Back to Journals » Clinical Ophthalmology » Volume 17
Subconjunctival Sirolimus-Loaded Liposomes for the Treatment of Moderate-to-Severe Dry Eye Disease
Authors Salcedo-Ledesma A , Córdoba A , Zatarain-Barrón NC , Graue-Hernández EO, Garfias Y, Morales Flores N, García-Sánchez GA, García-Santisteban D, Linares-Alba MA, García-Santisteban R , Navas A
Received 24 January 2023
Accepted for publication 20 April 2023
Published 5 May 2023 Volume 2023:17 Pages 1295—1305
DOI https://doi.org/10.2147/OPTH.S405841
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Alfredo Salcedo-Ledesma,1,2 Andrea Córdoba,1 Naomi C Zatarain-Barrón,1 Enrique O Graue-Hernández,1 Yonathan Garfias,3,4 Norma Morales Flores,1 Gustavo A García-Sánchez,5 Diego García-Santisteban,5 Mónica A Linares-Alba,5 Rodrigo García-Santisteban,6 Alejandro Navas1
1Department of Cornea and Refractive Surgery, Institute of Ophthalmology “Conde de Valenciana”, Mexico City, Mexico; 2PECEM MD/PhD Program, Faculty of Medicine, UNAM, Mexico City, Mexico; 3Department of Biochemistry, Faculty of Medicine, UNAM, Mexico City, Mexico; 4Research Unit, Institute of Ophthalmology “Conde de Valenciana”, Mexico City, Mexico; 5Research and Development, Santgar Laboratories, Mexico City, Mexico; 6Faculty of Medicine, Panamerican University, Mexico City, Mexico
Correspondence: Alejandro Navas, Department of Cornea and Refractive Surgery, Institute of Ophthalmology “Conde de Valenciana”, Chimalpopoca 14, Mexico City, 06800, Mexico, Tel +5255 54421700, Fax +5255 55789748, Email [email protected]
Purpose: To determine the effectiveness of subconjunctival application of a novel sirolimus liposomal formulation for the treatment of dry eye.
Methods: A randomized, triple-blind, Phase II clinical trial. Thirty-eight eyes of 19 patients were included. Nine patients (18 eyes) assigned to the sham group (Sham) and 10 patients (20 eyes) to sirolimus-loaded liposomes group (Sirolimus). The treatment group received three doses of subconjunctival liposome-encapsulated sirolimus and the sham group received three doses of liposomal suspension without sirolimus. Subjective (Ocular Surface Disease Index, OSDI) and measured (corrected distance visual acuity, conjunctival hyperemia, tear osmolarity, Schirmer’s test, corneal/conjunctival staining and matrix metalloproteinase-9) variables were measured.
Results: Sirolimus-entrapped liposomes-treated group OSDI scores changed from 62.19 (± 6.07) to 37.8 (± 17.81) (p=0.0024), and conjunctival hyperemia from 2.0 (± 0.68) to 0.83 (± 0.61) (p< 0.0001); Sham group with OSDI scores from 60.02 (± 14.2) to 36.02 (± 20.70) (p=0.01), and conjunctival hyperemia from 1.33 (± 0.68) to 0.94 (± 0.87) (p=0.048). All the other evaluated outcomes only showed significant differences in the sirolimus group: corneal/conjunctival staining score (p=0.0015), lipid layer interferometry (p=0.006), and inferior meibomian gland dropout (p=0.038). No local or systemic adverse effects regarding the medication itself were reported, and the administration route was well accepted.
Conclusion: Our findings suggest that sub-conjunctival sirolimus-loaded liposomes are effective in reducing both signs and symptoms of dry eye in patients with poorly controlled moderate-to-severe DED, while avoiding other topical administration adverse effects. Further investigation with a larger sample size is required to determine long-term effects.
Keywords: sirolimus, rapamycin, liposomes, sirolimus liposomal formulation, dry eye disease
Introduction
Due to its prevalence, dry eye disease (DED) represents a great economic burden to health systems, because of the costs involved derived from pharmacological treatment and physician visits, but also due to its negative effects on quality of life and economical productivity.1
Although there are multiple treatment options available for DED, including topical lubricants, gels, anti-inflammatory drugs, immunomodulators, autologous serum drops, lacrimal plugs, among others;2 the therapeutic options for severe and usually autoimmune-mediated DED are limited.3
As inflammation plays a key role in the ocular surface damage observed in DED,4 most therapies aim to reduce and reduce inflammatory responses.5 Topical corticosteroids and immunomodulators (cyclosporine, tacrolimus, lifitegrast, among others) have demonstrated variable degrees of inflammation reduction and sign/symptom improvement.4,6 However, their use is limited due to their adverse effects; steroids can only be used for short cycles due to the risk of glaucoma and cataract development; and immunomodulators such as cyclosporine and tacrolimus have a good safety profile for prolonged use, but their penetration is limited and they are poorly tolerated by patients, eventually affecting compliance.
Sirolimus (or rapamycin) is a macrolide derived from Streptomyces hygroscopicus that binds to FK506 protein. This union creates a potent immunosuppressive complex that prevents the activation of mammalian target of rapamycin (mTOR), a protein kinase that modulates multiple cellular functions such as lipid and protein synthesis, cellular proliferation, lymphocyte activation, proliferation, and antibody production. Additionally, sirolimus induces autophagy, a process of lysosomal degradation of damaged/aged macromolecules or organelles. Unlike cyclosporine and tacrolimus, this agent does not have an effect on the calcineurin complex, nor does it interfere with the production of IL-2.7–9
Sirolimus has been systemically used for solid organ transplant immunosuppression, autoimmune diseases and certain types of cancer. Systemic administration has been associated with adverse side effects such as stomatitis, nephrotoxicity, and pulmonary toxicity.7,8
Owing to its powerful immunosuppressive effects, local application of sirolimus could potentially play a significant role in the treatment of immune-mediated ocular surface diseases. However, because of its hydrophobic nature, in order to achieve adequate ocular surface penetration, the use of excipients, such as ethanol, polysorbate, and polyethylene glycol, is required. Nevertheless, the use of these agents is linked to potential harm to the ocular surface.7
For this reason, different routes of administration, such as topical, subconjunctival and intravitreal, as well as various delivery methods such as micellar solutions, microspheres and liposomal dispersions, have been evaluated in animal models with the purpose of creating a formulation with high tissue penetration, while also being clinically tolerable and safe in its application. These studies have demonstrated appropriate control of signs and symptoms, increased tear production, and absence of ocular and systemic toxicity.7,10–12
Preclinical, Phase 1, Phase 2 and Phase 3 studies support a recent publication demonstrating sirolimus safety and efficacy for intermediate and posterior uveitis.13 Still, to the best of the authors' knowledge, no studies have been reported for ocular surface diseases in humans.
The present study was performed to determine the effectiveness of subconjunctival sirolimus liposomal formulation for the treatment of signs and symptoms of patients with moderate-to-severe DED.
Materials and Methods
Study Design
This was a randomized, triple-blind, phase II clinical trial. The protocol was approved by the Institutional Review Board (CEI-2019/04/01). This trial was registered obtaining ClinicalTrial.gov Identifier: NCT04115800. Patients between 18 and 70 years old, with moderate-to-severe DED based on an Ocular Surface Disease Index (OSDI) score >22 and a van Bijsterveld score >4 at least in one eye, were invited to participate. Patients with past medical history of refractive surgery, ophthalmic surgery in the last 6 months, facial paralysis, lagophthalmos, herpetic keratitis, recent topical corticosteroids, history of oral isotretinoin in the previous 6 months, pregnant or lactating women, or known allergy or intolerance to sirolimus were excluded. During the study, patients were instructed to continue their current DED treatment, excluding topical corticosteroids, as well as to avoid introducing new medications throughout the trial.
Patient Recruitment
All the medical staff at Institute of Ophthalmology “Conde de Valenciana” were informed of patient eligibility criteria. Candidates had to be referred to Department of Cornea and Refractive Surgery in order to begin enrollment. After complete explanation of the protocol and once they signed the informed consent form, the subjects were enrolled to the assay.
Patient Initial Examination (First Visit)
Ophthalmologic examination and baseline diagnostic studies were performed, including corrected distance visual acuity (CDVA) (LogMAR), OSDI score, conjunctival hyperemia grading (0-++++), tear osmolarity (mOsm/L) (TearLab Corporation, San Diego, California, USA), Schirmer´s test with anesthesia (mm), corneal/conjunctival staining score (van Bijsterveld), intraocular pressure (mmHg), and LacryDiag testing (non-invasive tear break-up time (NITBUT) (seconds), lipid layer interferometry (nm), tear meniscus height (mm), meibomian gland dropout (%) (LacryDiag, Quantel Medical, Cournon-d’Auvergne, France) and detection of Matrix metalloproteinase-9 (MMP-9) protein levels of human tears (InflammaDry, Quidel Corporation, San Diego, CA, USA).
Patient Classification (First Visit)
After concluding initial diagnostic tests, patients were randomized into two different groups using block randomization: Sirolimus liposomal formulation/liposome-loaded sirolimus (Blue) and liposomes without sirolimus/Sham (Green). This color code was used because the vials of liposomal suspension with and without sirolimus were prepared and labeled by only one of the researchers in the laboratory with Good Manufacturing Practice (GMP) resources, using blue labeled vials for those containing sirolimus liposomal formulation and green labels for those containing liposomal suspension without sirolimus. This investigator was not involved in the clinical assay and the analysis until the trial data were opened. All other investigators and participating patients were blinded to the components and preparations.
Initial Treatment (First Visit)
Both sirolimus-loaded suspension and liposomal suspension without sirolimus were prepared with GMP by Laboratorio Santgar Fórmulas Magistrales de México SA de CV, using the Garcia-Sánchez Gustavo A. and Bernad Bernad María J. patented technique described in “IMMUNOSUPPRESSSIVE TREATMENTS FORMULATION AND METHODS” United States Patent Number: 9801862 B2 and World Intellectual Property Organization, International Publication Number: WO 2015/068020 A2. The vials were kept at 2–8°C until dispensed to the patients. Briefly, primary formulation comprises a suspension of approximately 0.4 mg/mL sirolimus encapsulated in soybean lecithin, cholesterol and sucrose liposomes, the aqueous phase comprised in a balanced (pH 7.4) buffer. Treatment was applied as the last step of the first visit, after initial diagnostic studies and patient classification. Subconjunctival injections were applied under topical anesthesia (tetracaine solution 5mg/mL, Ponti Ofteno, Laboratorios Sophia, Mexico). Under the slit-lamp, a 27-gauge syringe was used for injection 60 µg/0.15mL of the indicated suspension in the superior temporal subconjunctival space 4mm away from the corneal limbus. Both eyes of each patient were injected in every visit.
Subsequent Treatment (Second and Third Visits)
Two follow-up visits (second and third visits) were scheduled, each with a 10±2 days interval. In those visits, only the OSDI questionnaires were repeated and patients were inquired about possible adverse effects. At the end of the visit, the second and third doses were applied respectively, using the aforementioned technique.
Post-Treatment Evaluation (Fourth Visit)
At the fourth and last follow-up visit (approximately 4 weeks after baseline/first visit), patients underwent ophthalmologic examination and ancillary studies performed at the baseline examination for comparisons.
Statistical Analysis
Information was collected and recorded in a Microsoft EXCEL 2013 database, where missing, extreme or inconsistent data were identified and adjusted through database verification. Once all the information was verified, descriptive statistics analysis was performed, reporting frequencies and proportions for qualitative variables, along with means, standard deviations, medians, interquartile ranges, statistical dispersions and central tendency measures for continuous variables.
Statistical analysis was performed using Prism 8.3.1 Software. Kolmogorov–Smirnov and Anderson–Darling tests were initially performed to determine data normal distribution. Differences between groups regarding pre- and post-treatment variables were evaluated through X2 tests and non-paired t-tests, whereas intra-group (pre- and post-treatment) differences were assessed using paired t-tests. A p-value less than 0.05 was considered statistically significant.
Ethical Considerations
This trial was reviewed and approved by the Institute of Ophthalmology “Conde de Valenciana” Ethics Committee (CEI-2019/04/01) and was performed following the ethical procedures established by the Declaration of Helsinki. Informed consent included all the data necessary for patients to make an informed decision, and all participating patients signed the informed consent form before inclusion in the study.
Results
A total of 38 eyes of 19 patients were included. Nine patients (18 eyes) assigned to the sham group (Sham) and 10 patients (20 eyes) to sirolimus-loaded liposomes group (Sirolimus). One patient was excluded because of incomplete follow-up, leaving a total of 36 eyes of 18 patients for the final analysis.
All (100%) of the patients of the sirolimus group were female, with a mean age of 55.5±12.2 years and 6 (66.6%) had Sjogren’s syndrome accordingly to the American College of Rheumatology classification criteria. While, of the nine patients of the sham group, 8 (88.8%) were female and 1 (11.11%) was male, with a mean age of 51±10.4 years and 8 (88.8%) presented for Sjogren’s syndrome.
Treatments used by patients previous to enrollment were similar for both groups. All (100%) cases were using artificial tears, 89% were using lubricant ointments and 33.3% immunomodulators (cyclosporine 0.1% solution, Modusik-A Ofteno, Laboratorios Sophia, Mexico). During the whole study time, patients continued their DED treatment and did not introduce new medications different to sirolimus throughout the trial (Table 1).
 |
Table 1 Baseline Characteristics per Study Group |
Both groups had significant symptoms improvement according to the OSDI score, with a change from 62.19 (±6.07) in baseline to (37.8 ± 17.81) in the final visit for sirolimus-loaded liposomes group patients (p=0.0024) and a change from 60.02 (± 14.2) in baseline to 36.02 (± 20.70) in the final visit for the sham group patients (p=0.01). (Figure 1). There were no statistical differences between groups for OSDI improvement (p=0.84).
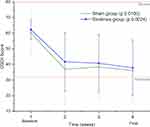 |
Figure 1 Changes in OSDI Score throughout time. |
Conjunctival hyperemia also demonstrated significant improvement in both groups; baseline scores improved from 2.0 (± 0.68) to 0.83 (±0.61) (p<0.0001) in the sirolimus group and from 1.33 (±0.68) to 0.94 (±0.87) (p=0.048) in the control group (Figure 2). There were no statistical differences between groups for conjunctival hyperemia improvement (p=0.66).
 |
Figure 2 Changes in conjunctival hyperemia, comparison between both groups. |
In the sham group, all other evaluated outcomes did not show significant differences, whereas positive and significant changes were observed for corneal/conjunctival staining score (van Bijsterveld) (p=0.0015), lipid layer interferometry (nm) (p=0.006), and inferior meibomian gland dropout (%) (p=0.038) for the group of patients receiving sirolimus liposomal formulation (Table 2 and Figures 3–7).
 |
Table 2 Outcomes According to Study Group |
 |
Figure 3 Corneal/conjunctival staining score (van Bijsterveld), comparison between both groups. |
 |
Figure 4 Lipid layer interferometry (nm), comparison between both groups. |
 |
Figure 5 Inferior Meibomian gland dropout (%), comparison between both groups. |
 |
Figure 6 Interferometry patterns example in the sirolimus-loaded liposomes group. Pre-treatment (left) and post-treatment (right). |
Regarding NITBUT, it increased in both groups from 8.91±0.68 to 9.15±0.97 seconds in the sham group and from 8.68±1.02 to 9.22 seconds in the sirolimus-loaded liposomes group (Figure 8). No statistically significant differences were found. Also, qualitative MMP-9 was similar in both groups before and after treatments. MMP-9 positive results in 88.8% of the eyes (n=16) at baseline, and 100% (n=18) at last visit in the sirolimus group; and MMP-9 positive results in 100% (n=18) at baseline and 83% (n=15) at last visit.
None of the patients showed deterioration of signs or symptoms of DED, nor significant elevation of intraocular pressure (IOP) compared to baseline. Adverse effects were limited to those attributed to the injection, such as mild pain at the application site, as well as self-limited subconjunctival hemorrhages which occurred in two eyes of two patients (one in the sham group and one in the sirolimus group). No systemic adverse effects were reported.
Discussion
DED is very common worldwide and has a major impact on economy and quality of life. Designing new therapies that target different pathways leading to DED signs and symptoms, apart from standard lubricating therapies, seems imperative. Decreasing ocular surface inflammation while augmenting lubrication is a key point in the management of DED.
Our findings suggest that subconjunctival sirolimus liposomal formulation is effective in reducing both signs and symptoms of dry eye in patients with poorly controlled moderate-to-severe DED.
This study demonstrated statistically significant improvement of the OSDI score values (subjective outcome) in both treatment groups, with an average decrease of 24 points. The OSDI has demonstrated to be a valid and reliable tool when discriminating disease severity, but many studies have found that when compared to other objective clinical measures of DED, it does not correlate well.14–16 In this study, the improvement in the OSDI score could be related to the vehicle (liposomal suspension) that is common for both groups, but cannot be related to sirolimus alone, since there were no statistical difference between groups. Our results showed also improvement in OSDI scores, the plausible explanation could be that liposomes have some effect alone in the scores, or injections could generate some subjective repercussions in the sham group. The improvement could also be not related to liposomal suspension application, however confirming this would require including an additional treatment group (placebo group without liposomal suspension), which was not implemented in this study.
Regarding objective clinical differences between groups, both treatment groups showed a significant decrease in conjunctival hyperemia, although significantly more important in sirolimus-loaded liposomes group (p<0.0001). Regarding other clinical signs, improvements were only statistically significant for the sirolimus group, with a substantial reduction in the corneal/conjunctival van Bijsterveld staining score (p=0.0015), increase in tear lipid layer thickness (p=0.006), and decrease in inferior meibomian gland dropout (p=0.038). These findings support sirolimus liposomal formulation potential to reduce ocular surface inflammation, which posteriorly translates into clinically objective improvement.
MMP-9 is a 23 zinc and calcium ion-dependent enzyme important for tissue remodeling in normal physiological processes like wound healing. MMP-9 is also understood to have a pathogenic role in inflammatory diseases.17 MMP-9 applicability in both diagnosis and monitoring treatment response is still debatable in DED.18 Surprisingly, MMP-9 presence in tears was similar in both groups before and after treatments in our study. Perhaps, subconjunctival injections could influence in these findings, due to local inflammation at the injection site.
Other studies have also shown clinically relevant ocular inflammation reduction in humans; one of the most important studies was reported by Nguyen et al, where intravitreal sirolimus was used as treatment for noninfectious intermediate uveitis, posterior uveitis, and panuveitis, finding an important reduction in inflammation, with a positive corticosteroid-sparing effect and no significant increase in IOP.13
Finding valuable alternatives like sirolimus-entrapped liposomes, that could reduce long-term corticosteroid use without significant adverse effects, is particularly relevant in diseases characterized by chronic inflammation as DED.
Strengths of this study include its design characteristics since it is a randomized, triple-blind, phase II clinical trial. Furthermore, the number of variables measured and suitable patient compliance in attending scheduled visits and programmed treatments. Limitations include, small sample size since it was designed as a pilot study, as well as short follow-up; also, this study does not include a placebo group without liposomal suspension application, making it impossible to determine if the outcomes that improved in both groups, such as the OSDI score, can be attributed to the liposomal suspension, the combination liposomes/sirolimus or are due to other uncontrolled factors. Further studies with sirolimus-loaded liposomes that include a larger sample size, a longer period of following, different treatment schemes, dose-escalation and probably additional comparison groups, as well as stratifying groups by disease severity are required to clarify the real effects of sirolimus and its benefits for the treatment of DED.
Conclusions
The addition of a potent immunomodulator like sirolimus in patients with poorly controlled moderate-to-severe DED could be beneficial in improving signs and symptoms of dry eye, with adequate security profile. Subconjunctival route of administration and the use of a liposomal nanocarrier help deliver the molecule effectively, requiring a very low dose, avoiding other topical administration adverse effects, as well as systemic toxicity. Further investigation is required to determine the long-term effects of sirolimus liposomal formulations in aiding signs and symptoms of DED, with a larger sample size that enables a more reliable approximation to the potential therapeutic effects.
Abbreviations
DED, dry eye disease; NITBUT, non-invasive tear break-up time; OSDI, ocular surface disease index; MMP-9, matrix metalloproteinase-9; IOP, intraocular pressure.
Data Sharing Statement
The authors do not plan to share deidentified patient-level data given this data are for an investigational device that has not been approved by any regulatory authorities.
Acknowledgment
Presented in part as a Paper Presentation at The Association for Research in Vision and Ophthalmology Annual Meeting in 2021 and as a Poster Presentation at the American Academy of Ophthalmology Annual Meeting in 2021.
Funding
This work was supported by Laboratorios Santgar, Mexico City, Mexico.
Disclosure
Alfredo Salcedo-Ledesma, Andrea Córdoba, Naomi C. Zatarian-Barron, Enrique O. Graue-Hernandez, Yonathan Garfias, Norma Morales Flores do not have any financial or proprietary interest or relationships to disclose. Gustavo A. García-Sánchez is co-owner of Laboratorios Santgar and has a patent: “IMMUNOSUPPRESSSIVE TREATMENTS FORMULATION AND METHODS” United States Patent Number: 9,801,862 B2 and World Intellectual Property Organization, International Publication Number: WO 2015/068020 A2. Diego García-Santisteban is co-owner of Laboratorios Santgar. Mónica A. Linares-Alba is an employee of Laboratorios Santgar and reports non-financial support from Santgar Laboratory, outside the submitted work. Rodrigo García-Santisteban is co-owner of Laboratorios Santgar. Alejandro Navas does not have any financial or proprietary interest or relationships to disclose.
References
1. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWSII Epidemiology Report. Ocul Surf. 2017;15:334–365. doi:10.1016/j.jtos.2017.05.003
2. Jones L, Downie LE, Korb D, et al. TFOS DEWS II Management and Therapy Report. Ocul Surf. 2017;15:575–628. doi:10.1016/j.jtos.2017.05.006
3. Both T, Dalm VA, van Hagen PM, et al. Reviewing primary Sjögren’s syndrome: beyond the dryness - From pathophysiology to diagnosis and treatment. Int J Med Sci. 2017;14:191–200. doi:10.7150/ijms.17718
4. Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15:438–510. doi:10.1016/j.jtos.2017.05.011
5. Kuklinski E, Asbell PA. Sjogren’s syndrome from the perspective of ophthalmology. Clin Immunol. 2017;182:55–61. doi:10.1016/j.clim.2017.04.017
6. Foulks GN, Forstot SL, Donshik PC, et al. Clinical guidelines for management of dry eye associated with Sjögren disease. Ocul Surf. 2015;13:118–132. doi:10.1016/j.jtos.2014.12.001
7. Shah M, Edman MC, Reddy Janga S, et al. Rapamycin eye drops suppress lacrimal gland inflammation in a murine model of Sjögren’s syndrome. Invest Ophthalmol Vis Sci. 2017;58:372–385. doi:10.1167/iovs.16-19159
8. Zaza G, Granata S, Caletti C, et al. mTOR inhibition role in cellular mechanisms. Transplantation. 2018;102:S3–S16. doi:10.1097/TP.0000000000001806
9. Bertelmann E, Player U. Immunomodulatory therapy in ophthalmology – is there a place for topical application? Ophthalmologica. 2004;218:359–367. doi:10.1159/000080937
10. Wang S, Wang M, Liu Y, et al. Effect of rapamycin microspheres in Sjögren syndrome dry eye: preparation and outcomes. Ocul Immunol Inflamm. 2018;1:1–8. doi:10.1080/09273948.2018.1527369
11. Douglas LC, Yi NY, Davis JL, et al. Ocular toxicity and distribution of subconjunctival and intravitreal rapamycin in horses. J Vet Pharmacol Ther. 2008;31:511–516. doi:10.1111/j.1365-2885.2008.00986.x
12. Linares-Alba MA, Gómez-Guajardo MB, Fonzar JF, et al. Preformulation studies of a liposomal formulation containing sirolimus for the treatment of dry eye disease. J Ocul Pharmacol Ther. 2016;32:11–22. doi:10.1089/jop.2015.0032
13. Nguyen QD, Merrill PT, Sepah YJ, et al. Intravitreal sirolimus for the treatment of noninfectious uveitis: evolution through preclinical and clinical studies. Ophthalmology. 2018;125:1984–1993. doi:10.1016/j.ophtha.2018.06.015
14. Schiffman RM, Christianson MD, Jacobsen G, et al. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000;118(5):615–621. doi:10.1001/archopht.118.5.615
15. Lemp MA. Report of the National Eye Institute/Industry workshop on clinical trials in dry eyes. CLAO J. 1995;21:221–232.
16. Baudouin C, Aragona P, Van Setten G, et al. Diagnosing the severity of dry eye: a clear and practical algorithm. Br J Ophthalmol. 2014;98:1168–1176. doi:10.1136/bjophthalmol-2013-304619
17. Aragona P, Aguennouz M, Rania L, et al. Matrix metalloproteinase 9 and transglutaminase 2 expression at the ocular surface in patients with different forms of dry eye disease. Ophthalmology. 2015;122:62–71. doi:10.1016/j.ophtha.2014.07.048
18. Schargus M, Ivanova S, Kakkassery V, et al. Correlation of tear film osmolarity and 2 different MMP-9 tests with common dry eye test in a cohort of non-dry eye patients. Cornea. 2015;34:739–744. doi:10.1097/ICO.0000000000000449
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


