Back to Journals » Clinical Ophthalmology » Volume 13
Subjective Perception Of Trifocal IOL Performance, Including Toric Models
Authors Hamdi IM
Received 13 July 2019
Accepted for publication 13 September 2019
Published 2 October 2019 Volume 2019:13 Pages 1955—1961
DOI https://doi.org/10.2147/OPTH.S223062
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Islam Mahmoud Hamdi1,2
1Ophthalmology Department, Faculty of Medicine, Ain Shams University, Cairo, Egypt; 2Ophthalmology Consultant, The Eye Consultants Center, Jeddah, Saudi Arabia
Correspondence: Islam Mahmoud Hamdi
The Eye Consultants Center, PO Box 15637, Jeddah 21454, Saudi Arabia
Tel +966 12 556888135
Email [email protected]
Purpose: To study the patients’ perception of trifocal IOL (Panoptix™) performance.
Patients and methods: 60 eyes of 35 were implanted with trifocal IOL. Refractive (sphere – S, cylinder – Cyl and spherical equivalent – SE, all in D) and visual (distance uncorrected – VAsc, distance corrected – VAcc, intermediate – IntVA, near uncorrected – NVAsc and distance corrected near – NVAcc, all in LogMAR) results were recorded. Patients were asked about satisfaction (per eye), spectacle independence, near and intermediate activities, distance activities in quantity and quality, finally about personal facial care (per patient). Comparison was made between non-toric (48) and toric models, genders (18 males) and between bilateral (25 patients) and unilateral implantations. Results were correlated to age and IOL power.
Results: With a SE of mean −0.3 ± 0.5 D, cases achieved mean VAsc 0.09 ± 0.1 (∼20/25), VAcc 0.05 ± 0.1 (∼20/22), IntVA 0.05 ± 0.9 (∼20/22), NVAsc 0.05 ± 0.09 (∼̴20/22) and NVAcc 0.04 ± 0.8 (̴∼20/22). Mean level of satisfaction was 85.7 ± 16.5, spectacle independence 96.0 ± 10.6, near activities 95.4 ± 9.8, intermediate activities 97.7 ± 6.4, quantity of distance activities 90.2 ± 10.1, quality of distance activities 88.0 ± 12.1 and facial care 92.6 ± 11.9. All comparisons (non-toric and toric, male and female and bilateral and unilateral implantation) were statistically insignificant (P>0.05). Correlation with age and IOL power was also statistically insignificant (P>0.05).
Conclusion: As perceived by patients, trifocal IOL resulted in very high level of satisfaction. This satisfaction is reflected on diverse visual activities. This level is achieved regardless of gender, IOL model or even unilateral implantation. It is also achieved regardless the age of patients or preoperative eye status.
Keywords: Panoptix, trifocal, toric, subjective
Introduction
The first reports addressed to IOLs treating presbyopia with multifocality, date back to 1987.1 However, it was rapidly noticed the degraded optical qualities of early prototypes.2–4 Various generations were introduced to practice, ending with the current trifocal one.5–9 Extensive concerns were addressed to assess advanced visual and optical functions, naming near and intermediate acuities, contrast sensitivity and glare and halos.10–13 While most of research focus on objective measures,9–14 patients’ perception of IOLs’ performance remains the cornerstone of lens choice.
Trifocal IOL (Panoptix™ – Alcon Laboratories Inc., Fort Worth, TX, USA) has been introduced lately with earliest reports in 2016.15 The lens is a non-apodized diffractive trifocal IOL that distributes light energy to three focal points in both small and large pupil conditions. It uses zeroth, second, and third non-sequential diffraction orders for distance, intermediate, and near foci, respectively, and the energy at the first diffractive order is redistributed to optimize the performance at three other focal points. This novel diffractive structure produces high light utilization, transmitting 88% of light at the simulated 3.0 mm pupil size to the retina. The light is split into two with one half allocated to the distance focus and the other half split between the near and intermediate focus. This IOL is also designed with an intermediary 4.5 mm diffractive zone, making its performance less dependent on pupil size.15 Various reports studied the performance of the lens, whether separately16–20 or in comparison with other lenses.11,21–26 Objective and subjective assessments were included.11,15–26
This study tries to focus on the patient’s perspective, by assessing various visual activities, with respect to fundamental life situations. It is also trying to widen the research, to tackle more specific issues like the performance of the IOL in different situations and with different cases.
Patients And Methods
This is a prospective observational study that included 60 eyes of 35 patient undergoing phacoemulsification with trifocal IOL (Panoptix) implantation, starting January 2016.
Cases were included if they were complaining of visually significant cataract, in one or both eyes, with otherwise normal ocular examination and with no age restriction and chose to be implanted with toric IOL after full explanation of the potential merits and drawbacks of the lens.
Cases were excluded if they had ocular comorbidity, like glaucoma, macular degeneration, corneal scars, etc. Cases were also excluded if they had previous ocular surgeries, except for uneventful corneal laser vision correction procedures.
After complete history taking, all cases were examined to assess visual acuity using ETDRS charts. Objective and subjective refractions were performed, if possible. Anterior segment and ocular surface were examined using slit-lamp biomicroscopy. Patients were then dilated to assess lens condition and examine the posterior segment by funduscopy. After explaining the condition and the required treatment for the patients, they were offered the choice of trifocal IOL, for more spectacle independence.
IOL power was calculated using IOL-master™ (Carl Zeiss, Meditec, Germany). Data retrieved from the calculation, in addition to IOL power, were: keratometry in Diopters for steep and flat meridians, plus cylinder. Axial length was retrieved in mm. IOL calculation formula was chosen depending on the ocular parameters. The choice of power was the first one on the myopic side to achieve emmetropia. For eyes with corneal cylinder <1.25 D, IOL with spherical power only was chosen. For cylinder ≥1.25 D, cases were informed that an additional corneal laser procedure would be needed. No additional measures, e.g. incision at steep meridian, LRI, were taken during phacoemulsification to manage the cylinder. Starting 2018, the same trifocal IOL toric models were used to treat these eyes, with same indications. Moreover, all cases were informed that an additional laser vision correction procedure might be needed, if emmetropia was not achieved for distance,2 months after surgery.
A standard uneventful phaco-emulsification procedure was performed for all cases. IOLs were implanted and centered properly in the capsular bag. Patients received postoperative medications in the form of topical antibiotics (Gatifloxacin 0.5%), corticosteroids (Prednisolone acetate 1%) Qid for 1 month. NSAIDs drops (Ketorolac) were also prescribed, Qid for 2 months, to avoid aggressive capsular healing and maintain lens position. Preservative-free artificial teardrops (carmellose/glycerin combination) was also prescribed Qid, starting week 2, ongoing, to achieve healthy ocular surface.
From the non-toric IOL implanted eyes (48), 3 required an additional laser vision correction procedure to treat residual cylinder.
After complete stability of the eyes, uncorrected and best-corrected visual acuity for distance were assessed. Visual acuity was also assessed for uncorrected intermediate (70 cm) and near (35 cm) distances, to simulate natural daily life activities. Distance corrected near visual acuity was also assessed. Visual acuity was first measured using ETDRS charts using Sloan family of 5×5 letters as optotypes under photopic conditions using room illumination of 85 cd/m2. Measures were then converted into LogMAR for statistical assessment.
Refraction was assessed in term of diopters for final cylinder and spherical equivalent.
All cases were given a questionnaire to rate these conditions:
- General satisfaction and impression about the final result, for each eye.
- Spectacle independence, to assess the frequency of using glasses, for each patient.
- Quality of reading and using mobile phones, to assess near activities, for each patient.
- Quality of using computer screens, to assess intermediate activities, for each patient.
- Quantity of vision at night driving or night outdoor activities to assess distance activities at dim illumination, for each patient.
- Quality of vision at night driving or night outdoor activities to assess symptoms like glare and halos at dim illumination, for each patient.
- Quality of personal care and facial activities (make-up for females and shaving for males), to assess comfort in personal life, for each patient.
(N.B.: for patients who had one eye only operated, they were asked to comment on the implanted eye only.)
Each question was given a score from 0 to 5, 0 being worst and 5 being best. For statistical purpose, grades were converted into percentage 0–100%.
All surgeries were performed in The Eye Consultants Center, Jeddah, by same surgeon (IH)
Study respected the tenets of Declaration of Helsinki. A prior ethical committee approval was obtained. All patients signed a preoperative consent. The questionnaire distributed for patients, included the purpose for data collection.
Statistical analysis :was performed using SPSS software, version 12 (SPSS Inc., Chicago, Illinois). Descriptive analysis was performed by calculating mean ± standard deviation and range for quantitative data. For qualitative data, frequencies were represented by a number and percentage. For parametric values, a between-group comparison was performed with the Student t-test for quantitative data. For non-parametric values, the Mann–Whitney U-test was used for between-group comparison. Correlation was made by Pearson’s test for parametric values and Spearman’s for non-parametric. P < 0.05 was considered statistically significant.
Results
The study included 60 eyes for 35 patients. 25 (62.5%) had bilateral implantation and 10 unilateral (37.5%). 18 (51.4%) were males and 17 (48.6%) were females. Of 60 eyes, 48 (80%) were non-toric and 12 (20%) were toric models. 32 (53.3%) were right eyes and 28 (46.7%) left ones. Mean age of patients was 55.0 ± 11.4 years (24–71). Table 1 presents the ocular parameters and IOL power statistics.
 |
Table 1 Ocular Parameters And IOL Power Statistics |
After a duration of follow up with mean 2.5 + 2.1 (1–9) months, cases were assessed. Only 3 cases required laser vision correction as enhancement after IOL implantation. Table 2 presents the visual and refractive results. Table 3 presents the response of cases to subjective impression about various activities.
 |
Table 2 Post-Operative Refractive And Visual Results |
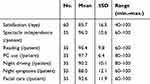 |
Table 3 Subjective Impression (%) |
In an attempt to find any potential difference between cases, comparison for refractive, visual results and subjective impression were made between eyes which were implanted with IOLs with non-toric and toric models (Table 4 and Figure 1). A similar comparison was made between males and females (Table 5 and Figure 2). A last comparison was made between individuals implanted bilaterally and in one eye only (Table 6 and Figure 3). As the sample of cases which required laser correction vision correction enhancement was too small (n=3), this was not compared to those which did not need it. As presented in corresponding tables, both groups, in each comparison, were matched (p >0.05). An exception for that is the eyes implanted with non-toric and toric models had a statistically significant difference (p<0.05) in steep K and corneal cylinder. Males and females’ parameters were matched, except for steep K (p <0.05). Results were statistically non-significant for both groups (p >0.05). There was also no statistical difference in the results between patients implanted bilaterally and in one eye only (p >0.05).
 |
Table 4 Comparison Between Eyes Implanted With Non-Toric And Toric Models (Mean ± SD) |
 |
Table 5 Comparison Between Males And Females (Mean ± SD) |
 |
Table 6 Comparison Between Patients Implanted Bilaterally And In One Eye Only (Mean ± SD) |
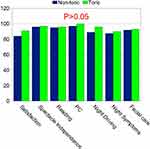 |
Figure 1 Comparison between eyes implanted with non-toric and toric models (P>0.05). |
 |
Figure 2 Comparison between males and females (P>0.05). |
 |
Figure 3 Comparison between patients implanted bilaterally and those implanted unilaterally (P>0.05). |
In an attempt to a better understanding of the lens performance, correlations were made between age and IOL power from one side and visual results and subjective performance form the other side. It was found that IOL performed equally in different ages and with different powers. All correlations were weak (r <0.4) and statistically insignificant (p >0.05) (Table 7).
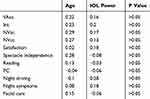 |
Table 7 Correlation Between Age And IOL Power From One Side And Visual Results And Subjective Performance Form The Other Side (r) |
Discussion
This study includes 60 eyes implanted with trifocal IOL, from which 12 were toric models. 10 patients, were implanted unilaterally. To our knowledge, this is the first publication to include toric models from this trifocal IOL. Moreover, unilateral implantation with trifocal IOLs was rarely discussed.20,27,28
Throughout the relatively short duration since the introduction of the lens, it has been sufficiently studied, both objectively and subjectively.11,15–26 In our study, we chose to focus on the subjective aspect and widen its analysis, in order to shed more light on patients’ experience. Objective measures were also taken into consideration. Expected findings were to be linked to objective lens performance to assess their reliability. Still, our objective lens results, nearly matched previous publications.11,15–26
The study chose a quantitative rather than a mere qualitative evaluation for subjective patients’ experience. Specific questions were posed, meant to represent different life situations. Each received an ascending (0 being worst) score out of 5, that was transformed to out of 100, in order to have a more statistical representation. The mean of scores was considered to be more representable than a percentage of patients. Finally, we could express the results per eye, or per patient, correspondingly. Results were all above 85%, some of which (PC use) reached up to 97.7% satisfaction (Table 3).
Comparison with previous studies concerned with the same trifocal IOL would not be effectively achieved.11,16,18,20,21,26 The same was concluded when revised other works not dealing with the current IOL.11,13,14,29–31 There are no standards in methodology-assessing subjective perception for vision after multifocal IOL implantation, not to mention results retrieved from this assessment. Questions vary in number and contents. Most of the studies simply represented the answers in term of percentage of 3–4 levels of satisfaction.10–14,16,29–31 Those which chose to use scoring, used it in a descending manner (0 being the best),18,20,21,26 or ascending (0 being the worst).11 The final score also varied from 4,20 618,21,26 and 10.11
Toric models were introduced at a later stage. To our knowledge, there are no reports till date, about them. For other trifocal IOLs, toric models existed. Results of which were presented, but we could not retrieve a direct comparison between them and non-toric ones. In this study, cases implanted with both models were matched in criteria, except for steep K readings and corneal cylinder (which is logic). They both achieved similar levels of satisfaction.
In view of the earlier lesser results in performance for previous multifocal IOLs generations, differences between individuals were of concern. It was constantly advised to perform the procedure bilaterally. For these reasons, we tried to expand the analysis. Gender differences were compared. There were no differences between males and females. Similar to previous work by Akman et al,20 individuals who received the lens in one eye, perceived performance similar to those who received it bilaterally. Those individuals were either single eyed or the other eye had poor vision for various reasons. They depended on that one, trifocal IOL eye on their activities. For that reason, it could be concluded that a bilateral implantation is not a condition for success with this lens. Neither the age, nor the original status of the eye (as represented by axial length), affected the results in patients.
For the previous analysis, it could be concluded that trifocal IOL could perform efficiently and equally, in a wide range of individuals and conditions, providing that the procedure is completed uneventfully.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Keates RH, Pearce JL, Schneider RT. Clinical results of the multifocal lens. J Cataract Refract Surg. 1987;13:557–560. doi:10.1016/s0886-3350(87)80114-1
2. Nowak MR, Strobel J, Jacobi F. Glare and contrast with diffraction intraocular lenses [article in German]. Fortschr Ophthalmol. 1991;88:125–127.
3. Gimbel HV, Sanders DR, Raanan MG. Visual and refractive results of multifocal intraocular lenses. Ophthalmology. 1991;98:881–887. doi:10.1016/s0161-6420(91)32205-x
4. Wollensak J, Pham DT, Wiemer C. Clinical results after implantation of a multifocal diffractive posterior chamber lens [article in German]. Klin Monbl Augenheilkd. 1991;199:91–95. doi:10.1055/s-2008-1046054
5. Voskresenskaya A, Pozdeyeva N, Pashtaev N, Batkov Y, Treushnicov V, Cherednik V. Initial results of trifocal diffractive IOL implantation. Graefe’s Arch Clin Exp Ophthalmol. 2010;248:1299–1306. doi:10.1007/s00417-010-1424-8
6. Gatinel D, Pagnoulle C, Houbrechts Y, et al. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 2011;37:2060–2067. doi:10.1016/j.jcrs.2011.05.047
7. Lesieur G. Outcomes after implantation of a trifocal diffractive IOL [article in French]. J Fr Ophtalmol. 2012;35:338–342. doi:10.1016/j.jfo.2011.09.012
8. Sheppard AL, Shah S, Bhatt U, et al. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013;39:343–349. doi:10.1016/j.jcrs.2012.09.017
9. Madrid-Costa D, Ruiz-Alcocer J, Ferrer-Blasco T, et al. Optical quality differences between three multifocal intraocular lenses: bifocal low add, bifocal moderate add, and trifocal. J Refract Surg. 2013;29:749–754. doi:10.3928/1081597X-20131021-04
10. Xu Z, Cao D, Chen X, et al. Comparison of clinical performance between trifocal and bifocal intraocular lenses: a meta-analysis. PLoS One. 2017;12:10. doi:10.1371/journal.pone.0186522
11. Cochener B, Boutillier G, Lamard M, et al. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg. 2018;34:507–514. doi:10.3928/1081597X-20180530-02
12. Yoon CH, Shin I, Kim MK. Trifocal versus bifocal diffractive intraocular lens implantation after cataract surgery or refractive lens exchange: a meta-analysis. J Korean Med Sci. 2018;33:44. doi:10.3346/jkms.2018.33.e101
13. Piovella M, Colonval S, Kapp A, et al. Patient outcomes following implantation with a trifocal toric IOL: twelve-month prospective multicentre study. Eye. 2019;33:144–153. doi:10.1038/s41433-018-0076-5
14. Yang Y, Lv H, Wang Y, et al. Clinical outcomes following trifocal diffractive intraocular lens implantation for age-related cataract in China. Clin Ophthalmol. 2018;12:1317–1324. doi:10.2147/OPTH.S169215
15. Lee S, Choi M, Xu Z, et al. Optical bench performance of a novel trifocal intraocular lens compared with a multifocal intraocular lens. Clin Ophthalmol. 2016;10:1031–1038. doi:10.2147/OPTH.S106646
16. García-Pérez JL, Gros-Otero J, Sánchez-Ramos C, et al. Short term visual outcomes of a new trifocal intraocular lens. BMC Ophthalmol. 2017;17:72. doi:10.1186/s12886-017-0462-y
17. Lawless M, Hodge C, Reich J, et al. Visual and refractive outcomes following implantation of a new trifocal intraocular lens. Eye Vis. 2017;4:10. doi:10.1186/s40662-017-0076-8
18. Kohnen T, Herzog M, Hemkeppler E, et al. Visual performance of a quadrifocal (trifocal) intraocular lens following removal of the crystalline lens. Am J Ophthalmol. 2017;184:52–62. doi:10.1016/j.ajo.2017.09.016
19. Shajari M, Kolb CM, Petermann K, et al. Comparison of 9 modern intraocular lens power calculation formulas for a quadrifocal intraocular lens. J Cataract Refract Surg. 2018;44:942–948. doi:10.1016/j.jcrs.2018.05.021
20. Akman A, Asena L, Ozturk C, et al. Evaluation of quality of life after implantation of a new trifocal intraocular lens. J Cataract Refract Surg. 2019;45:130–134. doi:10.1016/j.jcrs.2018.12.003
21. Gundersen KG, Potvin R. Trifocal intraocular lenses: a comparison of the visual performance and quality of vision provided by two different lens designs. Clin Ophthalmol. 2017;11:1081–1087. doi:10.2147/OPTH.S136164
22. Monaco G, Gari M, Di Censo F, et al. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: trifocal versus extended range of vision. J Cataract Refract Surg. 2017;43:737–747. doi:10.1016/j.jcrs.2017.03.037
23. Vilar C, Hida WT, de Medeiros AL, et al. Comparison between bilateral implantation of a trifocal intraocular lens and blended implantation of two bifocal intraocular lenses. Clin Ophthalmol. 2017;11:1393–1397. doi:10.2147/OPTH.S139909
24. Ruiz-Mesa R, Abengózar-Vela A, Ruiz-Santos M. A comparative study of the visual outcomes between a new trifocal and an extended depth of focus intraocular lens. Eur J Ophthalmol. 2018;28:182–187. doi:10.5301/ejo.5001029
25. Mencucci R, Favuzza E, Caporossi O, et al. Comparative analysis of visual outcomes, reading skills, contrast sensitivity, and patient satisfaction with two models of trifocal diffractive intraocular lenses and an extended range of vision intraocular lens. Graefes Arch Clin Exp Ophthalmol. 2018;256:1913–1922. doi:10.1007/s00417-018-4052-3
26. Böhm M, Hemkeppler E, Herzog M, et al. Comparison of a panfocal and trifocal diffractive intraocular lens after femtosecond laser-assisted lens surgery. J Cataract Refract Surg. 2018;44:1454–1462. doi:10.1016/j.jcrs.2018.07.060
27. Brožková M, Filipec M, Filipová L, et al. Outcomes of trifocal toric lens implantation in cataract patients. Cesk Slov Oftalmol. 2016;72:58–64 [article in Czech].
28. Levinger E, Levinger S, Mimouni M, et al. Unilateral refractive lens exchange with a multifocal intraocular lens in emmetropic presbyopic patients. Curr Eye Res. 2019:6. Epub ahead of print.
29. Mencucci R, Favuzza E, Caporossi O, et al. Visual performance, reading ability and patient satisfaction after implantation of a diffractive trifocalintraocular lens. Clin Ophthalmol. 2017;11:1987–1993. doi:10.2147/OPTH.S142860
30. Hovanesian JA. Patient-reported outcomes of multifocal and accommodating intraocular lenses: analysis of 117 patients 2–10 years after surgery. Clin Ophthalmol. 2018;12:2297–2304. doi:10.2147/OPTH.S182943
31. Goldberg DG, Goldberg MH, Shah R, et al. Pseudophakic mini-monovision: high patient satisfaction, reduced spectacle dependence, and low cost. BMC Ophthalmol. 2018;18:293. doi:10.1186/s12886-018-0963-3
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
