Back to Journals » Clinical Ophthalmology » Volume 11
Subjective evaluation of uncorrected vision in patients undergoing cataract surgery with (diffractive) multifocal lenses and monovision
Authors Stock RA , Thumé T , Paese LG , Bonamigo EL
Received 6 March 2017
Accepted for publication 20 June 2017
Published 11 July 2017 Volume 2017:11 Pages 1285—1290
DOI https://doi.org/10.2147/OPTH.S134541
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Ricardo Alexandre Stock, Thaís Thumé, Luan Gabriel Paese, Elcio Luiz Bonamigo
Universidade do Oeste de Santa Catarina, Rua Getúlio Vargas, Joaçaba, Santa Catarina, Brazil
Purpose: To analyze patient satisfaction and difficulties with bilateral multifocal intraocular lenses (IOLs) implantation and aspheric monofocal IOLs implantation using monovision, after cataract surgery.
Materials and methods: A total of 61 participants were included in the study, 29 with monovision and 32 with multifocal lenses. The inclusion criteria were patients undergoing phacoemulsification for bilateral visual impairment due to cataracts and presenting with postoperative visual acuity of 20/30 or better for distance and line J3 or better for near vision.
Results: The 2 groups had similar results regarding difficulties with daily activities such as distance vision, near vision, watching television, reading, cooking, using a computer or cellphone, shaving/putting on makeup and shopping. There were differences in responses between the groups regarding difficulty with night vision (P=0.0565) and night driving (P=0.0291). Degree of satisfaction in terms of distance vision without glasses was statistically significantly better in monovision group (P=0.0332), but not for near (P=0.9101).
Conclusion: Both techniques yielded satisfactory results regarding visual acuity for different activities without the need to use glasses. Multifocal lenses are a good option for patients with the exception of night driving, and who desire independence from glasses.
Keywords: cataract extraction, aphakia, postcataract, patient satisfaction, night vision
Introduction
Cataract surgery is currently considered to be a refractive procedure, as in addition to restoring vision, it provides the patient with greater independence from glasses. Multifocal intraocular lenses (IOLs) represent a major breakthrough in quality of life and visual expectations, especially with regard to independence from glasses. Evaluation studies of patient satisfaction regarding distance and near vision have shown high levels of satisfaction after the implantation of multifocal lenses.1–3 Despite the benefits of corrected visual acuity at multiple distances, multifocal lenses are associated with certain disadvantages, with halos and glares being the most frequent complaints.4 Furthermore, most of these lens modes are not available to all patients due to their high costs.5
Monovision is a technique that became common after the emergence of refractive surgery in which one eye, usually the dominant one, is focused for distance vision and the other for near vision.6 This mode eliminates or significantly reduces dependence on glasses and contact lenses for most daily activities and is slightly better than the multifocal IOLs in terms of intermediate vision. In addition, it costs much less and is a good alternative for some patients. Retrospective studies of monovision have revealed a success rate of 73%.7 However, one concern is the loss of binocularity, which does not commonly occur when using multifocal IOLs.8
Questions regarding the best choice for a particular patient are frequent. AcrySof® ReSTOR® (ALCON, Fort Lauderdale, FL, USA) is a diffractive aspheric multifocal IOL. The diffractive optical structure allocates light to multiple focal points by creating zones, or steps, on the anterior surface of the lens, thus dividing the potency of light between far and near. These steps are responsible for the halos and glares. The AcrySof® IQ (ALCOM) aspheric monofocal IOLs, in contrast, do not create multiple focal points. Thus, the aim of this study was to provide a comparative and subjective analysis of patient satisfaction and the difficulties with AcrySof Restor SN6AD1 bilateral diffractive aspheric multifocal IOLs and AcrySof IQ SN60WF aspheric monofocal IOLs using monovision.
Materials and methods
A mixed qualitative and quantitative field study was conducted with descriptive and analytical objectives for the subjective evaluation of visual function and satisfaction of patients undergoing cataract surgery with bilateral implantation of AcrySof® ReSTOR® SN6AD1 diffractive aspheric multifocal IOLs and the monovision technique with AcrySof IQ SN60WF aspheric monofocal IOLs bilateral. Their impact on daily activities was also examined.
Data were collected using questionnaires containing socioeconomic and specific structured questions that were based on other studies and scored on a Likert scale.1,9 Patients were asked about their level of visual satisfaction for distance and near vision without glasses and after surgery, as well as about their degree of difficulty in performing daily activities.
The study began in September 2013 and ended in March 2015. The questionnaires were administered at the Belotto Stock Ophthalmological Center by a nurse with experience in ophthalmology who guided the patients and answered their questions. All the participants were re-evaluated (refraction, biomicroscopy, uncorrected visual acuity and fundus) before being given the questionnaire in order to verify that the inclusion criteria were met. The purpose of the study and the importance of cooperation were explained to each patient, and they were assured that their confidentiality and anonymity would be maintained. Upon agreement, they signed free and informed consent forms. Parents signed the informed consent in accordance with the participation of the patient under 18 years old.
The survey sample comprised 61 participants, 29 with monovision and 32 with multifocal lenses, and all of the eyes were operated on by the same surgeon. The inclusion criteria were patients undergoing phacoemulsification due to low bilateral visual acuity caused by cataracts and patients who hoped to no longer need or have less of a need for vision correction, both for near and for distance vision. Furthermore, only patients with uncorrected distance visual acuity that was better than or equal to 20/30 and near visual acuity that was better than or equal to J3 were included. For patients with multifocal lenses, the test was performed on 1 eye at a time (monocular visual acuity), and only patients who completed at least 8 months of postoperative follow-up were included. Exclusion criteria were previous eye surgery, only 1 eye, systemic changes that could alter retinal function (diabetes mellitus, autoimmune diseases, and connective tissue diseases), pre-existing eye diseases that could alter visual acuity (herpetic eye disease, moderate or severe dry eye, uveitis, glaucoma, retinal diseases) and visual acuity that was less than that required by the inclusion criteria.
Data were analyzed using descriptive statistics, and the chi-square test was used to examine the associations between the variables. A 5% significance level was adopted. The computational system used was BioEstat 4.0. The research followed the guidelines of the Declaration of Helsinki and was approved by the Research Ethics Committee of the University of the West of Santa Catarina under the number 491.714.
Results
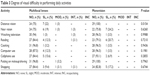
There was a total of 32 (52.45%) patients in the multifocal group and 29 (47.53%) in the monovision group. The socio-demographic characteristics of the 61 evaluated patients (gender, age, education level, profession, civil status and ethnicity) are shown in Table 1.
  | Table 1 Sociodemographic characteristics of the evaluated patients |
Regarding the degree of satisfaction in terms of distance vision without glasses, 75% of the patients using multifocal and 96.5% of monovision lenses reported being “very satisfied” and the difference between the groups was significant (P=0.0332). Regarding near vision without glasses, 78.2% of the patients using multifocal and 78.3% of the monovision were “very satisfied”, and the difference was not significant (P=0.9101) (Table 2).
The 2 groups also exhibited similar results (P>0.05) with regard to the practice of daily activities such as near vision, watching television, reading, cooking, computer use, cellphone use, shaving/putting on makeup and shopping, but not for near vision (P=0.0154) (Table 3).
  | Table 3 Degree of visual difficulty in performing daily activities |
The participants were also asked about difficulties with night vision and night driving, as well as the presence of glares and halos. A total of 24 (75%) participants in the multifocal group and 28 (96.5%) in the monovision group reported no night vision difficulties (P=0.0565). A total of 12 (37.5%) participants in the multifocal group and 25 (86.2%) in the monofocal group reported no night driving difficulties (P=0.0261). A total of 17 (53.1%) participants in the multifocal group and 19 (65.5%) in the monovision group had no complaints regarding glares (P=0.4417) and 19 (59.4%) participants in the multifocal group and 24 (82.7%) in the monovision group had no complaints regarding halos (P=0.1637) (Table 4).
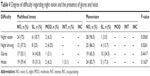  | Table 4 Degree of difficulty regarding night vision and the presence of glares and halos |
Discussion
Contemporary cataract surgery using the phacoemulsification technique not only has the objective of restoring lens transparency but also has a refractive objective, providing good distance and near vision and improving quality of life with independence from glasses.8 Furthermore, a national driver’s license may only be obtained in Brazil when visual acuity is equal to or better than 20/30, and for most near vision activities, a visual acuity of J3 or better allows performance of everyday activities with less difficulty. Our objective with these inclusion criteria was to increase the reliability of the subjective analysis of vision, as including patients with poor vision would defeat the objective of the analysis.
The satisfaction of the study participants with their distance vision was different for both monovision and multifocal lenses (Table 2). In the study by Marques et al,8 all the patients with monovision achieved uncorrected distance visual acuity of 20/40 or better, and in the study of Javitt and Steinert,9 96% of the patients who received multifocal IOLs also achieved 20/40 uncorrected visual acuity. The multifocal group reported a slightly more favorable level of satisfaction with near vision than the monovision group, although the difference was not significant (P=0.6260). In their comparative study of multifocal and monovision IOLs, Zhang et al10 also found that the first is higher than the second but only for intermediate vision, as did Akaishi et al,11 who when analyzing near visual acuity in a multifocal group found that 100% of the participants had near vision visual acuity that was better than or equal to J3.
An evaluation of overall satisfaction regarding the 2 methods revealed no major significant differences, as both achieved good visual function and independence from glasses, except for night vision (P=0.0565), night driving (P=0.0261) and distance vision (P=0.0332). In Akaishi et al’s12 study, multifocal lenses resulted in a mean satisfaction of 8.48 on a scale of 1–10 (1= incapacitating and 10= excellent), and in the study carried out by Marques et al,8 the pseudophakic monovision technique also resulted in a high degree of satisfaction (97.3%).
Regarding the performance of daily activities, 96.5% of the patients in the monovision group and 87.5% of the patients in the multifocal lens group of this study reported no difficulty in using a computer, with no significant differences between the groups (P=0.1981) (Table 3). These data corroborate the results of Zhang et al’s10 study in which 95% of the patients in the multifocal group experienced slight difficulty using computers, whereas the percentage was 74% in the monovision group. This is probably related to the differences in intermediate vision between the 2 lenses. Akaishi et al12 also found that the multifocal lenses provided good distance and near visual acuity and performed slightly worse in middle-distance activities. At the end of 3 months and at a distance of 60 cm, 83% of the patients achieved J3 or better and 35% of the patients achieved J2 or better. In the study carried out by Marques et al,8 which evaluated intermediate vision in monovision, 90% of the patients achieved a visual acuity of J3 or better. However, Chang’s13 study revealed that multifocal lenses provided good distance, intermediate and near vision under photopic and mesopic lighting conditions.
This study revealed no significant advantage of either lens in terms of reading ability. Zhang et al10 found that patients with multifocal IOLs had better near vision, but they still needed reading glasses. In contrast, other studies have revealed the superiority of monovision, wherein the reading ability of patients undergoing this technique increased.14 Various studies of patients with monovision and without glasses have reported excellent visual acuity at different distances, except for night driving in poorly lit environments. However, glasses have usually resolved this problem without the patient experiencing the uncomfortable dysphotopsias afforded by multifocal lenses, which usually interfere with night driving or make it impossible. In this study, none of the patients who underwent the monovision technique had problems with night driving, and 14.28% of those using multifocal lenses experienced slight difficulties (Table 4). Zhang et al10 found that of the 21 patients who underwent the monovision technique, 3 had moderate difficulty with night driving, and of the 22 patients who had received multifocal lenses, 2 reported extreme difficulty.
The presence of photic phenomena in patients with multifocal IOL implantations is already well established. Although the latest models have been designed to minimize this issue, the percentage of patients reporting their presence still remains high. In this study, the presence of halos was predominantly observed with the multifocal lens technique, wherein 37.5% (n=12) reported the presence of slight or moderate halos, while 17.2% of the patients in the monovision group experienced this effect to a slight degree but the difference was not significant (P=0.1637) (Table 4). A recent study found that halos and glares accounted for 10% of the dissatisfaction associated with multifocal lenses.15 Studies involving multifocal IOLs have shown that these visual phenomena are much more common than previously believed. Akaishi et al12 conducted an investigation in which halos and glares were reported by 46% of the patients in the multifocal group and 19% of the patients in the monofocal group. In a study involving 138 patients, Haring et al16 found that 41% of the patients experienced the presence of light phenomena that had not been noticed before cataract surgery and 18% were slightly or moderately affected. Studies involving more patients and a longer follow-up period will provide more significant results.
Conclusion
Based on the results of this study, we can conclude that multifocal IOLs remain a good option for patients who do not do a lot of night driving but who desire better vision and independence from glasses. Monovision can provide distance and near visual acuity that is comparable to multifocal lenses but more favorable with regard to distance vision and causes fewer photic symptoms. It is therefore a good option for patients who drive at night.
Surgeons can use the comparative information provided by this and other studies to provide a less expensive alternative for patients who desire independence from glasses when multifocal lenses cannot be implanted due to the high cost. In addition, this study provides additional data that will enable professionals to recommend the best techniques based on patient profiles, which should result in a higher satisfaction rate.
Neither the implantation of bilateral multifocal IOLs nor the monovision technique is perfect and free of adverse events. However, both have shown satisfactory results and are well suited for patients who desire good visual acuity at different distances without the need to wear glasses.
Acknowledgment
The authors thank Professor Rafael Andre Mergener for statistical analysis.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Santos BWL, Cançado JEP, Ferraz VADS, Campos M. Evaluation of life quality of patients submitted to cataract surgery with implants of monofocal, bifocal and multifocal lenses. Rev Bras Oftalmol. 2014;73(2):86–92. | ||
Gundersen KG, Potvin R. Comparative visual performance with monofocal and multifocal intraocular lenses. Clin Ophthalmol. 2013;7:1979–1985. | ||
Germano JE, Hida WT, Brasil AA, et al. Lente intraocular multifocal refrativa: a performance visual e qualidade de vida em implantes bilaterais versus unilaterais. [Refractive intra-ocular lens: visual performance and quality of life between unilateral versus bilateral]. Rev Bras Oftalmol. 2010;69(6):372–377. | ||
de Vries NE, Webers CA, Montes-Mico R, et al. Long-term follow-up of a multifocal apodized diffractive intraocular lens after cataract surgery. J Cataract Refract Surg. 2008;34(9):1476–1482. | ||
Greenbaum S. Cost–benefit analysis of multifocal IOLs versus monovision pseudophakia. J Cataract Refract Surg. 2009;35(4):614. | ||
Snellingen T, Evans JR, Ravilla T, Foster A. Surgical interventions for age-related cataract. Cochrane Database Syst Rev. 2002;(2):CD001323. | ||
Jain S, Arora I, Azar DT. Success of monovision in presbyopes: review of the literature and potential applications to refractive surgery. Surv Ophthalmol. 1996;40(6):491–499. | ||
Marques FF, Sato RM, Chiacchio BB, Marques DMV, Barreiro J, Caetano RL. Evaluation of visual performance and patient satisfaction with pseudophakic monovision technique. Arq Bras Oftalmol. 2009;72(2):164–168. | ||
Javitt JC, Steinert RF. Cataract extraction with multifocal intraocular lens implantation: a multinational clinical trial evaluating clinical, functional, and quality-of-life outcomes. Ophthalmology. 2000;107(11):2040–2048. | ||
Zhang F, Sugar A, Jacobsen G, Collins M. Visual function and patient satisfaction: comparison between bilateral diffractive multifocal intraocular lenses and monovision pseudophakia. J Cataract Refract Surg. 2011;37(3):446–453. | ||
Akaishi L, Araújo AGRD, Santos RCND, Santos PMD. Acuidade visual em implantes bilaterais de lentes intra-oculares monofocais e multifocais. [Visual acuity of bilateral implants of monofocal and multifocal intraocular lenses]. Arq Bras Oftalmol. 2003;66:199–205. | ||
Akaishi L, Messias CB, Tzelikis PFM. Desempenho visual após implante de uma lente intraocular asférica multifocal difrativa. [Visual performance after implantation of an aspheric multifocal diffractive intraocular lens]. Rev Bras Oftalmol. 2010;69(4):230–235. | ||
Chang DH. Visual acuity and patient satisfaction at varied distances and lighting conditions after implantation of an aspheric diffractive multifocal one-piece intraocular lens. Clin Ophthalmol. 2016;10:1471–1477. | ||
Ito M, Shimizu K. Reading ability with pseudophakic monovision and with refractive multifocal intraocular lenses: comparative study. J Cataract Refract Surg. 2009;35(9):1501–1504. | ||
Gibbons A, Ali TK, Waren DP, Donaldson KE. Causes and correction of dissatisfaction after implantation of presbyopia-correcting intraocular lenses. Clin Ophthalmol. 2016;10:1965–1970. | ||
Haring G, Dick HB, Krummenauer F, Weissmantel U, Kroncke W. Subjective photic phenomena with refractive multifocal and monofocal intraocular lenses. Results of a multicenter questionnaire. J Cataract Refract Surg. 2001;27(2):245–249. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

