Back to Journals » Risk Management and Healthcare Policy » Volume 16
Status and Risk Factors in Patients Requiring Unplanned Intensive Care Unit Readmission Within 48 Hours: A Retrospective Propensity-Matched Study in China
Authors Yin YL, Sun MR, Zhang K, Chen YH, Zhang J, Zhang SK, Zhou LL, Wu YS, Gao P, Shen KK, Hu ZJ
Received 13 December 2022
Accepted for publication 24 February 2023
Published 11 March 2023 Volume 2023:16 Pages 383—391
DOI https://doi.org/10.2147/RMHP.S399829
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Yan-Ling Yin,1,* Mei-Rong Sun,1,* Kun Zhang,1 Yu-Hong Chen,1 Jie Zhang,1 Shao-Kun Zhang,1 Li-Li Zhou,1 Yan-Shuo Wu,1 Peng Gao,1 Kang-Kang Shen,1 Zhen-Jie Hu1,2
1Department of ICU, the Fourth Hospital of Hebei Medical University, Shijiazhuang City, Hebei Province, People’s Republic of China; 2Hebei Key Laboratory of Critical Disease Mechanism and Intervention, Shijiazhuang City, Hebei Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhen-Jie Hu, Tel +86-0311-86095588, Email [email protected]
Aim: This study investigated the current status and related risk factors of 48-hour unplanned return to the intensive care unit (ICU) to reduce the return rate and improve the quality of critical care management.
Methods: Data were collected from 2365 patients discharged from the comprehensive ICU. Multivariate and 1:1 propensity score matching analyses were performed.
Results: Forty patients (1.69%) had unplanned readmission to the ICU within 48 hours after transfer. The primary reason for return was respiratory failure (16 patients, 40%). Furthermore, respiratory failure (odds ratio [OR] = 5.994, p = 0.02) and the number of organ failures (OR = 5.679, p = 0.006) were independent risk factors for unplanned ICU readmission. Receiver operating characteristic curves were drawn for the predictive value of the number of organ injuries during a patient’s unplanned transfer to the ICU (area under the curve [AUC] = 0.744, sensitivity = 60%, specificity = 77.5%).
Conclusion: The reason for patient transfer and the number of organ injuries during the process were independent risk factors for patients who were critically ill. The number of organs damaged had a predictive value on whether the patient would return to the ICU within 48 hours.
Keywords: risk factors, 48-hour unplanned readmission, comprehensive ICU, propensity-matched study, respiratory failure
Background
A hospital’s intensive care unit (ICU) focuses on treating critically ill patients. After stabilising the patient’s condition, they are transferred to the relevant hospital department to continue treatment. Unplanned ICU readmission is when a patient is readmitted to the ICU for treatment during the same hospitalisation for various reasons, such as a short-duration aggravated condition. Studies have shown that patients returning to the ICU have a worse prognosis, with increased hospital fatality rates, significantly longer hospital stays, and increased medical and financial burdens.1–4 A study in the US showed that up to 14% of all ICU discharges could be readmitted.5 Presently, unplanned readmission to the ICU within 48 hours is used as a sensitive indicator of clinical medical quality.6
A retrospective review of readmission studies showed that at least 10% of all readmissions were preventable.7 Therefore, research on and discoveries of the risk factors for unplanned return to the ICU can promote further actions to reduce return incidences. Patient disease severity is important in predicting unplanned ICU readmission.6 The current tools to measure patient severity are mainly the acute physiology and chronic health evaluation (APACHE II) and sequential organ failure assessment (SOFA). However, studies have not yet reached a unified conclusion on the risk factors of unplanned ICU readmissions.6,8–11 In addition, limited studies have examined unplanned ICU readmittance within 48 hours.
Since ICU readmissions correlate with complex and severe illnesses, readmission rates require case-mix adjustment before they can be adequately interpreted as quality measures. Therefore, this study investigated the current status and related risk factors of a 48-hour unplanned return to the ICU. In addition, a 1:1 propensity score matching (PSM) analysis was used to align the baseline characteristics of patients with unintended transfers back to the ICU to eliminate any confounding factors.
Methods
Study Design and Patients
We conducted a retrospective cohort study of unplanned ICU (43 beds) readmissions in XX Medical University in China from January 2016 to December 2019. Informed consent was obtained either from the patient or by proxy. The study protocol was approved by an institutional research ethics committee (approval number: 2022KS021). This research did not receive specific grants from funding agencies in public, commercial or not-for-profit sectors.
Readmission was defined as discharge to an area that provided lower levels of care followed by a return to the same or different ICU during the same hospital stay. We excluded patients readmitted for emergency surgery after ICU discharge.
The ICU 48-hour readmission rates = number of readmissions within 48 hours/number of patients discharged alive and eligible for unit readmission during the same hospitalisation cycle × 100%.
Data Collection and Variables
Data were obtained via a retrospective investigation of the hospital’s comprehensive ICU patient entry and exit registration forms, electronic medical records, nursing documents and medical records management systems. Data were double-checked and input into Microsoft Excel.
Through a literature search,1,8,9,11 consultation with critical care medicine specialists and panel discussions, we designed a form to collect data that included:
- The patient’s general condition, age, gender, underlying disease, transfer to the department, etc.
- The reason for the transfer to the ICU, whether they had surgery, any medical history, vital signs when transferred to the ICU, oxygen saturation (SPO2) in the ICU and the APACHE II and SOFA scores within the first 24 hours.
- The vital signs, SPO2 and the APACHE II and SOFA scores when transferred out of the ICU.
Statistical Analysis
SPSS (Statistical Software Version 25.0, IBM SPSS Statistics, IL, USA) was used for data analysis. Continuous variables were expressed as mean ± standard deviation (SD) or median (interquartile range) based on the data distribution. Frequency and percentage were used for categorical variables. Potential differences of continuous variables between patients with or without ICU readmission were compared using two independent sample t-tests or Wilcoxon signed-rank test. The efficiency of the prediction model by discrimination (concordance index [C-index]) and calibration (Hosmer–Lemeshow goodness-of-fit test [HL test]) was also assessed. A 1:1 (Propensity Score Matching [PSM]) analysis with a calliper width of 0.005 of the SD was conducted to reduce potential selection bias between patients with or without ICU readmission.12,13 All variables significantly associated with ICU readmission in the univariate analysis were included in a multivariable logistic regression model. A p-value of less than 0.05 (p < 0.05) was considered statistically significant.
Results
There were 2500 patients admitted to the ICU during the study period (Figure 1). Among them, 135 patients were excluded either due to death (n = 31) or discharge (n = 84) from the ICU, transfer for emergency surgery (n = 16), or without complete data (n = 4). Therefore, 2365 patients from the hospital’s general wards were included. Among them, 40 (1.69%) patients who were readmitted to the ICU within 48 hours of transfer were included in the final analysis.
 |
Figure 1 Patient flowchart. |
To balance all baseline characteristics, eliminate the confounding factors, and further reduce selection bias, this study matched 40 patients who did not return to the ICU by a 1:1 PSM. The matched items included age, gender, medical history, surgical history, and the SOFA and APACHE II scores when they first entered the ICU (Table 1).
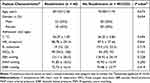 |
Table 1 Patient Demographic Characteristics After 1:1 PSM |
Patient Characteristics and Status
The characteristics of the patients readmitted to the ICU are shown in Table 2. The median age was 69 ± 12 years, and the distribution was roughly equal between male and female patients (22 vs 18). Of these 40 patients, 75% (n = 30) suffered from one or more chronic health conditions. More than half of the patients had undergone surgery (72.5% vs 27.5%). Organ failure was prevalent in all patients, and the median of organ failure was 2 (1, 3). In addition, the patients had APACHE II and SOFA median scores of 16 (13, 20) and (6.05 ± 3.59), respectively, when they were first admitted to the ICU.
 |
Table 2 Univariate Analysis of Patients with Unplanned Readmission to ICU Within 48 Hours and Without Readmission After 1:1 PSM |
Causes for ICU Readmission
The most common reason for ICU readmission was postoperative respiratory failure, observed in 16 patients (40%), followed by circulatory failure in five patients (12.5%). Other causes included perioperative period (n = 4, 10%), renal dysfunction (n = 3, 7.5%), delirium (n = 3, 7.5%), gastrointestinal disease (n = 3, 7.5%), neurological disease (n = 3, 7.5%) and sepsis (n = 3, 7.5%) (Figure 2).
 |
Figure 2 Reasons for intensive care unit readmission. |
Risk Factors for ICU Readmission
Univariate analysis found four variables that were significantly associated with ICU readmission, namely the reason for admission (p < 0.001), number of associated organ injuries (2 [1, 3] vs 1 [1, 1], p < 0.001), respiratory rate (R) and SOFA scores at first discharge between patients with and without ICU readmissions, R of 21 (18, 24) vs 19 (18, 21), p = 0.04 and SOFA of 1 (0, 2) vs 0 (0, 5), p = 0.012) (Table 2).
Considering these variables in the analytical model in logistic regression analysis, admissions for respiratory failure (odds ratio [OR] = 5.994, 95% confidence level [CI] = 1.319–27.242, p = 0 0.02) and number of organ injuries (OR = 3.022, 95% CI = 1.368–6.678, p = 0.006) were independent risk factors for ICU readmission (Table 3).
 |
Table 3 Multivariable Logistic Regression Analysis of Potential Risk Factors of ICU Readmission |
In addition, we plotted the receiver operating characteristic curve (ROC curve) of the number of organs damaged during patient transfer to the predictive value of unplanned return to the ICU within 48 hours and calculated the AUC (AUC = 0.744, sensitivity = 60% and specificity = 77.5%) (Figure 3).
 |
Figure 3 ROC curve. |
Discussion
To the best of our knowledge, this is the first retrospective observational study on patients’ unplanned readmission to the ICU within 48 hours via a 1:1 PSM analysis. Results showed that the 48-hour ICU readmission rate was 1.69%, which was at a low level globally (2.4% to 9.6%).8,11,14,15 Previous studies showed that unplanned readmissions were associated with more extended hospital stays and higher mortality. Therefore, it is necessary to consider unplanned readmissions to ICU as a sensitive indicator of the quality of care management. Compilations should be done quarterly, and comparisons should be made to identify problems promptly.
Risk Factors
We used propensity matching to control for all variables that affected the risk of readmission, such as basic patient information (age, gender, medical history and surgery), reasons for transfer, vital signs at transfer, and the SOFA and APACHE II scores.
Transfer Reasons
Our study found that the reason for ICU readmission within 48 hours was an independent risk factor. We divided the reasons for transfer into three major categories, namely respiratory and circulatory failures and others (such as bleeding, infection, etc.), and performed subgroup analyses. The results showed that respiratory failure was the leading cause of unplanned transfer (n = 16). This result was consistent with those of previous studies.1,15–19
The incomplete resolution of respiratory diseases remains a significant cause of potentially preventable ICU readmissions.19 Attention to sputum volume before ICU discharge may prevent unexpected readmissions. Applying nurse-led pulmonary physical therapy can effectively improve patient outcomes.20 In addition, general wards do not pay enough attention to patients’ respiratory status or lack of ability to predict changes in a patient’s condition, which may lead to unplanned transfers.
The readmission rate for breathing problems has been reported to range from 18% to 59%;18 our study’s result is 40%, which is on the higher side of the range. In future, we aim to focus on continuous treatment related to pulmonary diseases to enhance patients’ pulmonary rehabilitation, including integrating treatment with the general ward after the patient is transferred out of the ICU. Furthermore, family members will be invited to participate in the trinity management model.6
SOFA Scores
Most studies showed that SOFA scores at admission or discharge were associated with unplanned patient readmission.10,21 However, our findings were different and showed that, although patients readmitted had higher SOFA scores compared to those who were not (at first ICU admission 6.05 ± 3.59 vs 5.33 ± 3.92; at first ICU discharge 1 [0, 2] vs 0 [0, 5]), the logistic analysis showed that the SOFA scores had no association with patient readmission. Our findings support a previously reported study that the SOFA scores on discharge were not associated with patient readmissions.22 However, this finding may be related to the sample size and patient heterogeneity. Hence, further research is required.
Number of Organ Failures
We found that the number of patients with comorbid organ damage on the first admission to the ICU was an independent risk factor for unplanned readmission within 48 hours of transfer. However, limited studies support this finding. Patients admitted to the ICU usually have one or several organ failures, such as respiratory, renal, cerebral, circulatory, hepatic or coagulation disorders. There was a significant difference in respiratory parameters between readmitted and non-readmitted patients at discharge, with a lower PaO2/FiO2 ratio in the readmitted patients.23–25 Moreover, the respiratory score was considerably greater in readmitted patients when examining the specific SOFA measures. Moreover, respiratory conditions accounted for most of readmissions.26 As a consequence, respiratory functions seem to be crucial to the probability of ICU readmission, and patients might be released from the hospital with respiratory functions that are not adequately stable There may be a potential ward vulnerability with relation to particular respiratory assistance after critical care and therefore a comprehensive care of these patients is necessary.
A total of 678,960 patients were included in three studies.27 The different types of organ failures reported in the studies ranged from one to six, and the incidence of organ failure was 7%, 14% and 23%; the in-hospital mortality rate was 5%, 11% and 15%. The number of organ failures represented the patients’ severity. However, patients with organ failure can be treated, and organ function can be partially improved, but a complete recovery is a slow process. Therefore, after being transferred out of the ICU, the staff should pay close attention to partly recovered patients.
Limitations
This study had some limitations. First, this was a single-centre study with a limited sample size. After matching, only 40 patients were included in each group, resulting in wide intervals of predictors in univariate and multivariate analyses. Further multicentre studies with large sample sizes are warranted to verify our findings. Second, we only performed propensity matching on the patient’s basic information and information provided on admission. Third, the primary aim of this study was to investigate the risk factors and possible outcomes of ICU early readmission.
Conclusion
We identified two potential independent risk factors in this four-year retrospective analysis of 40 unplanned ICU readmissions within 48 hours. Respiratory failure remained the leading cause of readmission. In addition, the number of organs damaged on initial admission was a decisive factor in predicting unplanned readmissions. Hence, healthcare professionals should be concerned when patients have two or more damaged organs when they are first admitted to ICU. However, further randomized clinical trials are necessary to compare the effect of pre-emptive management versus routine care.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of The Fourth Hospital of Hebei Medical University (approval number: 2022KS021). Written informed consent was obtained from all participants.
Funding
No external funding.
Disclosure
The authors report no conflicts of interest in this work.
References
1. AbuSara AK, Nazer LH, Hawari FI. ICU readmission of patients with cancer: incidence, risk factors and mortality. J Crit Care. 2019;51:84–87. doi:10.1016/j.jcrc.2019.02.008
2. Daly K, Beale R, Chang RW. Reduction in mortality after inappropriate early discharge from intensive care unit: logistic regression triage model. BMJ. 2001;322(7297):1274–1276. doi:10.1136/bmj.322.7297.1274
3. Kramer AA, Higgins TL, Zimmerman JE. The association between ICU readmission rate and patient outcomes. Crit Care Med. 2013;41(1):24–33. doi:10.1097/CCM.0b013e3182657b8a
4. Xue Y, Klabjan D, Luo Y. Predicting ICU readmission using grouped physiological and medication trends. Artif Intell Med. 2019;95:27–37. doi:10.1016/j.artmed.2018.08.004
5. Kramer AA, Higgins TL, Zimmerman JE. Intensive care unit readmissions in U.S. hospitals: patient characteristics, risk factors, and outcomes. Crit Care Med. 2012;40(1):3–10. doi:10.1097/CCM.0b013e31822d751e
6. Nates JL, Nunnally M, Kleinpell R, et al. ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016;44(8):1553–1602. doi:10.1097/CCM.0000000000001856
7. Al-Jaghbeer MJ, Tekwani SS, Gunn SR, Kahn JM. Incidence and etiology of potentially preventable ICU readmissions. Crit Care Med. 2016;44(9):1704–1709. doi:10.1097/CCM.0000000000001746
8. Jo YS, Lee YJ, Park JS, et al. Readmission to medical intensive care units: risk factors and prediction. Yonsei Med J. 2015;56(2):543–549. doi:10.3349/ymj.2015.56.2.543
9. Killien EY, Huijsmans RLN, Vavilala MS, et al. Association of psychosocial factors and hospital complications with risk for readmission after trauma. J Surg Res. 2021;264:334–345. doi:10.1016/j.jss.2021.02.031
10. Kim HB, Na S, Paik HC, Joo H, Kim J. Risk factors for intensive care unit readmission after lung transplantation: a retrospective cohort study. Acute Crit Care. 2021;36(2):99–108. doi:10.4266/acc.2020.01144
11. Tejerina Álvarez EE, Gómez Mediavilla KA, Rodríguez Solís C, Valero González N, Lorente Balanza JÁ. Risk factors for readmission to ICU and analysis of intra-hospital mortality. Factores de riesgo de reingreso en UCI y análisis de la mortalidad intrahospitalaria. Med Clin. 2022;158(2):58–64. doi:10.1016/j.medcli.2020.11.035
12. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–3107. doi:10.1002/sim.3697
13. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. doi:10.1080/00273171.2011.568786
14. Holaubek C, Winter F, Lesjak A, et al. Perioperative risk factors for intensive care unit readmissions and mortality after cardiac surgery. J Cardiothorac Vasc Anesth. 2022;36(8Pt A):2339–2343. doi:10.1053/j.jvca.2021.10.044
15. Kogan A, Cohen J, Raanani E, et al. Readmission to the intensive care unit after “fast-track” cardiac surgery: risk factors and outcomes. Ann Thorac Surg. 2003;76(2):503–507. doi:10.1016/S0003-4975(03)00510-1
16. Tam OY, Lam SM, Shum HP, Lau CW, Chan KK, Yan WW. Characteristics of patients readmitted to intensive care unit: a nested case-control study. Hong Kong Med J. 2014;20(3):194–204. doi:10.12809/hkmj133973
17. Lin WT, Chen WL, Chao CM, Lai CC. The outcomes and prognostic factors of the patients with unplanned intensive care unit readmissions. Medicine. 2018;97(26):e11124. doi:10.1097/MD.0000000000011124
18. Mcneill H, Khairat S. Impact of intensive care unit readmissions on patient outcomes and the evaluation of the national early warning score to prevent readmissions: literature review. JMIR Perioper Med. 2020;3(1):e13782. doi:10.2196/13782
19. Tangonan R, Alvarado-Dyer R, Loggini A, et al. Frequency, risk factors, and outcomes of unplanned readmission to the neurological intensive care unit after spontaneous intracerebral hemorrhage. Neurocrit Care. 2022;37(2):390–398. doi:10.1007/s12028-021-01415-w
20. Sun J, Han W, Cui N, et al. Effect of nurse-led goal-directed lung physical therapy on the prognosis of pneumonia in sepsis patients in the ICU: a prospective cohort study. J Intensive Care Med. 2022;37(2):258–266. doi:10.1177/0885066620987200
21. Woldhek AL, Rijkenberg S, Bosman RJ, van der Voort PH. Readmission of ICU patients: a quality indicator? J Crit Care. 2017;38:328–334. doi:10.1016/j.jcrc.2016.12.001
22. Santos MC, Boniatti MM, Lincho CS, et al. Inflammatory and perfusion markers as risk factors and predictors of critically ill patient readmission. Rev Bras Ter Intensiva. 2014;26(2):130–136. doi:10.5935/0103-507X.20140019
23. Ouanes I, Schwebel C, Français A, et al. A model to predict short-term death or readmission after intensive care unit discharge. J Crit Care. 2012;27(4):422.e1–422.e4229. doi:10.1016/j.jcrc.2011.08.003
24. Gajic O, Malinchoc M, Comfere TB, et al. The stability and workload index for transfer score predicts unplanned intensive care unit patient readmission: initial development and validation. Crit Care Med. 2008;36(3):676–682. doi:10.1097/CCM.0B013E318164E3B0
25. Snow N, Bergin KT, Horrigan TP. Readmission of patients to the surgical intensive care unit: patient profiles and possibilities for prevention. Crit Care Med. 1985;13(11):961–964. doi:10.1097/00003246-198511000-00037
26. Kareliusson F, De Geer L, Tibblin AO. Risk prediction of ICU readmission in a mixed surgical and medical population. J Intensive Care. 2015;3(1):30. doi:10.1186/s40560-015-0096-1
27. Pedersen PB, Hrobjartsson A, Nielsen DL, Henriksen DP, Brabrand M, Lassen AT. Prevalence and prognosis of acutely ill patients with organ failure at arrival to hospital: a systematic review. PLoS One. 2018;13(11):e0206610. doi:10.1371/journal.pone.0206610
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
