Back to Journals » Clinical Ophthalmology » Volume 15
Structural Changes in the Optic Disc and Macula Detected by Swept-Source Optical Coherence Tomography After Surgical Intraocular Pressure Reduction in Patients with Open-Angle Glaucoma
Authors Vessani R , Frota T, Shigetomi G, Correa P, Mariottoni EB , Tavares I
Received 28 April 2021
Accepted for publication 27 June 2021
Published 14 July 2021 Volume 2021:15 Pages 3017—3026
DOI https://doi.org/10.2147/OPTH.S317190
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Roberto Vessani, Thalyta Frota, Gabriella Shigetomi, Priscila Correa, Eduardo B Mariottoni, Ivan Tavares
Department of Ophthalmology and Visual Sciences, Paulista School of Medicine, São Paulo Hospital, Federal University of São Paulo, São Paulo, Brazil
Correspondence: Roberto Vessani
Federal University of São Paulo, Rua Pará 222, Apto 92, São Paulo, 01243020, Brazil
Tel +55 1132370707
Email [email protected]
Purpose: To evaluate the magnitude of change in optic disc, peripapillary retinal nerve fiber layer (RNFL) and macular parameters measured by swept-source optical coherence tomography (SS-OCT) in glaucomatous eyes after filtration surgery, and to determine any possible relationship between these measurements and baseline factors.
Patients and Methods: This multicenter, prospective, consecutive observational study included patients with open-angle glaucoma who required glaucoma filtering surgery (surgical group, 29 eyes) and those with stable disease (control group, 25 eyes). Patients from the surgical group underwent measurement of optic disc, peripapillary retinal nerve fiber layer (RNFL) and macular parameters before and after surgery.
Results: In the surgical group, there was a significant increase in rim area and a significant decrease in the linear cup/disc ratio, vertical cup/disc ratio and cup volume 1 and 2 months postoperatively (p< 0.05). No significant change in the mean RNFL thickness and also sectorial measurements were observed from baseline to 1 and 2 months after surgery (p> 0.05). Furthermore, significant increases in macular parameters were observed until 2 months after surgery (p< 0.05). No significant changes were observed for all SS-OCT measurements in the control group. There was a significant correlation between the magnitude of the structural measurements change and the IOP reduction for two topographic parameters (rim area and linear cup-disc ratio) and macular average thickness 1 month and 2 months postoperatively.
Conclusion: In open-angle glaucoma patients submitted to surgical IOP reductions, improvements in topographic and macular OCT parameters measured by SS-OCT were observed for at least 2 months.
Keywords: filtering surgery, intraocular pressure, optic disc, macula, optical coherence tomography
Introduction
Automated perimetry, optic disc photography and objective measurements of the optic disc parameters, peripapillary retinal nerve fiber layer (RNFL) and inner macular layers by optical coherence tomography are part of the initial evaluation and follow-up of patients with glaucoma.1–3
In this disease, the principal proven method of treatment focuses on intraocular pressure (IOP) reduction, which reduces optic nerve damage as assessed by functional (visual field) or structural measures.4 Filtration surgery is a common approach in open-angle glaucoma treatment when disease is not controlled by conservative measures such as medication and laser trabeculoplasty. Surgical IOP reduction may affect measurements of routine tests performed in glaucoma patients, bringing difficulties in the investigation of possible disease progression.5–13 Structural reversibility in the optic disc after glaucoma filtering surgery was demonstrated in children as well as adults by photography and automated imaging instruments.6–10 Previous studies observed changes in ocular posterior segment measured by OCT after surgical reduction of IOP.11–13 Improvements in optic disc parameters such as cup depth, prelaminar tissue, and neuroretinal rim were identified.13–15
Changes in peripapillary RNFL thickness measured by time-domain (TD) OCT after glaucoma surgery have already been suggested by some reports,11,16 but not confirmed by others using spectral-domain OCT (SD-OCT).13,14
There is also evidence of macular thickness increase measured by TD-OCT and SD-OCT associated with IOP reduction after uncomplicated glaucoma filtering surgery.17,18 However, no information is available about how inner macular layers relevant to glaucoma are affected by this intervention or how their changes are related to changes in topographic parameters.
It is important to consider that most studies evaluated structural changes after surgical IOP reduction, with focus on specific areas. Because different imaging platforms and analyses were used in populations with variable characteristics, it is difficult to understand if surgically induced IOP reduction and other baseline factors may have a different impact on optic disc, RNFL, and macular parameters measured by OCT in the same patient.
Therefore, the purpose of the present study was to evaluate the magnitude of change in optic disc, RNFL and macular parameters measured by swept-source optical coherence tomography (SS-OCT) in glaucomatous eyes after filtration surgery and to elucidate any possible relationship between them. In addition, we investigated any association between postoperative changes in these parameters and factors such as IOP change, level of glaucomatous damage and age.
Materials and Methods
This was a multicenter prospective consecutive observational study that included subjects from the Glaucoma Service of the Department of Ophthalmology and Visual Science at Federal University of São Paulo and the Ophthalmology Service at General Hospital of Itapecerica da Serra. This study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Federal University of São Paulo, under the Certificate of Presentation for Ethical Appreciation (CAAE) 61705816.2.1001.5505. Informed consent was obtained from all subjects who agreed to participate.
Patients with primary open-angle glaucoma, exfoliative glaucoma, or pigmentary glaucoma who met the following eligibility criteria were included in this study: presence of glaucomatous optic neuropathy, age between 30 and 80 years, best-corrected visual acuity (BCVA) that is better than 20/40 in the selected eye, refractive error of ≤4 spherical diopters and/or 3 cylindrical diopters, and open-angle as shown by gonioscopy. Patients with any other ocular disease (such as retinal condition, important corneal disease, significant cataract or vitreous opacities) that could affect imaging and visual field results, were excluded. Subjects with systemic diseases such as neurologic conditions (previous history of cerebral vascular accident, neurodegenerative disease, tumor, etc.) that also could affect studied parameters were excluded from this study. Inability to provide informed consent or to undergo the proposed examinations was also an exclusion criterion.
Among the included patients, those with uncontrolled IOP after maximal medical therapy (according to medical criteria) and requiring trabeculectomy with mitomycin C or aqueous drainage device implantation were included in the surgical group and those with a controlled IOP and stable disease were included in the control group.
Subjects were submitted to full ophthalmological exam including evaluation of complete medical history, BCVA, IOP (Goldmann applanation tonometry), slit lamp biomicroscopy and fundoscopy.
Subjects underwent SS-OCT (Deep Range Imaging (DRI) OCT Triton Plus, software version 10.11, Topcon, Tokyo, Japan). This SS-OCT device uses a wavelength-sweeping laser with a center wavelength of 1050 nm and a tuning range of approximately 100 nm. 100,000 A-scans are acquired per second with an 8-µm axial resolution in tissue. Optic disc, peripapillary retinal nerve fiber layer (RNFL) and macular scan protocols were performed.
Measurements of all studied parameters were obtained using the automated segmentation algorithms provided by the commercial software.
The 3D optic disc scan protocol (512 A-scans × 256 B-scans covering a 6×6 mm2 area centered on the optic disc) was used to obtain optic disc topography measurements including rim area (mm2), disc area (mm2), linear cup-to-disc ratio (LCDR), vertical cup-to-disc ratio (VCDR), and cup volume (mm3). Mean and sectorial RNFL measurements (superior, inferior, temporal and nasal) (µm) were obtained from data along a scan circle with a diameter of 3.4 mm. Disc parameters were determined at the reference plane height of 120 mm above the retinal pigment epithelium plane in this version.
A 3D Macular protocol (7 x 7 mm-512 A-scans x 256 B-scans centered on the fovea) was also used for macular measurements. Average macular thickness (µm) and macular segments were calculated: average macular RNFL (mRNFL) thickness; average ganglion cell layer (GCL) plus inner plexiform layer (IPL) thickness (referred to as GCL+); average RNFL plus GCL+ (GCL plus IPL) thickness (referred to as GCL++). Superior and inferior halves of these three parameters were also evaluated.
The DRI-OCT Triton provides a quality scale in the image to indicate the signal strength. Only images with adequate signal strength (quality score >55) were included.
All OCT images were also clinically evaluated by one examiner. Images with artefacts and changes suggesting optic disc edema, hypotony maculopathy, epiretinal membrane and other fundus diseases that could affect the measurements of the optic disc, RNFL and macula were excluded.
Standard Automated Perimetry (SAP) tests (Humphrey Field analyzer, model HFA II −750, Carl Zeiss-Meditec, Dublin, California, EUA) with the Swedish Interactive Threshold Algorithm (SITA) Standard 24–2 were also performed in all included subjects up to 2 months before surgery. All patients were experienced with SAP. An abnormal SAP result was characterized by pattern SD index (PSD) outside the 95% confidence limits or a glaucoma hemifield test classified as outside normal limits.
Filtering surgeries were performed using a standardized technique by experienced glaucoma surgeons. Superior fornix-based trabeculectomy was performed with application of Mitomycin C 0.04% for 2 to 3 minutes. Aqueous drainage device implantation (Ahmed-FP7 or Baerveldt-350 implant) was performed in the superotemporal quadrant. Surgeries were conducted in local or general anesthesia. Patients with significant intra- or postoperative complications were excluded from analysis. Bleb needling was not performed in the included subjects during the period of the study.
Data were obtained from routine clinical assessment and Goldmann IOP measurement at 1 month following surgery. SS-OCT scan protocols were employed following dilation of the eye with tropicamide 1%. Using the same protocols, assessments were repeated in all patients, at 2 months following surgery. The same procedures and interval were applied to the control group.
Statistical analyses were performed using the Statistical Package for the Social Sciences version 27.0 (SPSS Inc., Chicago, IL, USA). Assumption of normality was assessed using descriptive statistics, histograms, normal plots, and skewness and kurtosis coefficients. The independent-samples t test and chi-square test were used to compare the data between the groups. Repeated measures ANOVA models with post hoc tests and Bonferroni correction were performed to compare baseline optic disc, RNFL and macular parameters measurements with the ones obtained after 1 month and after 2 months, in each of the groups. Pearson’s correlation coefficient was used to elucidate the association between changes in structural parameters with variables such as IOP change, visual field MD value and age and also between topographic and macular structural parameters. Changes in IOP and SS-OCT parameters were obtained by subtracting baseline values from the values obtained at the one-month or two-months timepoints. P values ≤ 0.05 were considered to be statistically significant.
Results
In this study, 36 eyes of 36 patients and 30 eyes of 30 patients were included in the surgical and control groups, respectively. Four eyes were excluded because of postoperative complications (corneal edema, hyphema, vitreous opacities, hypotonic maculopathy) that did not allow adequate imaging by SS-OCT. Three patients in the surgical group and 5 patients in the control group did not complete all examinations and were also excluded.
Fifty-four eyes of 54 patients with POAG were included in this analysis (surgical group, 29 eyes; control group, 25 eyes). Twenty-eight eyes included in the surgical group underwent trabeculectomy with MMC and one eye underwent the insertion of a glaucoma drainage device (Ahmed-FP7 valve).
Demographic data are presented in Table 1. Based on Hodapp-Parrish-Anderson criteria, 34%, 24% and 41% of patients presented with early, moderate, and severe glaucomatous damage, respectively, in the surgical group. In this group, the mean (±SD) IOP decreased from 22.5 ± 3.3 mmHg at baseline to 14.4 ± 2.9 mmHg (p < 0.001), and 15.1 ± 3.3 mmHg (p < 0.001) at 1 and 2 months after the procedure, respectively. In the control group, no significant changes were observed in IOP from baseline to 1 and 2 months of follow-up (15.4 ± 3.4, 14.6 ± 3.2 mmHg, 15.7 ± 3.9 mmHg, respectively; p = 0.53).
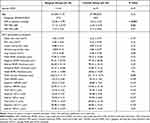 |
Table 1 Baseline Characteristics |
No significant changes were observed in topographic, macular and RNFL parameters in the control group from baseline to 1 month and 2 months of follow-up (p >0.05) (Table 2).
 |
Table 2 SS-OCT Optic Disc, RNFL and Macular Parameters Measurements in the Control Group |
In the surgical group, three topographic SS-OCT parameters changed significantly from baseline to 1 month after the surgery (Table 3). There was an increase in rim area and a decrease in LCDR and VCDR. These changes remained significant after 2 months of surgery. A decrease in cup volume was also observed after 2 months of surgery. No significant changes were observed in optic disc area from baseline to 1 month and 2 months after the surgery (p = 0.95).
 |
Table 3 SS-OCT Optic Disc, RNFL and Macular Parameters Measurements in the Surgical Group |
No significant change in mean peripapillary RNFL thickness and also sectorial measurements were observed after the procedure (Table 3).
The analysis of macular parameters demonstrated a significant increase in total macular thickness and total GCL+ thickness after 1 month as well as 2 months of surgery (Table 3). Significant increases in total GCL++ thickness and superior GCL ++ thickness were also observed after 1 month of surgery, but those changes did not maintain significance after 2 months. Superior GCL+ thickness and inferior GCL+ thickness presented significant increases after 2 months of surgery.
In the surgical group, the effects of IOP reduction on the SS-OCT parameters of the optic disc were also analyzed.
There was a significant correlation between the magnitude of change in each of the four topographic parameters (rim area, LCDR, VCDR and cup volume) and the decrease in IOP after 1 month of surgery, which was not maintained after 2 months.
The decrease in IOP was also correlated with increase in six macular parameters (total macular thickness, total GCL+, superior GCL+, total GCL++, superior GCL++, inferior GCL++), 1 month postoperatively (Table 4). This correlation was also significant after 2 months of surgery for all these parameters, except for superior GCL++.
 |
Table 4 Correlation Between SS-OCT Parameters Change and IOP Change in the Surgical Group |
A significant correlation was observed between changes in rim area and total macular thickness after 1 month of surgery (p = 0.03) (Figure 1A), but not after 2 months (p = 0.9). Furthermore, correlation between changes in rim area and superior GCL+ change after 1 month of surgery (p = 0.03) were noted (Figure 1B). Change in the LCDR was correlated with the superior GCL+ change after 1 month of surgery (p = 0.04) (Figure 1C).
There was no correlation between the visual field MD value at the baseline and the magnitude of change in optic disc and macular OCT parameters after 1 month and after 2 months of surgery (p> 0.05). Similarly, no correlation was observed between age and the magnitude of change in structural parameters (p> 0.05).
Discussion
This prospective study set out to evaluate the effect of uncomplicated glaucoma filtering surgery on SS-OCT parameters from the optic disc, RNFL and macula, provided by the commercial software, in patients with open-angle glaucoma.
With regard to the evaluation of topographic parameters, we observed an increase in the optic disc rim area and a decrease in LCDR, VCDR and cup volume measured by SS-OCT after glaucoma filtering surgery. These results are in agreement with previous reports that showed significant change in different topographic parameters measured by HRT and SD-OCT during a short-term postoperative period.13,19,20 Using HRT, Irak et al. observed a significant increase in the mean rim area and rim volume and a significant decrease in the mean cup-to-disc area ratio and cup volume at least three months after filtering surgery.20
Russo et al. also evaluated optic disc after glaucoma surgery with Spectralis®-SD-OCT (Heidelberg Engineering GmbH, Heidelberg, Germany). Using a separate software, the authors observed a decrease in the maximum and average cup depth at 1 month but not at one year after surgery.19 In a retrospective study, Gietzelt et al.13 measured neuroretinal tissue using the Bruch’s membrane opening minimum rim width (BMO-MRW) and Bruch’s membrane opening minimum rim area (BMO-MRA) before and after trabeculectomy. The authors observed a significant increase in these two parameters until 1 year after trabeculectomy.
It has been suggested that these changes in optic disc parameters are attributable to a decrease in lamina cribrosa (LC) posterior displacement as well as increases in both LC and prelaminar tissue thicknesses in response to glaucoma filtering surgery.21 Changes in SS-OCT measurements of the rim area, linear and vertical cup depths and cup volume in this study are probably consequences of those events.
Previous studies also observed that the optic disc size was decreased following IOP reduction, but the magnitude of decrease detected was of small degree.19,21 In contrast, Reis et al. did not observe significant changes in this parameter based on BMO measurements post-surgery at 1 week, 1 month, 3 months and 6 months. The suggestion that reduction of optic disc size may be associated with the reversal of the LC displacement and improvement of other optic disc parameters is controversial. Because we were not able to detect significant changes in optic disc size after surgery, our study may not support this theory.
Slight but significant macular changes after surgery were also observed in our results. A mean increase of 4 µm in total macular thickness was detected after 1 month of surgery. Similar results were observed by Sesar et al. using Cirrus HD- OCT in 34 eyes with open-angle glaucoma submitted to trabeculectomy.22 Our study also suggests that these slight significant changes in total macular thickness may be maintained at least two months after surgery. Kadziauskienė et al. also observed a significant increase in mean macular thickness and nine subfields defined by the Early Treatment Diabetic Retinopathy Study (ETDRS) in 106 eyes after 1 week of trabeculectomy.18 After six months, macula remained thicker only at the central and inner nasal subfields. In our study, the analysis conducted using the SS-OCT commercial software suggests that parameters of the inner macular layers relevant to glaucoma such as total GCL+ and total GCL++, may increase after surgery. Possible mechanisms that could contribute to the central retinal thickening after trabeculectomy have been discussed. IOP reduction may lead to direct modifications in its inner force on the retina and an indirect effect via sub-scleral deformations transmitted to compliant adjacent intraocular tissues. In addition, changes in the relationship between capillary pressure and interstitial fluid pressure may occur after IOP change.18,22
In this study, we did not observe any significant change in the mean and sectorial RNFL thickness measured by SS-OCT with surgical IOP reduction. This is in agreement with the findings of previous reports that used scanning laser polarimetry, TD-OCT and SD-OCT.13,14,23,24 With SD-OCT, Gietzelt et al.13 did not observe significant changes in mean and sectorial RNFL thicknesses between baseline and follow up at 3, 6 and 12 months after trabeculectomy. By contrast, using a prototype TD-OCT system, Aydin et al. observed a significant increase in the overall mean RNFL thickness as well as in the superior, nasal, and temporal quadrants in patients examined between 6 and 12 months after filtering surgery.11 In their study, patients who underwent combined cataract and glaucoma surgery were included, and it is possible that this could have influenced RNFL measurements positively after the procedure. In addition, differences in the resolution of OCT imaging platforms may affect the reliability of RNFL measurements in longitudinal studies.
A clear correlation between the magnitude of IOP reduction and improvement in different optic disc and macular SS-OCT parameters measurements was observed.
Changes in topographic parameters were significantly correlated with IOP reduction at 1 month after surgery, but this was not observed after 2 months. On the contrary, the relationship between the thickness increase of various macular parameters and IOP change was maintained until 2 months after surgery.
With regard to the evaluation of all SS-OCT structural parameters, the rim area showed the most pronounced change. Mean increases of almost 22% and 16% were observed in this optic disc parameter during follow up at 1 month and 2 months after surgery. By contrast, the mean total macular thickness increased 2% in the same time span. This observation may suggest that, in the same patient, structural improvements that occur in the macula could be subtler than the improvements in the optic disc after surgical IOP reduction. Anatomical differences in the locations of the optic disc and macula partially explain the differences in their susceptibilities to change in accordance with IOP changes. Despite this difference in the magnitude of change, we were able to observe a significant correlation between improvements in topographic parameters and improvement in macular parameters at 1 month after surgery. To the best of our knowledge, no previously published study has investigated this relationship.
It has been suggested that baseline levels of glaucomatous damage may influence certain optic nerve head parameters to change differently after glaucoma filtering surgery. In this study, the surgical group provided adequate representation of patients with early, moderate, and advanced glaucoma. Despite this, we were not able to observe any relationship between the baseline level of glaucomatous damage measured by the MD visual field index and improvements in optic disc parameters measured by SS-OCT. This is in agreement with findings of previous reports measuring different topographic parameters with TD-OCT16 and with SD-OCT.13 By contrast, a previous study with a prototype SS-OCT by Yoshikawa et al. have suggested a correlation between MD visual field index and change in the maximum LC depth measured manually.25 The authors speculate that the susceptibility of LC to IOP changes could not be detectable until glaucoma progression occurs substantially.25 On the contrary, experimental studies have shown that the earlier the stage of glaucoma, the more likely it is that structural changes may occur.26,27
We did not find any relationship between age and changes in optic disc parameters. The mean age of our subjects may be related to these findings. Lee et al. observed that age was a significant factor affecting the decrease in the LC displacement measured by SD-OCT.21 In a population of elderly individuals, Yoshikawa et al. did not observe this association using SS-OCT.25 The age difference between study populations was proposed as an explanation. It is suggested that the mechanical compliance of structural parameters such as LC are thought to decrease with age. In our study, 75% of surgical patients were aged over 60 years.
Similar to optic disc parameters, improvements in macular parameters were not associated with the baseline MD visual field index or age. To our knowledge, there is currently not any published study that evaluated these possible associations.
Conclusion
In conclusion, we observed changes in topographic and macular OCT parameters measured by SS-OCT after surgical IOP reduction, which were maintained for at least 2 months in the same patient. Our results suggest that the impact of IOP reduction is more pronounced in the optic disc than in the macula. These changes may reveal the importance to establish new baseline measurements for those parameters provided by the commercial software after glaucoma filtering procedure for adequate follow-up. The absence of significant change in RNFL parameters in this study may suggest that they are less affected by surgical IOP reduction and are possibly more reliable OCT-based indicators of structural progression in patients with glaucoma.
Acknowledgments
Funded by the Brazilian National Research Council-CAPES PNPD (RMV).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Arnould L, De Lazzer A, Seydou A, et al. Diagnostic ability of spectral-domain optical coherence tomography peripapillary retinal nerve fiber layer thickness to discriminate glaucoma patients from controls in an elderly population (The MONTRACHET study). Acta Ophthalmol. 2020;98(8):e1009–e16.
2. Maupin E, Baudin F, Arnould L, et al. Accuracy of the ISNT rule and its variants for differentiating glaucomatous from normal eyes in a population-based study. Br J Ophthalmol. 2020;104(10):1412–1417. doi:10.1136/bjophthalmol-2019-315554
3. Weinreb RN, Garway-Heath DF, Leung C, et al. Diagnosis of Primary Open Angle Glaucoma. Amsterdam, The Netherlands: Kugler Publications; 2017.
4. Boland MV, Ervin AM, Friedman DS, et al. Comparative effectiveness of treatments for open-angle glaucoma: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158(4):271–279. doi:10.7326/0003-4819-158-4-201302190-00008
5. Wright TM, Goharian I, Gardiner SK, et al. Short-term enhancement of visual field sensitivity in glaucomatous eyes following surgical intraocular pressure reduction. Am J Ophthalmol. 2015;159(2):378–85 e1. doi:10.1016/j.ajo.2014.11.012
6. Quigley HA. Childhood glaucoma: results with trabeculotomy and study of reversible cupping. Ophthalmology. 1982;89(3):219–226. doi:10.1016/S0161-6420(82)34803-4
7. Katz LJ, Spaeth GL, Cantor LB, et al. Reversible optic disk cupping and visual field improvement in adults with glaucoma. Am J Ophthalmol. 1989;107(5):485–492. doi:10.1016/0002-9394(89)90492-3
8. Funk J. Increase of neuroretinal rim area after surgical intraocular pressure reduction. Ophthalmic Surg. 1990;21(8):585–588.
9. Lesk MR, Spaeth GL, Azuara-Blanco A, et al. Reversal of optic disc cupping after glaucoma surgery analyzed with a scanning laser tomograph. Ophthalmology. 1999;106(5):1013–1018. doi:10.1016/S0161-6420(99)00526-6
10. Parrish RK
11. Aydin A, Wollstein G, Price LL, et al. Optical coherence tomography assessment of retinal nerve fiber layer thickness changes after glaucoma surgery. Ophthalmology. 2003;110(8):1506–1511. doi:10.1016/S0161-6420(03)00493-7
12. Lee EJ, Kim TW, Weinreb RN, Kim H. Reversal of lamina cribrosa displacement after intraocular pressure reduction in open-angle glaucoma. Ophthalmology. 2013;120(3):553–559. doi:10.1016/j.ophtha.2012.08.047
13. Gietzelt C, Lemke J, Schaub F, et al. Structural reversal of disc cupping after trabeculectomy alters bruch membrane opening-based parameters to assess neuroretinal rim. Am J Ophthalmol. 2018;194:143–152. doi:10.1016/j.ajo.2018.07.016
14. Waisbourd M, Ahmed OM, Molineaux J, et al. Reversible structural and functional changes after intraocular pressure reduction in patients with glaucoma. Graefes Arch Clin Exp Ophthalmol. 2016;254(6):1159–1166. doi:10.1007/s00417-016-3321-2
15. Reis AS, O’Leary N, Stanfield MJ, et al. Laminar displacement and prelaminar tissue thickness change after glaucoma surgery imaged with optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53(9):5819–5826. doi:10.1167/iovs.12-9924
16. Raghu N, Pandav SS, Kaushik S, et al. Effect of trabeculectomy on RNFL thickness and optic disc parameters using optical coherence tomography. Eye (Lond). 2012;26(8):1131–1137. doi:10.1038/eye.2012.115
17. Karasheva G, Goebel W, Klink T, et al. Changes in macular thickness and depth of anterior chamber in patients after filtration surgery. Graefes Arch Clin Exp Ophthalmol. 2003;241(3):170–175. doi:10.1007/s00417-003-0628-6
18. Kadziauskiene A, Strelkauskaite E, Mockeviciute E, et al. Changes in macular thickness after trabeculectomy with or without adjunctive 5-fluorouracil. Acta Med Litu. 2017;24(2):93–100. doi:10.6001/actamedica.v24i2.3489
19. Russo A, Katsanos A, Riva I, et al. Topographic optic disc changes after successful trabeculectomy evaluated using spectral domain optical coherence tomography. J Ocul Pharmacol Ther. 2013;29(10):870–875. doi:10.1089/jop.2013.0127
20. Irak I, Zangwill L, Garden V, et al. Change in optic disk topography after trabeculectomy. Am J Ophthalmol. 1996;122(5):690–695. doi:10.1016/S0002-9394(14)70488-X
21. Lee EJ, Kim TW, Weinreb RN. Reversal of lamina cribrosa displacement and thickness after trabeculectomy in glaucoma. Ophthalmology. 2012;119(7):1359–1366. doi:10.1016/j.ophtha.2012.01.034
22. Sesar A, Cavar I, Sesar AP, et al. Macular thickness after glaucoma filtration surgery. Coll Antropol. 2013;37(3):841–845.
23. Tavares IM, Melo LA
24. Chang PT, Sekhon N, Budenz DL, et al. Effect of lowering intraocular pressure on optical coherence tomography measurement of peripapillary retinal nerve fiber layer thickness. Ophthalmology. 2007;114(12):2252–2258. doi:10.1016/j.ophtha.2007.02.012
25. Yoshikawa M, Akagi T, Hangai M, et al. Alterations in the neural and connective tissue components of glaucomatous cupping after glaucoma surgery using swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. 2014;55(1):477–484. doi:10.1167/iovs.13-11897
26. Shirakashi M, Nanba K, Iwata K. Changes in reversal of cupping in experimental glaucoma. Longitudinal study. Ophthalmology. 1992;99(7):1104–1110. doi:10.1016/S0161-6420(92)31844-5
27. Coleman AL, Quigley HA, Vitale S, Dunkelberger G. Displacement of the optic nerve head by acute changes in intraocular pressure in monkey eyes. Ophthalmology. 1991;98(1):35–40. doi:10.1016/S0161-6420(91)32345-5
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

