Back to Journals » Psychology Research and Behavior Management » Volume 16
Stigma Experienced by Patients Who Recovered from COVID-19 in Post-Vaccination Period in Thailand; Prevalence and Associated Factors
Authors Techapoonpon K , Kerdchareon N , Polruamngern N, Chalermrungroj T, Srikhamdokkhae O, Matangkarat P
Received 2 July 2023
Accepted for publication 17 August 2023
Published 1 September 2023 Volume 2023:16 Pages 3561—3571
DOI https://doi.org/10.2147/PRBM.S425537
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Kamolvisa Techapoonpon, Nitchawan Kerdchareon, Nongnuch Polruamngern, Teeraphan Chalermrungroj, Orranee Srikhamdokkhae, Premyuda Matangkarat
Department of Psychiatry, Navamindradhiraj University, Vajira Hospital, Bangkok, Thailand
Correspondence: Nitchawan Kerdchareon, Department of Psychiatry, Navamindradhiraj University, Vajira Hospital, 681 Samsen Road, Dusit District, Bangkok, Thailand, 10300, Tel +66 2-244-3187, Email [email protected]
Purpose: Social stigma related to coronavirus disease-2019 (COVID-19) has been a public concern since its emergence, especially in the patients who are reintegrating into their society. However, the insights into COVID-19 stigmatization after vaccine availability are limited. This study aimed to estimate the prevalence, severity and associated factors of stigma experienced by patients who recovered from COVID-19 and reintegrated into their communities. The insights gained from this study are not only beneficial to COVID-19 but can also be used as a background information in future epidemics.
Patients and Methods: This study consisted of two phases. The first phase involved the translation and validation of the COVID-19-related stigma questionnaire. The second phase was a questionnaire-based cross-sectional survey conducted between January and February 2022, at the Vajira Hospital, Bangkok, Thailand. A series of questionnaires regarding stigma, negative emotions (Depression Anxiety Stress Scale-21), and personal information were administered to COVID-19 patients who were already discharged and returned to their communities from June 2021 to February 28, 2022 (N = 354).
Results: The prevalence of stigma among the patients who recovered from COVID-19 was 57.9%. These were classified as mild (28.2%), moderate (21.5%), and severe (8.2%). Pearson’s correlation analysis revealed that longer admissions (r = - 0.151, p = 0.001) and longer duration from discharge (r = - 0.222, p = 0.001) were related to lower stigma. Higher stigma was associated with higher levels of depression (r = 0.528, p < 0.001), anxiety (r = 0.506, p < 0.001) and stress (r = 0.583, p < 0.001).
Conclusion: Social stigma related to COVID-19 in Thailand declined during the post-vaccination period. However, this issue did not disappear, and still took a toll on mental health. Our findings suggested that providing appropriate assessment and help to the patients who recovered from COVID-19 is essential, even in the post-vaccination period.
Keywords: COVID-19, stigma, stigmatization, mental, pandemic, outbreak
Introduction
Since the emergence of the coronavirus disease-2019 (COVID-19), the world has been overwhelmed with fear.1 Stigma has become a public concern, especially in the population who were at risk of contracting the disease.2,3 A meta-analysis published in 2022 calculated that the pool prevalence of COVID-19-related stigma was 35% across all population.3 Among these groups, recovered patients who returned to their communities are one of the most vulnerable groups.4
Stigmatization is conceptualized as a negative social process that is characterized by discrimination, exclusion, rejection, blame or devaluation as a result of an individual’s undesirable characteristics.5 This social issue has been addressed at the forefront by several world class organizations such as the World Health Organization, the United Nations Children’s Fund, and the International Federation of Red Cross and Red Crescent Societies. Stigma has a prominent negative effect on mental health, both short term and long term.6 Adverse psychological consequences caused by COVID-19 stigmatization included anxiety, depression, suicidal behaviour and diminished quality of life.7,8 Moreover, stigmatization causes resistance to enter a treatment system, and therefore might propagate disease transmission.3
The success of the vaccine development against COVID-19 has provided tremendous relief. Community vaccination has significantly reduced stigma.9 However, the stigmatization against COVID-19 was not yet over and should be remained in focus. Owing to the uncertainty of the pandemic, the continuous evolution of new variants and an ongoing report of Long COVID might counterbalance the effects of vaccination and human habituation processes.10,11 Therefore, the magnitude of the stigma problem in the latter phase was difficult to determine. Disparity in stigma levels during the post-vaccination period was also observed. For example, in China, under the COVID Zero approach with strict lockdown, stigmatization in China continues to be apparent. A survey in China found that, although with the vaccine, the nationwide discrimination rate toward patients who recovered from COVID-19 was still high (62.26%).12,13 However, in India, which endorsed a less strict policy, a study concluded that vaccination significantly reduced fear and improved socialization.14
In Thailand, only one study regarding COVID-19-related public stigma was conducted prior to vaccination in 2020.15 Which demonstrated that the prevalence of moderate to high public stigma due to COVID-19 in Thailand was 75.8%. People who used to be quarantined experienced more stigmatization. Therefore, suitable interventions are recommended for vulnerable group. Nevertheless, it is doubtful how stigma has evolved in the post-vaccination period in Thailand, resulting in uncertainty regarding the need to address this problem. The insights gained from this study are not only beneficial to COVID-19 but can also be used as a background information in future outbreak situations. Thus, this study aimed to estimate the prevalence and severity of stigma during the post-vaccination period and to explore the factors associated with stigmatization. The present study was carried out specifically on COVID-19 patients who were discharged from the hospital and reintegrated into their society.
Materials and Methods
The research was approved by Vajira Institutional Review Board (COA 218/2564). This study consisted of two phases. The first phase involved the translation and validation of COVID-19-related stigma questionnaire. The second phase was a cross sectional study that used a series of questionnaires to estimate the level of stigma and stigma-associated factors in patients who recovered from COVID-19.
Phase 1: Questionnaire Translation and Validation
The first step of the translation involved identifying a pre-existing questionnaire of interest. Our criteria for consideration were as follows: 1) questions specifically inquire about stigma resulting from COVID-19, 2) contain both enacted and perceived domains of stigma, 3) available in the English language, 4) validated by an expert committee and a pilot population, 5) has an acceptable level of reliability (indicated by Cronbach’s alpha of at least 0.7, and 6) has an appropriate length (<20 min to complete).16,17 Based on these considerations, a questionnaire developed by Dar et al was eligible.18 This questionnaire was originally adapted from the Ebola-related stigma questionnaire.19 It consists of 15 items on a 4-point Likert scale. The stigma domains included enacted stigma (ES), internalized stigma (IS), perceived external stigma (PES), and disclosure concerns (DC). The COVID-19-related Stigma Questionnaire was used to assess COVID-19 survivors who were discharged from the hospital. In this study, Cronbach’s alpha coefficient was 0.92.
After contacting the author and obtaining permission to translate the pre-existing questionnaire, the following steps were followed: 1) forward translation from English to Thai by two independent translators (a professional translator and a bilingual Thai psychiatrist), 2) discussion and decision making on the best version of each item by three members in our team (two psychologists and one psychiatrist), 3) backward translation from Thai to English and 4) sending the back-translated version to the original author for approval. The backward translated version is listed in Figure 1.
 |
Figure 1 COVID-19-related stigma questionnaire. |
After the translated version was approved, a pilot test of the Thai version was conducted on 10 Thai patients with COVID-19 who were discharged from the hospital. No changes were required to the questionnaire. Content validity was measured using the content validity index (CVI) rated by five experts (three psychiatrists and two psychologists). Each item had CVI > 0.79 and the average CVI of the questionnaire was 0.95.20 Confirmatory factor analysis (CFA) was performed to investigate the factor structure of the questionnaire (Figure 2). The factor loading of every item was greater than the acceptable level of 0.5.21 The reliability measured by the coefficient of Cronbach’s alpha conducted in 300 participants was 0.91. The test-retest reliability measured in 101 sample at 2 weeks interval was 0.743 (p <0.001).22
 |
Figure 2 Confirmatory factor analysis of the four-factor, 15-item of COVID-19-related stigma questionnaire. |
Phase 2: Cross-Sectional Study of the Level of Stigma and Associated Factors in Patients Who Recovered from COVID-19
Participants
The sample size was calculated using a single population proportion formula.23 We listed α = 0.05, Zα/2 = 1.96, d = 0.05 and p = 0.64.24 The calculated sample size was 354.
Our inclusion criteria were as follows: 1) had a positive test for COVID-19, 2) were admitted due to COVID-19 infection and discharged (indication: afebrile and had ≥ 2 negative tests for COVID-19 or reached the recommended quarantine duration) from Vajira Hospital system between June 1, 2021 and February 28, 2022, and 3) were at least 18 years old. The exclusion criteria were refusal to participate and non-fluency in Thai.
Instruments
The questionnaires consisted of three sections. The first part included the personal data (age, sex, education, occupation, income, marital status, number of children, type of house, and underlying medical/psychiatric illness) and admission data (disclosure of infection status, admission setting, frequency of contact with relatives or friends, admission duration and duration from discharge).
The second section was the Thai version of the COVID-19-related stigma questionnaire. It comprised 15 items covering four stigma domains (Figure 1): enacted stigma (ES), disclosure concern (DC), internalized stigma (IS), and perceived external stigma (PES). A 4-point Likert scale was used. Regarding the result interpretation, a higher score indicates a higher stigma level. However, the original study did not provide a classification level. In the present study, we interpreted the total scores based on the K-means cluster analysis as follows: normal (0–5), mild (6–13), moderate (14–24), and severe (>25).25,26
The last section included the Thai version of the Depression Anxiety Stress Scale (DASS-21).27 This self-report questionnaire measures negative emotions including depression, anxiety, and stress. The scale has a total of 21 questions and each emotion has seven questions. The questionnaire has a Cronbach’s alpha coefficient of 0.75. The resulting scores were classified into five levels; normal, mild, moderate, severe and extremely severe. A higher score indicated a more severe condition.
Data Collection
The study protocol was approved by the Vajira Institutional Review Board of the Faculty of Medicine, Vajira Hospital, Navamindradhiraj University (COA 218/2564). All methods were carried out in accordance with the relevant guidelines and regulations and complied with the Helsinki Declaration.
This cross-sectional study was conducted between January and February 2022. Simple random sampling was performed on the list of patients who were admitted and discharged between June 2021 and February 2022. Our research team contacted the discharged patients through a chat application that was originally used during admission. After obtaining written informed consent online, the participants answered the questionnaires by themselves in Google form or via telephone in case of any inconvenience. Participants were asked to provide answers based on their experiences at the time of the survey. No incentives were offered. Participants were anonymized in a case-record form. The authors had no access to the participants’ identification information during or after data collection.
Data Analysis
We used descriptive statistics. Categorical data were presented as frequencies and percentages. Continuous data were summarized and reported as means, standard deviations and ranges. We calculated the correlation of categorical variables using chi-square and Fisher’s exact tests. To investigate the differences in the mean among groups of categorical variables, we used the t-test and analysis of variance (ANOVA). Pearson’ s correlation coefficient was used to determine the relationships between continuous variables. Post-hoc analysis was performed with Turkey’s honest significant difference (HSD) test and Scheffé’s test. K-means cluster analysis was used to classify stigmatization levels. Statistical significance was set at p < 0.05. This analysis used IBM SPSS Statistics version 28 (IBM Corp., Armonk, NY, USA) and STATA 13.
Results
Characteristics of the Participants
A total of 354 recovered patients participated in this study. Table 1 shows the characteristics of the participants and their information regarding admission. Approximately two-thirds (67.2%) of the patients were female. The age of the participants ranged from 18 to 85 years, and the median age was 37 years old. The majority of the respondents disclosed their infection status to non-family acquaintances (78%) and contacted relatives or friends every day (90%). The duration of admission ranged from 3 to 15 days (mean =11 days). Approximately half (49.7%) of the surveys took place more than 3 months after discharge. All the participants had mild-to-moderate symptoms and did not require a ventilator. We did not report the information regarding the admission settings because of its changeability within the hospital system. Most of the participants had normal emotional states. The data showed that 15.25%, 19.2% and 13.84% of the participants experienced at least mild levels of depression, anxiety, and stress respectively.
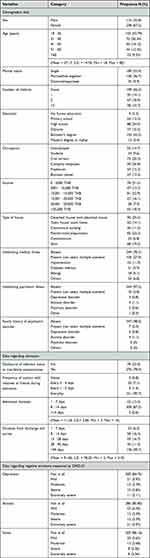 |
Table 1 Characteristic of the Participants (N = 354) |
Level of COVID-19-Related Stigma
Our study found that slightly more than half (57.9%, N=205) of the participants reported some degree of stigma. A major proportion of the patients in this group experienced mild stigmatization (28.2%, N=100). Moderate and severe stigma were found in 21.5% (N=76) and 8.2% (N=29) of the participants, respectively. From the total score of 45, the results ranged from 0 to 45, with the mean score of 24.57 (S.D. = 9.34), indicating moderate stigmatization.
The results for each stigma domain are summarized and reported as score percentages (mean score/full score) and SD: enacted stigma, 50.22% (4.52/9), SD = 2.05, disclosure concern: 51.17% (3.07/6), SD = 1.59, internalized stigma: 42.89% (3.86/9), SD = 1.70 and perceived external stigma: 62.52% (13.13/21), SD = 6.04.
Factors Associated with Overall Stigma
As regards the personal characteristics of the participants, the stigma level was significantly associated with the number of children (p = 0.040), education level (p = 0.036), and income (p = 0.024). No significant difference was found in the post-hoc analysis of each factor on the overall level of stigma level. Regarding the relationship with negative emotions measured by DASS-21, the overall level of stigma was also moderately correlated with stress (r = 0.583, p <0.001), anxiety (r = 0.506, p <0.001) and depression (r = 0.528, p <0.001).
In terms of the factors concerning admission, the correlation analysis revealed a very weak inverse correlation between the overall level of stigma and duration of admission (r = - 0.151, p = 0.001) and a weak inverse correlation with duration from discharge to survey (r = - 0.222, p = 0.001). A similar pattern of relationship was observed between the duration of admission/discharge and negative emotions as measured using the DASS-21 (Table 2).
 |
Table 2 Relationships Between Admission/Recovery Duration and DASS-21/Stigma |
Factors Associated with Each Domain of COVID-19-Related Stigma
One-way ANOVA revealed significant effects of the educational level (F (5, 348) = 2.24, p = 0.044) and number of children (F (3, 350) = 2.63, p = 0.03) on the PES domain. According to the HSD post-hoc test on these two factors, the only significant difference was between having 2 children and having no children (p = 0.029). Participant age was inversely related to the DC domain (r = - 0.175, p = 0.001).
Admission duration was inversely correlated with the DC domain (r = - 0.181, p = 0.001) and PES (r = - 0.149, p = 0.005). The duration between the date of discharge and survey was inversely correlated with all four domains of stigma: ES (r = - 0.183, p = 0.001), DC (r = - 0.178, p = 0.001), IS (r = - 0.122, p = 0.022) and PES (r = - 0.201, p = 0.000).
Discussion
This study confirmed that COVID-19-related stigma exists in the post-vaccination period. During the survey, approximately 70 to 80% of the Thai population had already received 2 doses of vaccines.28 Nevertheless, a downward trend was found compared with previous research before vaccination. We analyzed the tendency of stigmatization in two dimensions: prevalence and severity level. Although no major change was observed in the prevalence of stigmatization, its severity decreased significantly.
In this study, the prevalence of stigma experienced by patients who recovered from COVID-19 was 57.9%. In previous studies, the prevalence ranged from 29.4% to 84.5% in survivor-reported studies and from 45.9% to 64% in public-reported studied.4,11,19–32 Therefore, the value of 57.9% reported in this study still falls within the former range. However, various stigma measurement tools were used in these surveys.
In terms of the change in the stigmatization levels, we analyzed this tendency using three methods. First, we compared our number with the study by Dar et al, which used the original version of the questionnaire.18 The mean stigma score in Dar et al was 28.5, whereas, in this study, the mean score was 24.6. Second, we compared our results with those of a previous study, which classified stigma into levels. Among the survivor-reported studies, only the study by Wahyuhadi et al presented the level of stigma.4 Wahyuhadi et al found that 83.55% of the survivors experienced moderate-to-high stigmatization, whereas, only 29.7% reported moderate-to-high levels of stigma in this study. And third, the comparison was made to studies within Thailand. Since no other study has focused on recovered patients, we compared our results with those of a study conducted by Ruengorn et al which stated that the prevalence of moderate-to-high COVID-19 related public stigma was 75.8%.15 Accordingly, from these three means of comparison, less severe stigmatization was observed.
This study also highlighted the presence of mental health problems related to COVID-19 stigmatization even in the post-vaccination period. Our findings showed that stigma is related to stress, depression, and anxiety. This information is well aligned with previous knowledge regarding stigma and mental health.4,6,28 Stigmatization usually peaks in the initial stage after patients’ return to the community because stigmatized survivors often have to endure an extended period of home isolation, which results in a heightened sense of loneliness, discrimination or guilt.6
Our results indicated that stigma decreased over time after recovery. A longer duration of admission and discharge was associated with a lower level of stigma. However, this effect did not disappear completely. Given that approximately 40% of the survey took place within 1 month after discharge, 50% of the participants experienced stigmatization; therefore, stigma existed beyond 1 month after recovery. This was possibly caused by the image of the infected individuals as having substandard hygiene and therefore were more likely to have re-infection and spread the disease.28 Moreover, COVID-19 in the post-vaccination era remains a stigma because of the growing reports of Long COVID conditions, emergence of new variants, and breakthrough deaths of vaccinated people.29,33,34
In this study, other factors that were associated with stigma included participants’ age, number of children, education, and income. The age of the survivors was inversely related to the DC domain. Elderly people are considered vulnerable because they have a poorer prognosis, and higher rates of hospitalization and death.34 Accordingly, they might not be willing to share their infection status among seniors in the community. The second factor was the number of children of the participants. Post-hoc analysis found that patients who had >1 child tend to have higher stigma than childless ones. Children were also viewed as vulnerable because they lack immunization. During the survey, COVID-19 vaccination for children aged>5 years old had just started.35 Moreover, parents were reluctant to have their children vaccinated.36 Therefore, most children were not vaccinated at the time. The fear of transmission to the children might contribute to stigma. The two remaining factors were the educational level and income. These two variables have been found to be associated with stigma severity in several previous studies.28,30,37 A possible explanation is that the level of education was linked to the level of knowledge about COVID-19.38 People with low knowledge levels about COVID-19 tend to experience more stigma.28,30,39 In contrast, income factor might be related to income reduction from having to isolating themselves if infected.40
Regarding clinical implications, since stigmatization and negative emotions were likely to peak in the initial stage after reintegrating into the community, appropriate assessment and help should be emphasized during this period. Special attention should be paid to the older population, children, and people with a low socioeconomic status. In addition, the findings from this study highlighted the need to tackle the stigma of infectious outbreaks, even after the availability of a vaccine.
Strengths and Limitations
This study is among the first to be conducted solely during the post-vaccination period. Unlike other surveys, we included patients with a wide range of recovery periods. Therefore, this allowed us to examine the relationship between time and stigma.
This study had some limitations. First, this study did not examine the causal relationships between factors and stigma. Second, we did not explore the occurrence of and relationship with the Long COVID condition, which might have confounded the relationship with other factors. Finally, the generalizability might be limited to some extent because the study population was restricted to patients with mild-to-moderate conditions and within the context of Thailand. Therefore, cross-contextual research should be encouraged.41
Conclusion
Social stigma related to COVID-19 still exists and takes a toll on mental health even after the availability of vaccines. Stigma might decrease over time after recovery but does not completely disappear. Our findings suggest providing appropriate assessment and assistance to the patients who have recovered from COVID-19, especially in the initial stage of their reintegration into the community.
Abbreviations
COVID-19, coronavirus disease-2019; ES, enacted stigma; IS, internalized stigma; PES, perceived external stigma; DC, disclosure concerns; CVI, content validity index; DASS-21, Depression Anxiety Stress Scale – 21.
Acknowledgments
We would like to thank all participants for sacrificing their time. We also would like to thank Dr. Somkiat Wattanasirichaikul for supervising this study. This research was funded by the National Research Council of Thailand (grant number N35A650057).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang Y, Shi L, Que J, et al. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol Psychiatry. 2021;26(9):4813–4822. doi:10.1038/s41380-021-01019-y
2. Saeed F, Mihan R, Mousavi SZ, et al. A narrative review of stigma related to infectious disease outbreaks: what can be learned in the face of the COVID-19 pandemic? Front Psychiatry. 2020;11:565919. doi:10.3389/fpsyt.2020.565919
3. Yuan K, Huang X-L, Yan W, et al. A systematic review and meta-analysis on the prevalence of stigma in infectious diseases, including COVID-19: a call to action. Mol Psychiatry. 2021;27(1):19–33. doi:10.1038/s41380-021-01295-8
4. Wahyuhadi J, Efendi F, Al Farabi MJ, et al. Association of stigma with mental health and quality of life among Indonesian covid-19 survivors. PLoS One. 2022;17(2):e0264218. doi:10.1371/journal.pone.0264218
5. Gammon J, Hunt J, Musselwhite C. The stigmatisation of source isolation: a literature review. J Res Nurs. 2019;24(8):677–693. doi:10.1177/1744987119845031
6. Peprah P, Gyasi RM. Stigma and covid‐19 crisis: a wake‐up call. Int J Health Plann Manage. 2020;36(1):215–218. doi:10.1002/hpm.3065
7. Kang EK, Lee SY, Kim MS, et al. The psychological burden of covid-19 stigma: evaluation of the mental health of isolated mild condition covid-19 patients. J Korean Med Sci. 2021;36(3):e33. doi:10.3346/jkms.2021.36.e33
8. Shoib S, Chandradasa M, Saeed F, et al. Suicide, stigma and covid-19: a call for action from low and middle income countries. Front Psychiatry. 2022;13:894524. doi:10.3389/fpsyt.2022.894524
9. World Health Organization. Community vaccinations help overcome stigma and practical barriers. World Health Organization; 2021. Available from: https://www.who.int/philippines/news/feature-stories/detail/philippines-community-vaccinations-help-overcome-stigma-and-practical-barriers.
10. Byrne EA. Understanding long covid: nosology, social attitudes and stigma. Brain Behav Immun. 2022;99:17–24. doi:10.1016/j.bbi.2021.09.012
11. Kurita K, Katafuchi Y, Managi S. Covid-19, stigma, and habituation: evidence from mobility data. BMC Public Health. 2023;23(1):1–7. doi:10.1186/s12889-023-14980-w
12. Li L, Wang J, Leng A, Nicholas S, Maitland E, Liu R. Will covid-19 vaccinations end discrimination against COVID-19 patients in China? New evidence on recovered COVID-19 patients. Vaccines. 2021;9(5):490. doi:10.3390/vaccines9050490
13. Bloomberg. Covid stigma in China can cost recovered patients jobs, homes. Bloomberg; 2022. Available from: https://www.bloomberg.com/news/articles/2022-08-07/covid-stigma-in-china-can-cost-recovered-patients-jobs-homes.
14. Arce FP, Angrisani M, Bennett D, Darling J, Kapteyn A, Thomas K. COVID-19 vaccines and mental distress. PLoS One. 2021;16(9):e0256406. doi:10.1371/journal.pone.0256406
15. Ruengorn C, Awiphan R, Phosuya C, et al. Disparities and factors associated with coronavirus disease-2019-related public stigma: a cross-sectional study in Thailand. Int J Environ Res Public Health. 2022;19(11):6436. doi:10.3390/ijerph19116436
16. Tsang S, Royse CF, Terkawi AS. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J Anaesth. 2017;11(5):80. doi:10.4103/sja.SJA_203_17
17. Revilla M, Ochoa C. Ideal and maximum length for a web survey. Int J Mark Res. 2017;59(5):557–566.
18. Dar SA, Khurshid SQ, Wani ZA, et al. Stigma in coronavirus disease −19 survivors in Kashmir, India: a cross-sectional exploratory study. PLoS One. 2020;15(12):e0244715. doi:10.1371/journal.pone.0244715
19. Overholt L, Wohl DA, Fischer WA, et al. Stigma and Ebola survivorship in Liberia: results from a longitudinal cohort study. PLoS One. 2018;13(11):e0206595. doi:10.1371/journal.pone.0206595
20. Rubio DM, Berg-Weger M, Tebb SS, Lee ES, Rauch S. Objectifying content validity: conducting a content validity study in social work research. Soc Work Res. 2003;27(2):94–104. doi:10.1093/swr/27.2.94
21. Awang Z, Afthanorhan A, Mamat M. The Likert scale analysis using parametric based Structural Equation Modeling (SEM). Comput Methods Soc Sci. 2016;4(1):13–21.
22. Kennedy I. Sample size determination in test-retest and Cronbach alpha reliability estimates. Br J Contemp Educ. 2022;2(1):17–29. doi:10.52589/BJCE-FY266HK9
23. Mohammedhussein M, Hajure M, Shifa JE, Hassen TA. Perceived stigma among 10 patients with pulmonary tuberculosis at public health facilities in southwest Ethiopia:11 A cross-sectional study. PLoS One. 2020;15(12):e0243433. doi:10.1371/journal.pone.0243433
24. Abuhammad S, Alzoubi KH, Khabour O. Fear of Covid‐19 and stigmatization towards infected people among Jordanian people. Int J of Clin Pract. 2021;75(4):e13899. doi:10.1111/ijcp.13899
25. Lysaker PH, Roe D, Yanos PT. Toward understanding the insight paradox: internalized stigma moderates the association between Insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophr Bull. 2006;33(1):192–199. doi:10.1093/schbul/sbl016
26. Maharjan S, Panthee B. Prevalence of self-stigma and its association with self-esteem among psychiatric patients in a Nepalese Teaching Hospital: a cross-sectional study. BMC Psychiatry. 2019;19(1):347. doi:10.1186/s12888-019-2344-8
27. Oei TP, Sawang S, Goh YW, Mukhtar F. Using the depression anxiety stress scale 21 (DASS-21) across cultures. Int J Psychol. 2013;48:1018–1029. doi:10.1080/00207594.2012.755535
28. Redfern A. Live COVID-19 vaccination tracker - see vaccinations in real time! 2021 Available from: https://covidvax.live/en/location/tha.
29. Sugiyama A, Miwata K, Kitahara Y, et al. Long covid occurrence in covid-19 survivors. Sci Rep. 2022;12(1):6039. doi:10.1038/s41598-022-10051-z
30. Osei E, Amu H, Appiah PK, et al. Stigma and discrimination tendencies towards covid-19 survivors: evidence from a nationwide population-based survey in Ghana. PLOS Glob Public Health. 2022;2(6):e0000307. doi:10.1371/journal.pgph.0000307
31. Chandran N, Vinuprasad VG, Sreedevi C, Sathiadevan S, Deepak KS. Covid-19-related stigma among the affected individuals: a cross-sectional study from Kerala, India. Indian J Psychol Med. 2022;44(3):279–284. doi:10.1177/02537176221086983
32. Bhatnagar S, Kumar S, Rathore P, et al. Surviving covid-19 is half the battle; Living Life with perceived stigma is other half: a cross-sectional study. Indian J Psychol Med. 2021;43(5):428–435. doi:10.1177/02537176211029331
33. Global Change Data Lab. United States: covid-19 weekly death rate by vaccination status. Our world in data; 2022. Available from: https://ourworldindata.org/grapher/united-states-rates-of-covid-19-deaths-by-vaccination-status?country=~All%2Bages.
34. Rewerska-Juśko M, Rejdak K. Social stigma of patients suffering from covid-19: challenges for health care system. Healthcare. 2022;10(2):292. doi:10.3390/healthcare10020292
35. Angskul T. MRNA vaccine for children aged 5 to 11. National News Bureau of Thailand; 2022. Available from: https://thainews.prd.go.th/en/news/detail/TCATG220216194715933.
36. Kitro A, Sirikul W, Dilokkhamaruk E, et al. Covid-19 vaccine hesitancy and influential factors among Thai parents and guardians to vaccinate their children. Vaccine. 2022;11:100182. doi:10.1016/j.jvacx.2022.100182
37. Zhang T-M, Fang Q, Yao H, Ran M-S. Public stigma of COVID-19 and its correlates in the general population of China. Int J Environ Res Public Health. 2021;18(21):11718. doi:10.3390/ijerph182111718
38. Kumar R, Singh V, Mohanty A, Bahurupi Y, Gupta PK. Corona health-care warriors in India: knowledge, attitude, and practices during COVID-19 outbreak. J Edu Health Promot. 2021;10(1):44. doi:10.4103/jehp.jehp_524_20
39. Haddad C, Bou Malhab S, Malaeb D, et al. Stigma toward people with covid-19 among the Lebanese population: a cross-sectional study of correlates and mediating effects. BMC Psychol. 2021;9(1):164. doi:10.1186/s40359-021-00646-y
40. Farhat M, Leurcharusmee S, Merttens F. Social impact assessment of covid-19 in Thailand - UNICEF. UNICEF; 2020. Available from: https://www.unicef.org/thailand/media/5071/file/SocialImpactAssessmentofCOVID-19inThailand.pdf.
41. Turner-Musa J, Ajayi O, Kemp L. Examining social determinants of health, stigma, and covid-19 disparities. Healthcare. 2020;8(2):168. doi:10.3390/healthcare8020168
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
