security plan were reviewed by RAND’s Institutional Review Board (known as the Human Subjects Protection Committee), the Westat Institutional Review Board, the Coast Guard’s Institutional Review Board, the Office of People Analytics, the Office of the Under Secretary of Defense for Personnel and Readiness’s Research Regulatory Oversight Office, the Office of the Assistant Secretary of Defense for Health Affairs and the Defense Health Agency’s Human Research Protection Office, and the DoD Security Office. All survey materials included the survey report control system license number: DD-HA(BE)2189. Informed consent was required and obtained at the beginning of this web-based survey, and responses were confidential. The current study used secondary data, and the authors analyzed a de-identified data file. Because the data were previously collected and de-identified, the protocol for the present study was deemed exempt (not human subject research) by the Institutional Review Board of the Uniformed Services University of the Health Sciences. All methods were carried out in accordance with relevant guidelines and regulations (Declaration of Helsinki).
Acknowledgments
The contents, views, or opinions expressed in this publication or presentation are those of the authors. They do not necessarily reflect the official policy or position of the Uniformed Services University of the Health Sciences (USUHS), the Department of Defense (DoD), or the Departments of the Army, Navy, or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the US Government.
The 2018 DoD Health-Related Behavior Survey (HRBS) is the result of a collaboration between the Defense Health Agency and RAND. The authors thank the service members in the Air Force, Army, Marine Corps, Navy, and Coast Guard who contributed to this survey.
Funding
There is no funding to report.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Garnett MF, Curtin SC, Stone DM. Suicide mortality in the United States, 2000–2020. NCHS Data Brief. PMID: 35312475. 2022;433:1–8.
2. CRS. Trends in active-duty military deaths from 2006 through 2021. Washington DC: Library Of Congress. Available from: https://sgp.fas.org/crs/natsec/IF10899.pdf.
3. Curtin SC, Garnett MF. Provisional numbers and rates of suicide by month and demographic characteristics: United States, 2021. NVSS-Vital Statistics Rapid Release; 2021. Available from: https://www.cdc.gov/nchs/data/vsrr/vsrr024.pdf.
4. CDC. Web-based injury statistics query and reporting system (WISQARS). Atlanta, GA: US Department of Health and Human Services, CDC; 2021. Available from: https://wisqars.cdc.gov/cgi-bin/broker.exe.
5. Anglemyer A, Miller ML, Buttrey S, Whitaker L. Suicide rates and methods in active duty military personnel, 2005 to 2011: a cohort study. Ann Intern Med. 2016;165(3):167–174. doi:10.7326/M15-2785
6. Population representation in the military services: fiscal year 2019 summary report. Available from: https://www.cna.org/pop-rep/2019/summary/summary.pdf.
7. Kapp L Defense primer: military enlisted personnel. Washington DC: Library Of Congress. Available from: https://crsreports.congress.gov/product/pdf/IF/IF10684.
8. Nock MK, Stein MB, Heeringa SG, et al. Prevalence and correlates of suicidal behavior among soldiers: results from the army study to assess risk and resilience in servicemembers (Army STARRS). JAMA psychiatry. 2014;71(5):514–522. doi:10.1001/jamapsychiatry.2014.30
9. Naifeh JA, Ursano RJ, Stein MB, et al. Association of premilitary mental health with suicide attempts during US army service. JAMA Netw Open. 2022;5(6):e2214771. doi:10.1001/jamanetworkopen.2022.14771
10. Snarr JD, Heyman RE, Slep AM. Recent suicidal ideation and suicide attempts in a large‐scale survey of the US Air Force: prevalences and demographic risk factors. Suicide Life Threat Behav. 2010;40(6):544–552. doi:10.1521/suli.2010.40.6.544
11. LeardMann CA, Matsuno RK, Boyko EJ, Powell TM, Reger MA, Hoge CW. Association of combat experiences with suicide attempts among active-duty US service members. JAMA Netw Open. 2021;4(2):e2036065. doi:10.1001/jamanetworkopen.2020.36065
12. Ursano RJ, Kessler RC, Stein MB, et al. Medically documented suicide ideation among US Army soldiers. Suicide Life Threat Behav. 2017;47(5):612–628. doi:10.1111/sltb.12316
13. Ursano RJ, Kessler RC, Naifeh JA, et al. Risk factors associated with attempted suicide among US Army soldiers without a history of mental health diagnosis. JAMA psychiatry. 2018;75(10):1022–1032. doi:10.1001/jamapsychiatry.2018.2069
14. Ursano RJ, Kessler RC, Stein MB, et al. Suicide attempts in the US Army during the wars in Afghanistan and Iraq, 2004 to 2009. JAMA psychiatry. 2015;72(9):917–926. doi:10.1001/jamapsychiatry.2015.0987
15. Mash HB, Ursano RJ, Kessler RC, et al. Predictors of suicide attempt within 30 days after first medically documented suicidal ideation in US Army soldiers. Am J Psychiatry. 2021;178(11):1050–1059. doi:10.1176/appi.ajp.2021.20111570
16. Ursano RJ, Mash HB, Kessler RC, et al. Factors associated with suicide ideation in US Army soldiers during deployment in Afghanistan. JAMA Netw Open. 2020;3(1):e1919935. doi:10.1001/jamanetworkopen.2019.19935
17. Manton KG, Blazer DG, Woodbury MA. Suicide in middle age and later life: sex and race specific life table and cohort analyses. J Gerontol. 1987;42(2):219–227. doi:10.1093/geronj/42.2.219
18. Ursano RJ, Kessler RC, Stein MB, et al. Risk factors, methods, and timing of suicide attempts among US Army soldiers. JAMA psychiatry. 2016;73(7):741–749. doi:10.1001/jamapsychiatry.2016.0600
19. Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol. 2016;12:307–330. doi:10.1146/annurev-clinpsy-021815-093204
20. Meadows SO, Engel CC, Collins RL, et al. Department of defense health related behaviors survey (HRBS); 2018.
21. May AM, Klonsky ED, Klein DN. Predicting future suicide attempts among depressed suicide ideators: a 10-year longitudinal study. J Psychiatr Res. 2012;46(7):946–952. doi:10.1016/j.jpsychires.2012.04.009
22. Han B, Compton WM, Gfroerer J, McKeon R. Prevalence and correlates of past 12-month suicide attempt among adults with past-year suicidal ideation in the United States. J Clin Psychiatry. 2015;76(3):15414. doi:10.4088/JCP.14m09287
23. US Department of Health and Human Services. Social determinants of health: healthy People 2030. HealthyPeople. gov. Available from: https://health.gov/healthypeople/priority-areas/social-determinants-health.
24. Abuse S; Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2018 national survey on drug use and health (HHS Publication No. PEP19-5068, NSDUH Series H-54). Rockville, MD: Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration; 2019. Available from: https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf.
25. Naifeh JA, Ursano RJ, Kessler RC, et al. Transition to suicide attempt from recent suicide ideation in US army soldiers: results from the army study to assess risk and resilience in servicemembers (Army STARRS). Depress Anxiety. 2019;36(5):412–422. doi:10.1002/da.22870
26. Campbell-Sills L, Kessler RC, Ursano RJ, et al. Nicotine dependence and pre-enlistment suicidal behavior among us army soldiers. Am J Prev Med. 2019;56(3):420–428. doi:10.1016/j.amepre.2018.09.016
27. Naifeh JA, Ursano RJ, Kessler RC, et al. Early first deployment and risk of suicide attempt among first‐term enlisted soldiers in the US army. Suicide Life Threat Behav. 2020;50(2):345–358. doi:10.1111/sltb.12592
28. Wooten NR, Brittingham JA, Pitner RO, Tavakoli AS, Jeffery DD, Haddock KS. Purchased behavioral health care received by military health system beneficiaries in civilian medical facilities, 2000–2014. Mil Med. 2018;183(7–8):e278–90. doi:10.1093/milmed/usx101
29. Belsher BE, Jaycox LH, Freed MC, et al. Mental health utilization patterns during a stepped, collaborative care effectiveness trial for PTSD and depression in the military health system. Med Care. 2016;54(7):706–713. doi:10.1097/MLR.0000000000000545
30. Mancuso JD, Young J, Rusiecki J, et al. Advancing health equity in the US military. J Health Dispar Res Pract. 2023;16(1):38–50.
31. Keltner CH, Kao TC, Ahmed A, Mancuso JD. E-cigarette and dual product use as an emerging health threat to the US military. Tob Prev & Cessation. 2021;7:1–12. doi:10.18332/tpc/135516
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.