Back to Journals » Clinical Ophthalmology » Volume 15
Successful Implementation of Femtosecond Laser-Assisted Cataract Surgery: A Real-World Economic Analysis
Authors George DS , Ainslie-Garcia MH, Ferko NC, Cheng H
Received 20 November 2020
Accepted for publication 8 February 2021
Published 2 March 2021 Volume 2021:15 Pages 923—929
DOI https://doi.org/10.2147/OPTH.S293111
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
David S George,1,2 Margaret H Ainslie-Garcia,3 Nicole C Ferko,3 Hang Cheng4
1The Eye MDs, Parkersburg, WV, USA; 2Physicians Outpatient Surgery Center, Belpre, OH, USA; 3EVERSANA™, Burlington, ON, Canada; 4Alcon Vision LLC., Fort Worth, TX, USA
Correspondence: David S George
The Eye MDs, 418 Grand Park Dr #315, Parkersburg, WV, 26104, USA
Email [email protected]
Purpose: To calculate the minimum number of Femtosecond laser-assisted cataract surgery (FLACS) procedures required per month to pay off the fixed investment cost over 5 years to achieve break-even.
Setting: A rural ophthalmology practice located in the mid-West United States.
Design: An economic analysis, based on real-world, retrospectively collected data over 12 months, from an ambulatory surgical care perspective.
Methods: FLACS was initiated in 2017 with the LenSx® laser (Alcon Vision LLC., Fort Worth, TX). The incremental cost of FLACS, cases needed to break-even, return on investment (ROI), patient education, and marketing efforts were assessed. The financial analysis considered cataract volume, conversion rates, fixed (eg, principal) and variable (eg, supplies) costs, and revenue in the first 12 months.
Results: The clinic performed 2717 cataract surgeries in the 12-month period, with 1304 (48%) of patients converting to FLACS. Of FLACS procedures, 613 (47%) selected an advanced-technology intraocular lens (AT-IOL; eg, toric or lifestyle IOL), and the remaining patients selected a monofocal IOL with laser astigmatism correction. FLACS increased AT-IOL use by 113 procedures (23%) compared to volumes in the year prior to FLACS. Overall, FLACS was predicted to be profitable, with only 13 cases required per month to break even in 5 years. If both facility and physician fees are considered revenue, only eight cases per month are required to break-even in 5 years.
Conclusion: The practice experienced a greater-than-anticipated conversion to FLACS and increased selection of AT-IOLs, well above the break-even volume required, contributing to a rapid return on their investment.
Keywords: cataract surgery, economic, return on investment, financial pro-forma, femtosecond laser
Introduction
Healthcare costs and demand continue to rise globally, which poses issues for finite budgets. This is especially evident in cataract surgery, as this is one of the most frequently performed surgical procedures in developed countries.1 There has been a decline in reimbursement for cataract surgery since 1985 of 69%.2 Many surgeons are concerned about the financial viability of non-refractive cataract surgery due to declining reimbursement.2 Advanced-technology intraocular lenses (AT-IOLs; eg, those correcting astigmatism or presbyopia) can provide an additional source of revenue for ophthalmologists. However, few patients opt for these lenses, so many cataract cases are performed at the lowest level of reimbursement. At the same time, patient expectations of cataract surgery are changing from simple removal of visual obstruction to that of restoring normal vision and achieving spectacle independence.2–4 Unsatisfied patients pose a risk for reputation and referrals, which are key to continued success.
Femtosecond laser-assisted cataract surgery (FLACS) helps automate the creation of corneal incisions, capsulorhexis, and pre-cuts the lens prior to the intraocular steps of surgery.5 This automation can help reduce procedural variation and improve technical accuracy. Several meta-analyses that compare FLACS with manual cataract surgery have been published, with FLACS often showing improved capsulorhexis circularity, lower central corneal thickness and endothelial cell loss, lower phacoemulsification time and power, and improved corrected distance visual acuity.6–8 Such advancements in technology may help to build patient satisfaction and optimize clinical practice success.
Over the last several years, there has been a large shift in the site of cataract surgery from hospital outpatient departments to ambulatory surgical centers (ASCs). In fact, the proportion of cataract surgeries performed at ASCs increased from 43.6% in 2001 to 73.0% in 2014.9 In the face of healthcare funding constraints and declining reimbursement rates, ASCs need to evolve to remain financially viable, while retaining and attracting required patient volumes. Adoption of FLACs may represent an important opportunity that helps to achieve these objectives, given its proven incremental benefits, demonstrated safety, and its use in many “premium” refractive services that provide additional revenue, including astigmatism correction, and implantation of AT-IOLs. Adding technologies with increased precision and reproducibility can help to increase patient confidence and overall satisfaction.
However, there are concerns with adopting FLACS technology, including the capital investment and per-procedure costs, and patient acceptance and willingness to pay.10 The magnitude of increase in practice revenue is dependent on the financial details of implementation, which impact subsequent incremental increases in revenue. Limited studies are currently published which comprehensively assess these factors. As such, a United States (US) economic analysis was conducted by a three-physician ophthalmology practice to determine the minimum number of FLACS procedures required per month to pay off fixed investment costs over 5 years. This study will help to illustrate how other clinics can predict the return on investment (ROI) according to their own setting parameters.
Methods
This three-surgeon ophthalmology practice is located in an Appalachian region, servicing a mostly rural area of Ohio and West Virginia, USA. The practice has several strengths, including a good local reputation with a large market share, and a history of offering innovative ophthalmology services, such as laser-assisted in situ keratomileusis (LASIK) and AT-IOLs. However, as the region’s average income was lower than the national average,11 there were concerns that uptake of the elective FLACS procedure and AT-IOLs would be limited. A business plan was developed to efficiently incorporate FLACS technology into the practice. This included the development of a marketing plan and patient education materials, as well as a fiscal projection to determine if FLACS was financially feasible (Table 1).
 |
Table 1 Schematic of Components Considered in Business Model for Integration of Femtosecond Laser-Assisted Cataract Surgery |
The practice began using FLACS in July 2017 after acquiring the LenSx® laser (Alcon Vison LLC., Fort Worth, TX). Cataract patients could select a standard surgery (monofocal IOL) with or without FLACS, or a fully refractive procedure (AT-IOL + FLACS). Patients with astigmatism could correct their astigmatism with laser incisions or a toric IOL. As they are not a covered benefit, the incremental charge for use of the laser for astigmatism management, and/or for any AT-IOLs were paid out-of-pocket by patients.12 For cataract patients selecting a monofocal IOL seeking additional refractive benefits, through imaging and arcuate incisions, only the additional charge of FLACS for astigmatism management would require patient payment.12
The marketing campaign included newspaper, radio, TV, billboards, website and Facebook ads to inform local patients that FLACS was now offered at the clinic. Patients opting for FLACS were surveyed to learn how they first heard about FLACS. Patients who chose traditional manual surgery were surveyed to determine what influenced their decision and how they heard about the clinic. Furthermore, patient education materials were developed for several stages of the patient pathway. Educational brochures were provided for offices of referring practitioners or optometrists, and a short video contrasting conventional and laser-assisted cataract surgery was provided to patients during their cataract evaluation at the office. Upon arrival to our clinic, patients referred for a cataract evaluation were provided with handouts of detailed information for surgery options, including conventional methods or bladeless (FLACS), astigmatism correction options, AT-IOL options, and price. The material included information on spectacle dependence after each surgery type (eg, that glasses would be needed for near vision after monofocal toric IOL surgery, and that glasses may still be needed for reading or low-light activities after lifestyle IOL surgery). An employee was designated the role of a dedicated “patient educator”. Several initiatives communicated directly to referring doctors, including the use of an existing practice ambassador to distribute education materials to referring offices, and hosting a continuing education meeting about FLACS at the surgery center. Referring doctors viewed a demonstration of laser incisions into a model acrylic eye and had an opportunity to ask questions regarding the technology.
The financial analysis was conducted by integrating data and calculations within a Microsoft Excel file that could vary several input values. Data collection was retrospective in nature and did not qualify as human subjects research as defined by either the Food and Drug Administration (21 CFR 50.3 g), 56.102e) or 21 CFR 812.3p)) or the Department of Health and Human Services (45 CFR 46.102e)1)); therefore, institutional approval was not needed. The analysis considered fixed and variable costs for the femtosecond laser, procedural costs (supplies, labor), and the average patient charge from a physician-owned ASC perspective (where both physician service fee and ASC fee are considered revenue) and an ASC-only perspective (excluding physician-component fees). The incremental time costs of a FLACS procedure were calculated by timing the femto portion of 75 consecutive FLACS cases and applying the wage cost. Specifically, it was determined that it takes an average of 5.35 minutes to conduct the femto portion of the procedure. Additional supply costs per FLACS case were limited to the SoftFit™ patient interface. Applying the hourly wage of the staff required to support a surgery gave a total of $57.10 in labor costs per FLACS case. Key inputs for the financial analyses are described in Tables 2 and 3. As financial details vary across practices, one-way and two-way sensitivity analyses were performed to determine break-even requirements for alternate labor costs (50% or 80% reduction) and/or revenue (20% and 50% reduction). A wide variation in revenue was selected to test the financial viability under increasingly conservative conditions, and improve the applicability of results globally, where labor costs, as well as revenue per case, are lower.13
 |
Table 2 Monthly Femto Cases Required to Break-Even for the Physician-Owned Ambulatory Surgical Center Perspective, Including Main Analysis and Sensitivity Analyses (5-Year Repayment Period) |
 |
Table 3 Monthly Femto Cases Required to Break-Even for the Ambulatory Surgical Center Perspective, Including Main Analysis and Sensitivity Analyses (5-Year Repayment Period) |
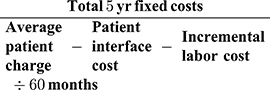
The number of FLACS cases required per month to break-even was calculated according to Equation 1. To determine whether the technology was worth the investment and its impact on practice finances, ROI was calculated over the 5-year period according to the classic definition of ROI, Equation 2,14 using data collected in the first year. Net income generated by FLACS was determined by subtracting the AT-IOL cost, the labor cost, and the interface supply cost from the FLACS revenue.
Equation 1: Number of FLACS Patients Per Month Required to Break-Even
Equation 2: Return on Investment
Results
The site increased marketing efforts in the year of FLACS initiation to increase awareness of FLACS and AT-IOLs. Overall, the site spent 3% of total business expenses on marketing, on par with the industry average, but higher than the annual 2% invested in years prior. However, as demonstrated in Table 4, a surprisingly low number of patients recognized any paid forms of marketing on the survey, as the majority of patients were identified through referral by doctors and other patients.
 |
Table 4 Survey Responses to Methods of Advertising That Led Patients to Select the Clinic |
FLACS was well received by patients, with over 1300 FLACS cases completed in the first 12 months (48% of the practice’s cataract cases opting for the new technology). Individual conversion rates between surgeons were similar, ranging from 47%-52%. FLACS increased the use of AT-IOLs, up 113 units (23%) compared to the 12-month period prior to FLACS initiation. FLACS also introduced a novel revenue stream from monofocal IOL recipients, with a monofocal IOL selected in 691 (53%) of FLACS procedures (Figure 1). Overwhelmingly, the main influence for selecting FLACS technology was a patient’s discussion with their doctor (identified by 123 [85%] of the 145 FLACS patients surveyed) followed by the patient educator (57 [39%]) and surgery scheduler (46 [32%]), with 30–41 (20–30%) of patients also identifying the patient handout, educational video, or discussion with the technician as influential. Similarly, most patients selecting FLACS identified the referring physician as the source that led them to the clinic (71 [49%]; Table 4). The three main reasons for selecting conventional cataract surgery were price sensitivity (identified by 75 [75%] of the 100 patients surveyed), lack of belief that FLACS had advantages (14 [14%]) and referring doctor advising against FLACS (4 [4%]).
 |
Figure 1 IOL selection and surgery types within FLACS procedures. |
When considering a 5-year payment plan, the economic analysis predicted that an average of 8 FLACS cases would be required per month to break-even in 5 years from the perspective of a physician-owned ASC, where both ASC and physician component fees are considered revenue (Table 2; Equation 1). As an alternate scenario, if only the facility fee is included as revenue, the break-even volume is predicted to increase to 13 cases per month (Table 3). As can be seen from sensitivity analyses within these tables, reduction in revenue per case had the largest impact on the number of cases required to break even. In either perspective, the highest case volume required was in the analysis with a 50% reduction in per-case revenue, and no reduction in labor cost. At these values, the physician-owned ASC would require 21 cases per month, while an ASC not receiving physician component fees would require 53 cases per month. Conversely, the most favorable break-even result is seen when revenue is unchanged and labor cost is reduced by 80%.
Data from the first year were used to estimate ROI for the repayment period of 5 years according to Equation 2. Dividing the net gains provided by FLACS by the procedural and fixed costs for the 5-year period demonstrated an ROI of 247%.
Discussion
This economic analysis was conducted to determine if FLACS could be financially viable in an ophthalmology practice servicing a mostly rural region in the mid-west US Study results showed that FLACS demonstrated an excellent financial trajectory within its first year of implementation and is predicted to remain a financial asset. Case volumes required for break-even were very reasonable with there being little concern as to whether these targets could be consistently met. Case volumes predicted under alternative assumptions remained in line with default findings and were highly achievable.
One of the primary concerns that physicians have with adopting FLACS technology is the significant capital investment required. However, this study clearly demonstrates that an ophthalmology clinic can be well compensated for the expense and maintenance costs of FLACS, not only by the secondary revenue stream that FLACS provides but also by the increased uptake of AT-IOLs. In fact, according to the ROI calculation, if first-year volumes remain stable over the 5-year period, this practice would see a return equal to double their total investments. This is in line with a national survey wherein the majority (86%) of ophthalmologists reported a positive outlook, anticipating a rapid return on investment due to patient volumes in excess of break-even requirements.15
From a physician-owned ASC perspective, 8 FLACS cases would be required each month to break-even in 5 years, while 13 would be required in the ASC-only perspective. This is comparable to a survey of 205 ophthalmologists in the US during the first years where FLACS was commercially available, which reported a volume of 19 cases per month to break-even. This analysis used a lower per-case margin of $532, and a higher 5-year average fixed cost of $603,400,15 due to the use of a variety of FLACS platforms (some of which cost in excess of $500,000).16 Break-even volumes in the current analysis are also comparable to a technology assessment from Canada, which reported a total break-even case load of 600 required by a clinic to support the acquisition of FLACS technology.17 Another analysis found a much higher annual patient volume required to support the FLACS technology (1400 cases); similarly, this used a more expensive laser with higher interest and lower patient out-of-pocket costs.16 The time required to break-even may be increased with higher laser or supply costs, while higher surgical volumes, patient charges, and the number of surgeons using the technology can all decrease the time to break-even.2,15,17
Another source of uncertainty in adopting FLACS technology is whether the patient conversion will be high enough to support the financial investment of FLACS.10,16 This study shows patient conversions were very high despite initial concerns that the region’s low average income would limit disposable income and the uptake of elective procedures. Within the first year, just under half of all cataract procedures were performed with FLACS, contributing to the excellent returns on investment. This is lower than the 63% to 65% conversion rate reported in other regions of the US with rural location or low average regional income,10,18 but higher than international FLACS conversion rates of 26% gathered during benchmarking initiatives (internal data regarding the LenSx® laser platform provided by Alcon).19 A lower conversion can be offset by high patient volumes, as seen in the current study, where actual monthly volumes were 8-times higher than required to break-even, and almost 2-times higher than nationally reported monthly volumes.15 This center was supported by three surgeons, which promotes the financial viability of FLACS as multiple surgeons can draw a larger patient volume.
Although patient education initiatives and satisfied patients leading to additional word-of-mouth referrals were instrumental in driving conversion, marketing initiatives had less impact than anticipated. The most expensive components of the advertising campaign were acknowledged as the reason for selecting FLACS in less than 12 (8%) patients. It is possible the marketing promoted the practice by keeping services in the forefront for local referring doctors and patients in general, and thus, indirectly supported referrals.
This study has some important limitations. First, economic results were of focus. As such, data was not rigorously collected to methodologically assess clinical outcomes across the entire sample. However, meta-analyses are increasingly demonstrating the improved benefits and safety of FLACS technology.6–8 These clinical findings, in combination with our economic analysis, can be interpreted as a win-win scenario for FLACS. Data collection on an appropriately powered sample can help to inform the clinical value of FLACS in more real-world settings. Second, long-term (5 years) predictions were based on data collected over a 12-month period. Nevertheless, predictions for required monthly case volumes were considerably lower than actual observed cases, even in the worst-case analysis where revenue was substantially reduced and labor costs remained high, rendering any uncertainty about predictions over the 5-year period to be low. Finally, the current analysis is clearly dependent on the assumed costs and revenue (patient charges), and only one (mostly rural) site was involved in this economic analysis which may not be representative of some other practices. However, costs in this study were considered conservative given that additional labor costs were also factored into the analysis, and sensitivity analyses were conducted to increase the generalizability of the results in a global audience where labor costs and patient willingness to pay may be considerably lower than in the United States. As well, in an effort to vary driving factors of the analysis to be more interpretable by other settings, this financial analysis assessed two settings. The first considers the break-even volume for a physician-owned ASC, where the physician would receive compensation for their role in the procedure (Table 2), and the second considers the perspective of a facility that would not receive physician-component fees (eg, use by independent physicians; Table 3). Future studies could analyze the first year of FLACS implementation in other regions with different considerations (eg, an urban setting, greater competition, or a smaller practice) to improve the generalizability of results.
The decision to adopt FLACS technology was an expensive undertaking and carried risk, but having a well-developed business plan inclusive of marketing, educational initiatives and a financial analysis allowed a successful launch and efficient integration of this new technology. In conclusion, patient acceptance of FLACS was high and conversion to AT-IOLs was higher than before the introduction of FLACS technology, which contributed to a rapid financial return at a US Mid-West ophthalmology practice. Education programs with multiple points of contact were believed to be critical to inform patients about FLACS technology, with minimal expenditure on paid marketing required as word-of-mouth referrals were high. Overall, FLACS was highly successful and is predicted to be profitable for the practice.
Conclusions
Medical practices must run as efficient businesses and must generate enough revenue to cover expenses. Ophthalmology is a therapeutic area facing increases in operating costs due to constant technological advancements, and a constant downward pressure on reimbursements due to the high procedural volumes. This study demonstrated that FLACS can provide ophthalmologists with additional revenue streams related to refractive services. The primary sources of uncertainty in adopting FLACS technology, significant capital investment and achieving sufficient patient volumes, were not a concern as FLACS was well accepted by patients and referring doctors, contributing to a rapid return on investment.
Abbreviations
AT-IOL, advanced technology intraocular lens; FLACS, femtosecond laser-assisted cataract surgery; IOL, intraocular lens; LASIK, laser in situ keratomileusis; ROI, return on investment; TV, television; U.S., United States.
Disclosure
DSG received financial compensation from Alcon for his consulting work; MHA and NCF are employees of EVERSANA™, which was contracted by Alcon to support the development of the manuscript; HC is an employee of Alcon. The authors report no other conflicts of interest in this work.
References
1. Erie JC. Rising cataract surgery rates: demand and supply. Ophthalmology. 2014;121(1):2–4. doi:10.1016/j.ophtha.2013.10.002
2. Bartlett JD, Miller KM. The economics of femtosecond laser-assisted cataract surgery. Curr Opin Ophthalmol. 2016;27(1):76–81. doi:10.1097/ICU.0000000000000219
3. Hawker MJ, Madge SN, Baddeley PA, Perry SR. Refractive expectations of patients having cataract surgery. J Cataract Refract Surg. 2005;31(10):1970–1975. doi:10.1016/j.jcrs.2005.03.065
4. Pager CK, McCluskey PJ, Retsas C. Cataract surgery in Australia: a profile of patient-centred outcomes. Clin Exp Ophthalmol. 2004;32(4):388–392. doi:10.1111/j.1442-9071.2004.00843.x
5. Alcon. LenSx® Laser Important Product Information for Cataract Treatment; 2019.
6. Chen X, Chen K, He J, Yao K. Comparing the Curative Effects between Femtosecond Laser-Assisted Cataract Surgery and Conventional Phacoemulsification Surgery: a Meta-Analysis. PLoS One. 2016;11(3):e0152088. doi:10.1371/journal.pone.0152088
7. Chen X, Xiao W, Ye S, Chen W, Liu Y. Efficacy and safety of femtosecond laser-assisted cataract surgery versus conventional phacoemulsification for cataract: a meta-analysis of randomized controlled trials. Sci Rep. 2015;5(1):13123. doi:10.1038/srep13123
8. Popovic M, Campos-Moller X, Schlenker MB, Ahmed II. Efficacy and Safety of Femtosecond Laser-Assisted Cataract Surgery Compared with Manual Cataract Surgery: a Meta-Analysis of 14 567 Eyes. Ophthalmology. 2016;123(10):2113–2126. doi:10.1016/j.ophtha.2016.07.005
9. Stagg BC, Talwar N, Mattox C, Lee PP, Stein JD. Trends in Use of Ambulatory Surgery Centers for Cataract Surgery in the United States, 2001–2014. JAMA Ophthalmol. 2018;136(1):53–60. doi:10.1001/jamaophthalmol.2017.5101
10. Swann F. Can your practice make a go of FLACS? Ophthalmol Management. 2019;12–16.
11. U.S. Census Bureau. American Community Survey 1-Year Estimates; 2017. Available from: https://www.census.gov/library/visualizations/2018/comm/acs-income-map.html. Accessed February 15, 2021.
12. Center for Medicare and Medicaid Services. CMS Ruling 05-01, Issued May 3, 2005 and 1536 R, 1. 22.2007by Department of Health and Human Services; 2005.
13. Lansingh VC, Carterd MJ, Eckertd KA, Winthrope KL, Furtadof JM, Resnikoffg S. Affordability of cataract surgery using the Big Mac prices. Revista Mexicana de Ofthalmologia. 2015;89(1):21–30. doi:10.1016/j.mexoft.2014.07.001
14. Brown MM, Brown GC, Lieske HB, Lieske PA. Financial return-on-investment of ophthalmic interventions: a new paradigm. Curr Opin Ophthalmol. 2014;25(3):171–176. doi:10.1097/ICU.0000000000000040
15. Lachman M. Femtosecond Laser Cataract Surgery: 2013 User Survey. Available from: https://crstoday.com/articles/2013-sep/femtosecond-laser-cataract-surgery-2013-user-survey/. Accessed February 15 2021.
16. Trigueros JA, Pinero DP, Ismail MM. Profitability analysis of a femtosecond laser system for cataract surgery using a fuzzy logic approach. Int J Ophthalmol. 2016;9(7):1046–1050. doi:10.18240/ijo.2016.07.18
17. Murtagh J. Femtosecond Laser-Assisted Cataract Surgery (FLACS) In. Issues in Emerging Health Technologies. 2014. 1753.
18. Williamson B It’s a Conversation, Not a Conversion. Available from: https://theophthalmologist.com/subspecialties/its-a-conversation-not-a-conversion.
19. Julie Anderson (Brand Manager LenSx® laser). 2017.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.