Back to Journals » Clinical Interventions in Aging » Volume 18
Suboptimal Use of DOACs Post-Discharge for Geriatric Hip Fractures with Isolated Calf Deep Vein Thrombosis: Do Clinician Prescribing Preferences and Patient Compliance Alters Clinical Outcomes?
Authors Wang Z, Lu Y , Wang P, Fei C, Li S, Xue H, Li Z, Wang Q, Zhang K, Ma T
Received 4 June 2023
Accepted for publication 6 August 2023
Published 28 August 2023 Volume 2023:18 Pages 1423—1436
DOI https://doi.org/10.2147/CIA.S421422
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Zhimeng Wang,* Yao Lu,* Pengfei Wang, Chen Fei, Shuhao Li, Hanzhong Xue, Zhong Li, Qian Wang, Kun Zhang, Teng Ma
Department of Orthopedics and Traumatology, Honghui Hospital, Xi’an Jiaotong University, Xi’an, Shaanxi, 710000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Kun Zhang; Teng Ma, Department of Orthopedics and Traumatology, Honghui Hospital, Xi’an Jiaotong University, No. 555, East Youyi Road, Xi’an, Shaanxi, 710000, People’s Republic of China, Email [email protected]; [email protected]
Introduction: This study aimed to examine the impacts of DOACs compliance and prescribing preferences on clinical outcomes in elderly hip fracture patients with isolated calf deep vein thrombosis (ICDVT).
Methods: We conducted a retrospective cohort study that evaluated 702 patients who underwent surgical treatment combined with ICDVT in an academic university hospital between January 2016 and October 2021. DOACs compliance was investigated through telephone and outpatient follow-up, and ICDVT clinical outcomes were collected 30 and 90 days post-discharge, respectively. Variables of interest were collected through the electronic medical record system, and data were analyzed after adjusting for predictors of non-completely dissolved (CD) of ICDVT.
Results: The DOACs compliance survey revealed that 375 (53.42%) patients were fully adherent, 270 (38.46%) were fairly adherent, and 57 (8.12%) were poorly adherent. Approximately 62% of patients had ICDVT dissipation within 30 days after discharge, reaching 94% within 90 days. DOACs QD/BID regimen is often based on economic status, activity capacity, discharge destination and post-operative weight-bearing activities (p< 0.05).The mechanism of injury, ASA classification, surgical technique and timing of ICDVT formation were significantly correlated with DOACs 14/28 days regimen (p< 0.05).Multivariate analysis revealed that rural patients [OR 1.518 (95% CI, 1.117– 2.236)], pre-operative ICDVT[OR 2.816 (95% CI, 1.862– 4.259)] and thrombus length [OR 1.157 (95% CI, 1.263– 1.821)] were ICDVT risk factors for non-CD. Furthermore, DOACs fair compliance [OR 0.087 (95% CI, 0.042– 0.178)], DOACs full compliance [OR 0.283 (95% CI, 0.139– 0.579)], and hospitalization duration [OR 0.793 (95% CI, 0.694– 0.907)] were ICDVT protective factors for CD.
Conclusion: Better compliance with DOACs benefits early ICDVT dissipation, but final clinical outcomes have to be validated with longer follow-up periods. When managing elderly patients with hip fractures, indications for anticoagulation should be considered and individualized protocols should be used.
Keywords: hip fractures, direct oral anticoagulant, calf deep vein thrombosis, compliance, elderly
Introduction
The treatment of elderly patients with hip fractures has always been a key concern for clinicians. Furthermore, due to the high incidence of comorbidities, elderly patients with hip fractures have high mortality and disability rates, with a reported mortality rate of 1.7–6.9% at 30 days postoperatively and up to 14–36% within 1 year.1–3 Deep vein thrombosis (DVT) in the lower extremity is one of the common complications of hip fractures, due to the significant risks associated with DVT, numerous countries and regions have developed comprehensive guidelines and consensus on the prevention and treatment of this condition, including treatment modalities for different locations of DVT involvement and different orthopedic surgery. Reports also show that in clinical practice, only strict adherence to guidelines can reduce the incidence of fatal pulmonary embolism (PE) and post-thrombotic syndrome (PTS).4–7
The calf vein is one of the most common sites of thrombosis after major orthopedic surgery and is easily overlooked clinically owing to the lack of specific presentation.8,9 Controversy still exists regarding the role of isolated calf deep vein thrombosis (ICDVT). Although most cases of ICDVT gradually resolve with standard anticoagulation therapy, a proportion of the untreated case has a tendency to spread proximally or form the PE.9–13 The high degree of uncertainty regarding the clinical relevance of and risks associated with ICDVT, however, is the reason for the variable diagnostic and therapeutic demands of orthopedic surgeons and the limited clear medical evidence (need for anticoagulants, timing, dose, and duration).14
In actual clinical practice, there is heterogeneity in the risk-benefit analysis of anticoagulation by orthopedic surgeons and anaesthetists in elderly patients with hip fractures combined with ICDVT population, due to the need for anticoagulation, the risk of bleeding, and surgical delay, blood management.15–17 According to some academics, anticoagulation during hospitalization should be managed according to the outcomes of ultrasonography monitoring in order to be safe and effective.18,19 For many patients, the transition from hospital to home is a particularly vulnerable period, and it is unclear whether inadequate guidance from healthcare practitioners during this period leads to reduced compliance with anticoagulation and an increased risk of proximal spread of ICDVT and thrombosis-related adverse events.20,21 In our institution, to circumvent this risk after hospital discharge, it is common to use direct oral anticoagulants (DOACs) as an alternative to other types of anticoagulants post-discharge, driven by cost-effectiveness (reduced monitoring requirements, rapid onset of action, fewer complications) and ease of use for patients (predictable pharmacokinetics and fewer drug and dietary interactions).22
During clinical data collection in a prospective study, we found that orthopedic surgeons prescribing of DOACs post-discharge in the elderly hip fracture combined with ICDVT population varied considerably in terms of dose and duration, and furthermore, there are no studies on the relationship between compliance to post-discharge DOACs and clinical outcomes of ICDVT in this population. Therefore, we conducted a retrospective cohort study with three main objectives: (1) to analyze the potential interference factors when surgeons prescribe different DOACs regimens and the risk factors associated with differences in patient compliance with DOACs; (2) to investigate the adherence to DOACs among elderly patients with hip fractures after discharge and to evaluate the clinical outcomes at 30 and 90 days for ICDVT based on different levels of adherence; and (3) to analyze the correlation between non-complete dissipation (CD) ICDVT and potential risk factors.
Materials and Methods
Patients
This was a retrospective cohort study of elderly patients with hip fracture diagnosed with unilateral ICDVT using duplex ultrasonography (DUS) during hospitalization in the Department of Orthopedics and Traumatology (Level I Trauma Center) at a major university hospital from January 2016 to October 2021. The entire data for this study was obtained from a randomized controlled study conducted in our department and registered in the Chinese Clinical Trials Registry. The research was carried out in accordance with the Declaration of Helsinki’s guiding principles and received approval from the institutional review board of Xi’an Jiao Tong University (No. 201606008), a signed informed consent was obtained from all subjects and/or their legal guardian(s).
The inclusion criteria were hip fracture as presentation, age ≥65 years, time from injury to admission ≤12 hours, acute ICDVT as the initial venous thromboembolic event during hospitalisation and duplex ultrasonography (DUS) of the whole leg as the gold standard for diagnosis. The exclusion criteria were: (1) the initial thromboembolic event involves the proximal veins of the lower extremity, inferior vena cava or contralateral limb; (2) atypical thrombosis or thrombosis in usual sites (eg obsolete thrombosis, pulmonary embolism, splanchnic vein thrombosis, renal vein thrombosis, etc.); (3) inferior vena cava filter implantation; (4) open fracture, pathological fracture, peri-implant or periprosthetic fracture patients; (5) inability to tolerate surgery, or a change in treatment plan; (6) history of recent surgery on any part of the body within 3 months; and (7) death, incomplete medical records or loss of follow-up.
Detection, Treatment, and Regression of ICDVT
All patients included in the study underwent ultrasound examinations performed by a trained sonographer according to a standard protocol, including complete whole-leg ultrasound, the results of doubtful diagnoses were determined jointly by two senior sonographers.23 All participants were given LMWH prophylactic anticoagulation therapy (0.4 mL, qd; Glaxo Smith Kline Tianjin Co., Ltd.) during hospitalization according to the recommendations of the Chinese Guidelines for the Prevention of Major orthopedic Venous Thromboembolism and intermittent compression boots were used as adjuvant therapy, and changed to therapeutic doses (bid regimen) if a positive result was found on lower limb venous ultrasound.24 According to the agreement signed upon admission, the patients underwent IV ultrasound examinations of both lower extremities at the bedside every day during hospitalization and were examined at the outpatient clinic 30 and 90 days post-discharge. DOACs (rivaroxaban or apixaban) were prescribed by the surgeon for voluntary purchase on an outpatient basis after discharge, and the surgeon decision on dosage (qd or bid) and administration (14 days or 28 days).
The criteria for the diagnosis of ICDVT were non-compressed veins, lumen obstruction or filling defects, lack of respiratory vibration above the knee vein segment, and inadequate flow augmentation in the lower leg.25 The ICDVT results were divided into two groups: the completely dissolved (CD) group and the non-completely dissolved (non-CD) group. Complete thrombus elimination during follow-up was defined as the absence of filling defect and complete compressibility recovery in the segment that initially had thrombosis on DUS; non-complete dissolution was defined as proximal propagation, localised propagation in the calf, no change and partial dissolution. Proximal propagation was defined as ICDVT not benefiting from anticoagulation management, cumulative iliac, superficial femoral, femoral and popliteal vein thrombosis; localized propagation in the calf was defined as the extension of a thrombus confined to a calf vein had to be significantly beyond the length of the previous thrombus, extend into a new vein segment (superior, middle or inferior), or involve a new vein within the calf.26
Data Collection
Participant demographic information, medical record data and relevant laboratory test results are collected from both inpatient and outpatient electronic medical records. All data involved in the current study were recorded and followed by three uniformly trained osteopaths. The interest variables of interest were divided into four categories.
Demographic variables included age (years), sex, education, marital disruption (ie, separation, divorce, and being widowed), pensions, body mass index (BMI, kg/m2), smoking, alcoholism, co-morbidities, neurological and psychiatric disorders (eg, dementia, delirium), dyskinesia (eg, post-stroke hemiplegia, myasthenia gravis, Parkinson’s disease, and advanced osteoarthritis, etc.), and mechanism of injury, and recent history of surgery to any part of the body. Mechanisms of injury are divided into two categories: low energy (fall from standing height) and high energy (car accident, fall from height, etc.).
Variables associated with surgery included American Society of Anesthesiologists (ASA; I–II and III–IV) classification, surgical technique (hemiarthroplasty, total hip arthroplasty or internal fixation), length of stay, duration of surgery, intraoperative blood loss, perioperative allogeneic blood transfusion, perioperative major bleeding, and postoperative weight-bearing activities (patients were mobilized with protected weight-bearing as tolerated along with the use of assistive devices, such as walkers or crutches). A drop in hemoglobin concentration of 20 g/L or more within 24 hours, necessitating the transfusion of more than 2 units of red blood cells, were all considered major bleeding.27
The thrombus-related variables included the timing of ICDVT formation (admission, preoperative or postoperative), symptomatic ICDVT, thrombus length on the last ultrasound test, and maximum thrombus diameter. Biochemical parameters associated with thrombus on the day of the last ultrasound diagnosis included hemoglobin concentration (HGB, g/L), red blood cell count (RBC, 109/L), white blood cell count (WBC, 109/L), platelet count (PLT, 109/L), prothrombin time (PT, s), activated partial thromboplastin time (APTT), fibrinogen (FIB, g/L), and D-dimer (mg/L).
Variables associated with follow-up in patients with thrombosis included primary family caregiver (spouse, child, or caregiver), discharge destination (home, rehabilitation center, or community hospital), DOACs compliance, treatment dose (qd regimen or bid regimen) and period (14 days or 28 days).
Study Protocol and Outcome Measures
DOACs compliance was investigated by the three surgeons involved in data collection (medical records and telephone return visit services), and was defined as using DOACs for a cumulative period of 14 days or 28 days after discharge as prescribed (full compliance, Group A), purchase of DOACs as prescribed but administered for a cumulative period of less than 14 days or 28 days (fair compliance, Group B), and never used it after discharge (poor compliance, Group C). The efficacy and safety of DOACs in patients with hip fracture after discharge were evaluated using the following indices: ICDVT clinical outcomes, incidence of out-of-hospital bleeding events, symptomatic venous thrombosis, and petechiae or ecchymosis.
Statistical Analysis
SPSS version 22.0 was used for all statistical analyses (IBM Corp., Armonk, NY, USA). To compare continuous factors between the CD and non-CD groups, Mann–Whitney U or t-tests were used to show continuous variables as mean± standard deviation (SD). Comparations were made using the Chi-square or Fisher’s exact test, as applicable, and discrete variables were shown as frequencies with percentages. In order to identify the independent risk factors between various risk factors, stepwise multiple logistic regression analyses (backward LR) were used on predictors that were significant (p values <0.05 in the single-factor analysis), odds ratios (OR) and 95% confidence intervals (CI) were determined. P values <0.05 were considered to be statistically significant. The final model fitness was evaluated using the Hosmer-Lemeshow test.
Results
Demographics
Figure 1 shows a detailed flow chart of the selection of the study participants. A total of 2317 patients were treated for hip fracture surgery in our department during the survey period, and 702 patients were ultimately included according to the established exclusion criteria. Of these, 236 were male and 466 were female, the mean age of the patients enrolled was 75.59±7.92 years, and the mean BMI was 26.17±3.87 kg/m²; furthermore, 281 patients underwent hemiarthroplasty, 155 patients underwent total hip arthroplasty and 266 patients underwent internal fixation.
 |
Figure 1 Flow chart for the selection of study participants. |
DOACs Regimens and Compliance Survey
Three follow-up surgeons surveyed the participants compliance and obtained details of DOACs prescribed at discharge from the electronic medical records. The prescribers issued 317 prescription orders for rivaroxaban and 385 prescription orders for apixaban. Overall, 397 patients (58.84%) were discharged with the required QD regimen, while 305 patients (41.16%) received the BID regimen; 374 patients (53.28%) were discharged with the requirement to use the prescribed medications sequentially for 14 days, while 328 patients (46.72%) were to receive the medications for 28 days. (Details are shown in Figure 2).
 |
Figure 2 Results of the survey of DOACs prescription orders at the time of discharge. |
Fifty-seven patients (8.12%) never used DOACs after discharge; 270 patients (38.46%) were discharged with the requirement to purchase DOACs as prescribed, without regularly administered the drugs orally for a cumulative period of less than 14 days or 28 days; 375 patients (53.42%) used DOACs for a cumulative period of 14 days or 28 days after discharge as prescribed. Thus, 375 patients were judged to have full compliance with DOACs (group A), 270 patients were judged to have fair compliance (group B), and 57 patients were judged to have poor compliance (group C) (details are shown in Figures 2 and 3).
Clinical Outcomes, Safety and Efficacy of ICDVT with Varying Compliance to DOACs
The clinical outcomes of all patients with ICDVT 30 and 90 days after discharge are shown in Table 1. Complete dissolution was observed in 436 cases (62.11%), partial dissolution in 188 cases (26.78%), no change in 36 cases (5.13%), localised calf propagation in 25 cases (3.56%) and proximal propagation in 17 patients (2.42%) at 30 days. Proximal propagation was observed in 17 patients according to site, including the contralateral or ipsilateral femoral veins (4 case), popliteal vein (13 case). The ICDVT completely resolved in 659 patients (93.87%), partially dissolved in 24 patients (3.42%), was unchanged in 9 patients (1.28%), localised calf propagation in 6 patients (0.85%) and propagation proximally in 4 patients (0.57%) at 90 days. The four patients with proximal propagation included two cases of recurrent venous thromboembolism, one cases of popliteal vein, and one cases of bilateral calf muscle vein thrombosis. Patients with good compliance with DOACs had a higher rate of ICDVT dissipation and no increased risk of out-of-hospital bleeding events; however, there was no additional advantage in reducing the incidence of symptomatic venous thrombosis and petechiae or ecchymosis.
 |
Table 1 ICDVT Clinical Outcomes and Different DOACs Compliance Safety and Efficacy |
Analysis Surgeon Preferences for DOACs Regimen
We found that when surgeons prescribed doses of DOACs (QD or BID regimen) for patients, the following factors were considered pension (p=0.015), movement disorders (p=0.007), recent surgical history (p=0.008), patients long-term caregiver post-discharge (p=0.006), post-discharge destination (p=0.006) and post-operative weight-bearing activities (p<0.001). The results of the subsequent multiple logistic regression analysis showed that, surgeons preferred the QD prescription regimen for patients without a pension [OR 1.471 (95% CI, 1.075–2.013), P=0.016]. The QD regimen was also preferred in the group without pre-injury motor impairment [OR 0.716 (95% CI, 0.515–0.995), P=0.046] and in the group without a recent history of surgery [OR 1.971 (95% CI, 1.067–3.643), P=0.030]. Similar, when patients chose to go home after discharge [OR 0.418 (95% CI, 0.241–0.816), P=0.011] or to a community care centers [OR 0.395 (95% CI, 0.0.181–0.862), P=0.020]. Surgeons were more likely to prescribe a QD regimen when patients were told they could progressively weight-bearing activities after surgical treatment [OR 0.410 (95% CI, 0.299–0.562), P<0.001].Details in Table 2.
 |
Table 2 Results of Multivariate Logistic Regression Analysis of Surgeons DOACs QD Regimen |
In addition, when surgeons considered the duration of use in DOACs prescription (14 or 28 days), there was a stronger relationship with mechanism of injury, discharge destination, Timing of ICDVT formation, ASA classification and surgical technique (P<0.05, respectively). Then, the results of the subsequent multiple logistic regression analysis showed that, the 14 days regimen was preferred by surgeons in the group of mechanism of injury (low energy) and ASA classification (I–II), [OR 0.516 (95% CI, 0.038–0.864), P=0.012] and [OR 1.549 (95% CI, 1.114–2.154), P=0.009]. Patients who underwent total hip arthroplasty had 0.6 times more 14 day regimen than 28 day regimen [OR 0.609 (95% CI, 0.389–0.954), P=0.030].Another interesting finding is that when patients presents with ICDVT at the time of admission, surgeons more frequently prescribe for the 14 days regimen[OR 0.511 (95% CI, 0.310–0.844), P=0.009]. Details in Table 3.
 |
Table 3 Results of Multivariate Logistic Regression Analysis of Surgeons DOACs 14 Days Regimen |
Analysis of Patients Compliance with DOACs
Based on the results of the patient compliance survey, the variables of interest were subjected to ordinal logistic regression analysis and the results are shown below. The hip fractures patients from rural areas were positively associated with poor compliance with DOACs, with 2.273 times more than urban patients. Another important finding was that patients diagnosed with ICDVT on admission and preoperative waiting period were 2.38 and 1.841 times more likely to have poor compliance than those diagnosed with ICDVT in the postoperative period, respectively. Details in Table 4.
 |
Table 4 Results of Ordinal Logistic Regression Analysis of Patient Compliance with DOACs |
Univariate Analysis of Categorical Factors for Non-Complete Dissipation of ICDVT at 30 Days Post-Discharge
Univariate analysis of categorical factors showed significant differences in the 9 items (with p<0.05) with regard to hospitalization duration (days), thrombus length (mm), HGB (g/L), D-dimer (mg/L), habitation region, surgical technique, timing of ICDVT formation, long-term caregiver, DOACs compliance (Table 5 and Table 6). Consequently, we included these 9 factors in the multivariate regression analysis.
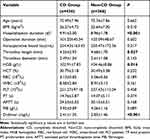 |
Table 5 Continuous Variable Comparison Between Completely Dissolved (CD) and Non-Completely Dissolved (Non-CD) Groups |
 |
Table 6 Categorical Variable Comparison Between Completely Dissolved (CD) and Non-Completely Dissolved (Non-CD) Groups |
Multiple Logistic Regression Analysis
The adjusted data from the multivariate regression analysis are summarized in Table 7. The rural patients, ICDVT formed during preoperative waiting period, and thrombus length (the last ultrasound diagnosis as reference) were associated with a higher risk of incomplete dissolution.
 |
Table 7 Multivariate Analysis of Factors Associated with Non-Completely Dissolved ICDVT |
DOACs full compliance and DOACs fair compliance (poor compliance as reference), and longer hospitalization duration were the protective factors for completely dissolved ICDVT.
Discussion
In this study, which focused on DOACs compliance and prescribing preferences on clinical outcomes in elderly hip fracture patients with ICDVT, several key findings were uncovered. First, patients from rural regions, as well as those who formed ICDVT on admission or preoperatively, demonstrated poor compliance post-discharge. Second, the study found that a majority of patients in the cohort who had ICDVT showed a trend towards dissipation in the first month post-discharge, with nearly 94% dissipated at the three month mark. Third, surgeons take into account a variety of factors when deciding on dosage, such as financial condition, pre-injury exercise capacity, post-discharge destination, long-term caregivers, and post-operative weight-bearing activities. Meanwhile, the duration of DOACs is often influenced by the mechanism of injury, ASA classification, surgical protocol and time to ICDVT formation. These findings highlight the importance of personalized treatment plans that take into account all relevant patient factors. Finally, after adjusting for various confounding variables, the study identified several independent risk and protective factors. Rural patients, those who formed ICDVT during the preoperative waiting period, and those with longer thrombus length had a higher risk of incomplete ICDVT dissolution at 30 days post-discharge. On the other hand, patients who displayed full and fair DOACs compliance and who experienced a longer hospitalization duration were considered independent protective factors for complete dissolution of ICDVT. These findings provide valuable insight into the factors that influence patient outcomes and can help inform future treatment decisions in elderly hip fracture patients with ICDVT.
Currently, the consistent theory holds that ICDVT is more commonly associated with transient risk factors and less often with permanent, irrevocable risk factors; furthermore, the risk of proximal propagation and recurrence is significantly lower than that of proximal DVT.11,12 There is insufficient medical-based evidence to support the need for anticoagulation after discharge, particularly in the population of elderly patients with hip fractures. Although some suggestions or guidelines based on a weak level of evidence recommend surveillance compression ultrasound within two weeks of discharge to detect proximal propagation, few patients and clinicians choose to do so in practice.26,28 Owing to their widespread use and excellent safety profile, DOACs are often used for post-discharge prophylaxis and treatment in this population.22
Previous studies have shown that untreated ICDVT have a tendency for proximal proliferation.12,13 At 1 month post-discharge, the incidence of proximal propagation and localized calf propagation was 24.56% (n=14) in the DOACs poor compliance group, much higher than in the fair compliance group (7.04%, n=19) and full compliance group (2.4%, n=9), with p<0.001.This highlights the importance of patient compliance to medication regimen in preventing the progression of ICDVT. While, the overall dissipation rate at month 3 could be as high as 93.87%, which suggests that patients who develop ICDVT may have a good chance of recovery over time, but that close monitoring and follow-up care are necessary to ensure complete resolution of the condition. Some scholars have argued that with a longer follow-up, all thrombi dissipate completely, regardless of their size or location. Overall, good patient compliance post-discharge in the current study reduced the risk of early propagation of proximal ICDVT; unfortunately, whether patients with non-CD at month 1 follow-up were re-using DOACs was not investigated. Therefore, this part of the data should be interpreted with caution.
Known demographic risk factors for DVT following hip fracture in the Chinese population include older age, female sex, malignancy, underlying disease, previous history of DVT, family history of thromboembolic disease, smoking, BMI, and high D-dimer and fibrinogen.29–32 The complex link between patients DOACs compliance, surgeon prescription order preferences, and clinical outcomes is the focus of current discussions. Elderly people often have various coexisting medical problems, which forces them to concomitantly receive multiple drugs.33,34 The incidence of adverse drug reactions is significantly higher in patients taking over six drugs, and antithrombotic drugs increase the risk of bleeding in patients aged over 75 years.34 The fear of DOAC-associated bleeding and the complexity of DOACs dosing regimens, also based on medical economic considerations in developing countries, may prompt doctors to prescribe inappropriate doses and regimens.35 In some non-orthopedic surgical groups, such as atrial fibrillation and cancer, the use of DOACs is a lengthy process, and the effectiveness and safety of anticoagulants is highly dependent on the patient’s ability to manage and take these complex, high-risk medications.36
Factors affecting adherence are multifaceted and complex. Non-adherence factors may be patient related (lack of literacy, engagement, or participation), physician related (prescribing complex protocols or ineffective communication) or healthcare system related.37 Rural patients are more likely to be candidates for poor adherence and ICDVT non-CD owing to gaps in awareness and information dissemination. In addition, the hierarchical healthcare system in developing countries is still poorly developed, and community or secondary care hospital treatment is inadequate. This deficiency forces approximately 78% of patients included in this study to return home after discharge and self-manage their post-hospital rehabilitation or medication needs.Healthcare professionals play an important role in educating and motivating patients to participate in their treatment plans to ensure maximum adherence to medications. Empowering and motivating patients and involving them in the decision-making process may have far-reaching benefits for patients and the overall healthcare economy as the incidence of symptomatic VTE, fatal PE, and costly hospital admissions is reduced.38,39
Some academics believe that being at high risk of DVT, including complications of cerebrovascular disease, malignancy, long-term immobilization, or orthopedic surgery, requires anticoagulation, whereas asymptomatic calf thrombosis does not require anticoagulation due to its good prognosis.40 Zhao et al suggest the use of individualized treatment, that is, high-risk patients should be given anticoagulation for the same duration as those with proximal DVT, and early physical activity and regular review should be encouraged in low-risk patients to monitor their progression until after at least 6 weeks.12 A study that included 483 patients with calf vein thrombosis, including 399 patients treated with anticoagulation and 84 treated with ultrasound monitoring, showed significantly improved outcomes with anticoagulant treatment without increasing bleeding outcomes.26 A meta-analysis of anticoagulant prolongation regimens, which included a total of 16 studies (24,930 participants), provided moderate-quality evidence for patients undergoing hip surgery to consider the use of prolonged anticoagulation to prevent venous thromboembolism; however, the benefits should be weighed against the increased risk of minor bleeding.41 In a cohort study on the effects of the rouge of administration and dosage on adherence to anticoagulation in patients who underwent hip or knee arthroplasty, it was concluded that patients were more adherent to once-daily oral medication (rivaroxaban) than they were to twice-daily oral medication (apixaban); however, there was no difference in patients’ adherence between once daily regimens of oral or injectable medications (enoxaparin).42 A meta-analysis that compared the treatment effect of QD and those of BID administration of DOACs in patients who underwent major orthopedic surgery, non-valvular atrial fibrillation, venous thromboembolism, and acute coronary syndrome concluded that there was no difference in the incidence of major thrombotic events (RRBID/QD=1.06, 95% CI, 0.86–1.30) or for major bleeding (RRBID/QD=1.02, 95% CI, 0.84–1.23) between the BID and QD regimens, without heterogeneity.43 All these elements highlight the uncertainty about the natural history of ICDVT, its clinical significance and the need for its treatment and modality and duration of treatment.
Although most patients with ICDVT were treated with DOACs, a gap was observed between clinical practice and international guideline recommendations. Non-compliance with guideline recommendations was associated with certain choices, such as the characteristics of ICDVT, duration, and different treatment philosophies of surgeons.44 Since the implementation of systematic whole-leg compression ultrasound in all fracture patients with suspected DVT, there has been an increase in the prevalence of this medical condition.45 This has resulted in significant efforts over the past 10 years to address the question of whether anticoagulants are necessary for its treatment, without reaching a conclusive conclusion but with some significant data on the potential necessity to stratify the risk of extension in patients with distal DVT to help with decision-making. Secondly, whether encouraging early activity reduces the risk of exposing patients to unnecessary anticoagulant therapy and the value of D-dimer use in low-risk populations will be the focus of our subsequent studies.
This study has three main highlights: (i) due to the universality and lack of specific presentation of ICDVT, the prescription management of DOACs by surgeons is not uniform; (ii) surgeons DOACs prescription preferences and patients compliance have a significant impact on the early clinical outcomes of ICDVT; (iii) a multivariable logistic regression analysis revealed that formation of preoperative ICDVT and thrombus length were rare independent risk factor for ICDVT non-CD 1 month post-discharge. This study also has several limitations. First, this was a single-center study and may not be representative of the prevalent population. Secondly, the sample size calculation in our study did not have a sufficient degree of certainty to adequately detect differences in clinical outcomes. Furthermore, the results cannot be applied to the general population since the cost-effectiveness issues arising from the National Essential Medicines List and the inventory policy may prompt inappropriate prescribing of DOACs.
Conclusion
Based on the recommendations of this study findings, surgeons prescribing DOACs should provide effective health education for rural patients and patient groups suffering from ICDVT prior to surgery to improve medication adherence. Their individual needs should also be taken into account to ensure that patients follow the prescribed treatment plan and aim for a satisfactory clinical outcome in a safe and acceptable manner.
Abbreviations
DOACs, Direct oral anticoagulants; ICDVT, Isolated calf deep vein thrombosis; DVT, Deep vein thrombosis; PE, Pulmonary embolism; PTS, post-thrombotic syndrome; DUS, Duplex ultrasonography; ASA, American Society of Anesthesiologists, CD, Completely dissolved; Non-CD, Non-completely dissolved; QD, once daily; BID, Twice daily; FIB, fibrinogen; OR, Odds ratio; CI, Confidence interval.
Data Sharing Statement
Data is available on reasonable request via contacting the corresponding authors (Kun Zhang or Teng Ma).
Acknowledgments
This study was supported by the Social Development Foundation of Shaanxi Province (Grant numbers 2017ZDXM-SF-009, 2019ZDLSF01-09).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Pincus D, Ravi B, Wasserstein D, et al. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318:1994–2003. doi:10.1001/jama.2017.17606
2. Yoo J, Lee JS, Kim S, et al. Length of hospital stay after Hip fracture surgery and 1-year mortality. Osteoporos Int. 2019;30:145–153. doi:10.1007/s00198-018-4747-7
3. Chen X, Wang Z, Liu H, et al. Muscular calf vein thrombosis is associated with increased 30-day mortality but not 90-day mortality in older patients with hip fracture. Am J Cardiol. 2022;184:141–146. doi:10.1016/j.amjcard.2022.08.018
4. Gao Y, Long A, Xie Z, et al. The compliance of thromboprophylaxis affects the risk of venous thromboembolism in patients undergoing Hip fracture surgery. SpringerPlus. 2016;5:1362. doi:10.1186/s40064-016-2724-1
5. Li L, Zhou J, Huang L, et al. Prevention, treatment, and risk factors of deep vein thrombosis in critically ill patients in Zhejiang province, China: a multicenter, prospective, observational study. Ann Med. 2021;53:2234–2245. doi:10.1080/07853890.2021.2005822
6. Stevens SM, Woller SC, Kreuziger LB, et al. Antithrombotic therapy for VTE disease: second update of the CHEST guideline and expert panel report. Chest. 2021;160:e545–e608. doi:10.1016/j.chest.2021.07.055
7. McCormack T, Harrisingh MC, Horner D, Bewley S. Venous thromboembolism in adults: summary of updated NICE guidance on diagnosis, management, and thrombophilia testing. BMJ. 2020;2022:369.
8. Liu XC, Chen XW, Li ZL, Wang SC, Chen C. Anatomical distribution of lower-extremity deep venous thrombosis in patients with acute stroke. J Stroke Cerebrovasc Dis. 2020;29:104866. doi:10.1016/j.jstrokecerebrovasdis.2020.104866
9. Qiu T, Zhang T, Liu L, et al. The anatomic distribution and pulmonary embolism complications of hospital-acquired lower extremity deep venous thrombosis. J Vasc Surg Venous Lymphat Disord. 2021;9:1391–1398.e1393. doi:10.1016/j.jvsv.2021.03.004
10. Elfandi A, Anghel S, Sales C. Current management of isolated soleal and gastrocnemius vein thrombosis. J Vasc Surg Venous Lymphat Disord. 2015;3:341–344. doi:10.1016/j.jvsv.2015.02.002
11. Makedonov I, Galanaud JP, Kahn SR. Significance and management of isolated distal deep vein thrombosis. Curr Opin Hematol. 2021;28:331–338. doi:10.1097/moh.0000000000000670
12. Zhao WG, Yan J-Y, Li X-L, et al. Characteristics and treatment strategy of isolated calf deep venous thrombosis after fractures: a review of recent literature. Orthop Surg. 2022;14:1263–1270. doi:10.1111/os.13292
13. Brewster AC, Jones AE, Johnson SA, Saunders JA, Witt DM. Outcomes of isolated distal thrombosis managed with serial compression ultrasonography. Thromb Res. 2021;208:66–70. doi:10.1016/j.thromres.2021.10.004
14. Palareti G. How I treat isolated distal deep vein thrombosis (IDDVT). Blood. 2014;123:1802–1809. doi:10.1182/blood-2013-10-512616
15. Xia ZN, Xiao K, Zhu W, et al. Risk assessment and management of preoperative venous thromboembolism following femoral neck fracture. J Orthop Surg Res. 2018;13:291. doi:10.1186/s13018-018-0998-4
16. Xu S, Chen JY, Zheng Q, Shi L, Tan AHC. Is chemoprophylaxis required after total knee and total Hip arthroplasty in the Asian population? A systematic review and network meta-analysis. Thromb Res. 2021;198:86–92. doi:10.1016/j.thromres.2020.11.033
17. Griffiths R, Babu S, Dixon P, et al. Guideline for the management of Hip fractures 2020: guideline by the Association of Anaesthetists. Anaesthesia. 2021;76:225–237. doi:10.1111/anae.15291
18. Ktistakis I, Giannoudis V, Giannoudis PV. Anticoagulation therapy and proximal femoral fracture treatment: an update. EFORT Open Rev. 2016;1:310–315. doi:10.1302/2058-5241.1.160034
19. Sugiyama T. Anticoagulant therapy and hip fracture risk: a possible involvement of physical activity. J Am Coll Cardiol. 2020;75:987. doi:10.1016/j.jacc.2019.11.064
20. Chen C, Liu Y, Wu H, et al. The outcome of isolated calf muscle vein thrombosis after open reduction and internal fixation for closed intra-articular distal femur fractures: a prospective cohort study. BMC Musculoskelet Disord. 2021;22:397. doi:10.1186/s12891-021-04289-3
21. Schulman S. Distal deep vein thrombosis--a benign disease? Thromb Res. 2014;134:5–6. doi:10.1016/j.thromres.2014.04.001
22. Rostagno C, Cartei A, Polidori G, et al. Management of ongoing direct anticoagulant treatment in patients with Hip fracture. Sci Rep. 2021;11:9467. doi:10.1038/s41598-021-89077-8
23. Needleman L, Cronan JJ, Lilly MP, et al. Ultrasound for lower extremity deep venous thrombosis: multidisciplinary recommendations from the society of radiologists in ultrasound consensus conference. Circulation. 2018;137:1505–1515. doi:10.1161/circulationaha.117.030687
24. Cui Y, Lu Y, Huang Q, et al. Clinical application effects of different preoperative blood management schemes in older patients with delayed intertrochanteric fracture surgery. Clin Interv Aging. 2022;17:825–835. doi:10.2147/cia.s362020
25. Barrosse-Antle ME, Patel KH, Kramer JA, Baston CM. Point-of-care ultrasound for bedside diagnosis of lower extremity DVT. Chest. 2021;160:1853–1863. doi:10.1016/j.chest.2021.07.010
26. Kuczmik W, Wysokinski WE, Macedo T, et al. Calf vein thrombosis outcomes comparing anticoagulation and serial ultrasound imaging management strategies. Mayo Clin Proc. 2021;96:1184–1192. doi:10.1016/j.mayocp.2021.01.024
27. Shah A, Kerner V, Stanworth SJ, Agarwal S. Major haemorrhage: past, present and future. Anaesthesia. 2023;78:93–104. doi:10.1111/anae.15866
28. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic Therapy for VTE Disease: CHEST guideline and expert panel report. Chest. 2016;149:315–352. doi:10.1016/j.chest.2015.11.026
29. Xing F, Li L, Long Y, Xiang Z. Admission prevalence of deep vein thrombosis in elderly Chinese patients with Hip fracture and a new predictor based on risk factors for thrombosis screening. BMC Musculoskelet Disord. 2018;19:444. doi:10.1186/s12891-018-2371-5
30. Zhang BF, Wei X, Huang H, et al. Deep vein thrombosis in bilateral lower extremities after Hip fracture: a retrospective study of 463 patients. Clin Interv Aging. 2018;13:681–689. doi:10.2147/cia.s161191
31. Zhao K, Wang Z, Tian S, et al. Incidence of and risk factors for pre-operative deep venous thrombosis in geriatric intertrochanteric fracture patients. Int Orthop. 2022;46:351–359. doi:10.1007/s00264-021-05215-x
32. Ding K, Wang H, Jia Y, et al. Incidence and risk factors associated with preoperative deep venous thrombosis in the young and middle-aged patients after Hip fracture. J Orthop Surg Res. 2022;17:15. doi:10.1186/s13018-021-02902-8
33. Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. doi:10.1016/s0140-6736(12)60240-2
34. Arahata M, Asakura H. Antithrombotic therapies for elderly patients: handling problems originating from their comorbidities. Clin Interv Aging. 2018;13:1675–1690. doi:10.2147/cia.s174896
35. Wattanaruengchai P, Nathisuwan S, Rattanavipanon W, et al. Prescriber compliance to direct oral anticoagulant labels and impact on outcomes in Thailand. Br J Clin Pharmacol. 2021;87:1390–1400. doi:10.1111/bcp.14535
36. Pandya EY, Bajorek B. Factors affecting patients’ perception on, and adherence to, anticoagulant therapy: anticipating the role of direct oral anticoagulants. Patient. 2017;10:163–185. doi:10.1007/s40271-016-0180-1
37. Holbrook A, Wang M, Swinton M, et al. Barriers and facilitators for optimizing oral anticoagulant management: perspectives of patients, caregivers, and providers. PLoS One. 2021;16:e0257798. doi:10.1371/journal.pone.0257798
38. Al-Jabi SW, Dalu AA, Koni AA, et al. The relationship between self-efficacy and treatment satisfaction among patients with anticoagulant therapy: a cross-sectional study from a developing country. Thromb J. 2022;20:15. doi:10.1186/s12959-022-00374-2
39. Afzal SK, Hasan SS, Babar ZU. A systematic review of patient-reported outcomes associated with the use of direct-acting oral anticoagulants. Br J Clin Pharmacol. 2019;85:2652–2667. doi:10.1111/bcp.13985
40. Singh K, Yakoub D, Giangola P, et al. Early follow-up and treatment recommendations for isolated calf deep venous thrombosis. J Vasc Surg. 2012;55:136–140. doi:10.1016/j.jvs.2011.07.088
41. Forster R, Stewart M. Anticoagulants (extended duration) for prevention of venous thromboembolism following total Hip or knee replacement or Hip fracture repair. Cochrane Database Syst Rev. 2016;3:Cd004179. doi:10.1002/14651858.CD004179.pub2
42. Moreno JP, Bautista M, Castro J, Bonilla G, Llinás A. Extended thromboprophylaxis for Hip or knee arthroplasty. Does the administration route and dosage regimen affect adherence? A cohort study. Int Orthop. 2020;44:237–243. doi:10.1007/s00264-019-04454-3
43. Mainbourg S, Cucherat M, Provencher S, et al. Twice- or once-daily dosing of direct oral anticoagulants, a systematic review and meta-analysis. Thromb Res. 2021;197:24–32. doi:10.1016/j.thromres.2020.10.011
44. Randelli F, Cimminiello C, Capozzi M, Bosco M, Cerulli G. Real life thromboprophylaxis in orthopedic surgery in Italy. Results of the GIOTTO study. Thromb Res. 2016;137:103–107. doi:10.1016/j.thromres.2015.11.007
45. Markel A. Should preoperative duplex for orthopedic operations be performed? The answer seems to be negative. Thromb Res. 2015;136:841–842. doi:10.1016/j.thromres.2015.08.012
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

