Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
Statin Prescription Patterns and Associated Factors Among Patients with Type 2 Diabetes Mellitus Attending Diabetic Clinic at Muhimbili National Hospital, Dar es Salaam, Tanzania
Authors Bideberi AT, Mutagaywa R
Received 4 November 2021
Accepted for publication 21 January 2022
Published 27 February 2022 Volume 2022:15 Pages 633—646
DOI https://doi.org/10.2147/DMSO.S347765
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ming-Hui Zou
Aneth Telesphore Bideberi,1,2 Reuben Mutagaywa1,2
1Department of Internal Medicine, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; 2Department of Internal Medicine, Muhimbili National Hospital, Dar es Salaam, Tanzania
Correspondence: Aneth Telesphore Bideberi, Department of Internal Medicine, Muhimbili University of Health and Allied Sciences, P. O. Box 65001, Dar es Salaam, Tanzania, Tel +255 759334883, Email [email protected]
Purpose: To determine statin prescription patterns and associated factors among type 2 diabetes patients attending the diabetic clinic at Muhimbili National Hospital (MNH) in Dar es Salaam, Tanzania.
Patients and Methods: A hospital-based cross-sectional study involving outpatients was conducted from September 2020 to November 2020. Statin prescription history (both type and dosage) was obtained from patients as well as from the electronic medical records for determination of patterns. Participants were categorized as moderate or high risk for cardiovascular disease whereas prescription patterns were categorized as moderate and high intensity statins. Logistic regression was used to examine association, control confounders and effect modifier whereby p < 0.05 was considered statistically significant.
Results: Of 400 patients who were approached for the study, 395 (98.8%) were eligible for statin prescriptions. The mean (±SD) age of the study participants was 58.1± 10.3 years, out of which 371 (93.9%) belonged to the age group ≥ 40 years. Two-thirds(241 61.0%) of the patients were female. About two-thirds(257; 69.4%) of patients had health insurance coverage. Statins were prescribed in 47.3% of the participants. Moderate intensity statin was the only pattern prescribed. In the adjusted model, insurance coverage (OR: 0.056; 95% CI: 0.03– 0.12), and hypertension (OR: 0.259; 95% CI: 0.12– 0.54) were associated with an increased likelihood of being prescribed a moderate intensity statin.
Conclusion: A significant number of patients at MNH diabetic clinic were not on statins despite qualifying for the prescription. The findings call for further studies on reasons for low statin prescription practices in this tertiary facility.
Keywords: type 2 diabetes, statins, prescription, Tanzania
A Letter to the Editor has been published for this article.
A Response to Letter has been published for this article.
Introduction
Cardiovascular disease (CVD), which includes coronary artery disease (CAD), cerebrovascular accident, and peripheral arterial disease (PAD), is the leading cause of morbidity and mortality in patients with type 2 diabetes mellitus (T2DM).1 Patients with type 2 diabetes have an increased prevalence of lipid abnormalities, contributing to their high risk of CVD.2,3 Multiple clinical trials have demonstrated the beneficial effects of statins therapy on CVD outcomes in patients with and without coronary heart disease (CHD).4,5 Subgroup analyses of patients with diabetes in larger trials6–9 and trials in patients with diabetes10,11 showed significant primary and secondary prevention of CVD events and CAD deaths. Meta-analyses of 14 randomized trials of statin therapy, including data from over 18,000 patients with diabetes (mean follow-up 4.3 years) demonstrated a 9% proportional reduction in all-cause mortality and 13% reduction in vascular mortality for each mmol/L (39 mg/dL) reduction in LDL cholesterol.4
Accordingly, statins are the drugs of choice for LDL cholesterol lowering and cardio-protection. Statin prescription patterns in patients with diabetes are categorized as moderate or high intensity dosage. Moderate intensity dosage includes: atorvastatin 10–20 mg, rosuvastatin 5–10 mg, simvastatin 20–40 mg, pravastatin 40–80 mg, lovastatin 40 mg, fluvastatin 40 mg twice a day/80 mg once a day and pitavastatin 2–4 mg whereas high intensity dosage includes: atorvastatin 40–80 mg and rosuvastatin 20–40 mg.12 High intensity statin therapy achieves approximately a 50% reduction in LDL cholesterol and moderate intensity statin regimens achieve 30–50% reductions in LDL cholesterol. Low-dose statin therapy is generally not recommended in patients with diabetes but is sometimes the only dose of statin that a patient can tolerate.13 For patients who do not tolerate the intended intensity of statin, the maximally tolerated statin dose should be used.12 As in those without diabetes, absolute reductions in atherosclerotic cardiovascular disease (ASCVD) outcomes (coronary arterial disease death and non-fatal myocardial infarction) are greatest in people with high baseline ASCVD risk (known ASCVD and/or very high LDL cholesterol levels), but the overall benefits of statin therapy in people with diabetes at moderate or even low risk for ASCVD are convincing.14,15
The American Diabetes Association (ADA) standards of medical care in diabetes of 202112 recommends that: For patients of all ages with diabetes and ASCVD high-intensity statin therapy should be added to lifestyle therapy (Grade A recommendation); for patients with diabetes aged 40–75 years (grade A recommendation); for patients aged >75 years without ASCVD, use of moderate-intensity statin in addition to lifestyle therapy is recommended (grade B recommendation). For patients with diabetes aged <40 years with additional ASCVD risk factors, the patient and provider should consider using moderate-intensity statin in addition to lifestyle therapy (Grade C recommendation); In clinical practice, providers may need to adjust the intensity of statin therapy based on individual patient response to medication (for example; side effects, tolerability, low-density lipoprotein [LDL] cholesterol levels, or percent LDL reduction on statin therapy); for patients who do not tolerate the intended intensity of statin, the maximally tolerated statin dose should be used (Grade E recommendation); for patients with diabetes aged 40 years and above with multiple traditional cardiovascular risk factors without obvious ASCVD high intensity statins to be considered (Grade C recommendation).
Despite the fact that the role of statins in both primary and secondary prevention of cardiovascular disease is established, several real-world studies have shown a distance between guideline recommendations and use of statin treatment.16–18
Tanzania, like other developing countries, is facing a high burden of cardiovascular diseases (CVDs). The country is experiencing rapid growth of modifiable and intermediate-risk factors that accelerate CVD mortality and morbidity rates. In rural and urban settings, diabetes is among the cardiovascular risk factors which contribute to mortality and morbidity.19,20 High cholesterol is one of the most important and modifiable risk factors for the development of cardiovascular disease.21 Appropriate prescribing of cholesterol-lowering medications, therefore, represents one of the most important and accessible interventions for combating the burden. Obtaining baseline data on patterns of statin prescriptions, prevalence, and adherence to dosages of statins by benefit groups, sociodemographic and clinical determinants of statins prescription is critical for future intervention and prospective studies. The aim of this study was to determine statin prescription patterns and associated factors among type 2 diabetes patients attending a diabetes clinic at Muhimbili National Hospital, a tertiary hospital in Dar es Salaam, Tanzania.
Materials and Methods
Study Design, Area and Setting
A cross-sectional study design was conducted at Muhimbili National Hospital (MNH) in Dar es salaam, Tanzania. MNH is a tertiary hospital with 1500 bed capacity. The diabetic clinic is one of the clinics in the hospital, it operates 3 days a week. About 50–70 patients are consulted by doctors on each clinic appointment day. The clinic receives both insured and non-insured diabetes patients from within and outside of Dar es Salaam. The hospital has routine diabetic clinics every Tuesday, Wednesday, and Thursday. Overall, there are 5 Endocrinologists, 1 General practitioner, 9 nurses and 1 medical record officer who run the clinic. The clinic provides routine diabetic services such as glucose monitoring, vitals, weight and height assessment, medication prescriptions and diet advice sessions. Inclusion criteria for the study were adult patients with type 2 diabetes mellitus who have attended the clinic for at least 3 months who consented to participate in the study. Pregnant women and those categorized as having low cardiovascular risk (less than 40 years with no ASCVD risk) were excluded from the study.
Sample Size Calculation
Sample size for this study was conservatively calculated from the formula for cross-sectional design;22 considering that the outcome was binary, an estimate prevalence of 50% with a margin of error set arbitrarily at 5%, the upper limit of the sample size was estimated at 384 participants.
Sampling Technique and Study Procedures
Convenience sampling technique with consecutive enrolment of study participants was used whereby all consenting adult DM patients attending the Muhimbili diabetic clinic were recruited into the study. The recruitment process was conducted by recruiting eligible participants during the study period. Participants’ unique registration codes were also recorded and cross-checked to ensure that none of the participants was recruited more than once.
Study Variables
Dependent variables for the study included statin prescription patterns. The patterns are categorized as statin benefit group versus statin intensity as follows:12 (a) For patients with diabetes aged <40 years without additional ASCVD risk factors (low risk category) – none; (b) For patients with diabetes aged ≥40 without ASCVD (moderate risk category) – moderate intensity statins; (c) All ages with diabetes and ASCVD (high risk category) – high intensity statins; (d) Age ≥40 years with multiple (≥2 traditional cardiovascular risk factors) (high risk category) – high intensity statins.
Independent variables included sociodemographic characteristics and clinical and laboratory parameters. Demographic characteristics included: age, gender, and education level, insurance status. Clinical parameters included: (a) traditional cardiovascular risk factors: smoking history, duration of diabetes mellitus, obesity and hypertension; (b) atherosclerotic cardiovascular diseases: acute coronary syndrome, peripheral arterial disease and cerebral vascular events; (c) chronic diabetic complications: neuropathy, retinopathy and nephropathy; (d) cardiovascular risk stratification including moderate and high risk strata (where moderate risk <2, while high risk ≥2 traditional risk factors).23 Laboratory records included: low-density lipoproteins (LDL) cholesterol, protein in urine, creatinine, glycosylated hemoglobin (HbAIc). Estimation of kidney function (eGFR) – from Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.
We sought to establish the proportion of participants who belonged to the “very high risk” category, this being defined as documented/established to have any of the following conditions: acute coronary syndrome, coronary artery disease, peripheral arterial disease, chronic kidney disease (nephropathy), and cerebrovascular events.24–26
Data Collection
The investigator interviewed the patients and recorded laboratory results from the electronic system for all the recruited participants. Statin prescription was also confirmed from the electronic system. An interviewer-based structured case report form (questionnaire) was administered to consented patients or caretakers for those who are unable to communicate. Information collected included sociodemographic characteristics such as age, gender, marital status, education level, and insurance status. Medical information collected included current status of risk factors such as the history of hypertension, smoking, diabetes duration, acute coronary syndromes (ACS), arterial revascularization, stroke, peripheral artery disease. Use and dosage of statins whether low, moderate or high intensity was recorded. Diabetic and other medications in use were also recorded.
Clinical Measurements
Weight was measured on a SECCA weighing scale without shoes and recorded to the nearest 0.5 kg. Height was measured using a height measuring rod and recorded to the nearest 0.5 cm. Body mass index (BMI) was calculated as weight in kilograms (kg) divided by height in meters (m) squared expressed as kg/m2. The value obtained was classified as underweight (˂18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.5 kg/m2) or obese (˃30 kg/m2).27 Blood pressure was measured by placing a cuff 2 cm above the elbow crease on the bare arm with the midline of the bladder on the brachial artery. Then obliteration pressure was obtained and cuff was inflated 20–30 mmHg beyond the obliteration pressure. Cuff was deflated and the first and fifth Korotkoff sounds were recorded as systolic and diastolic blood pressures in mmHg respectively.28 Hypertension was defined as SBP of at least 140 mmHg and DBP of at least 90 mmHg.29 Alternatively, hypertension was defined as a documented history of hypertension with the current use of antihypertensive medications regardless of blood pressure level at the time of recruitment. Results were recorded on the clinical characteristics case report form.
Laboratory Investigations
Each patient’s serum cholesterol levels, proteinuria, creatinine and HbAIC levels were documented provided that these investigations were obtained in the previous visits. HbA1c control target of 6.5% according to American Diabetes Association was used.30 Low density lipoprotein (LDL) cholesterol was categorized as normal if it fell within the hospital’s chemistry laboratory reference range of 2.6–3.6 mmol/L.
Statistical Analysis
Data were entered and analysed using SPSS version 23.0 and exported to R software version 4.1.2 for analysis. Categorical data were summarized as frequencies and percentages whereas continuous variables were summarized using mean or median as appropriate depending on distribution. Groups were compared for differences using either Chi-square test or Fisher’s exact test. All variables with p <0.2 in the bivariate analysis were entered into the multivariate analysis model. Furthermore, a backward elimination approach was used to select which variables would be included in the final model using the Akaike information criterion (AIC);31 p <0.05 was considered statistically significant.
Ethical Considerations
Ethical clearance was obtained from the Muhimbili University of Health and Allied Sciences Research and Publication Committee (Ref: MUHAS-REC-06-2020-284). Permission to conduct the research was sought from MNH administration. Eligible patients were recruited only after verbal or written consent from themselves or their next of kin, for patients who could not provide verbal or written consent. All the principles of the Declaration of Helsinki were adhered to during the data collection process.
Results
In a 3-month study from September to November 2020, 400 participants were approached; 5 participants had low risk for cardiovascular disease (not requiring statin therapy), hence were excluded, the remaining 395 were studied and analyzed, as shown in Figure 1.
 |
Figure 1 CONSORT diagram to show the recruitment process of participants. Note: Adapted from Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Br Med J. 2010;340:c332. doi: 10.1136/bmj.c332. Creative Commons.48 |
The mean (±SD) age of the study participants was 58.1±10.3 years, out of which 371 (93.9%) belonged to the age group ≥40 years. Two-thirds (241; 61.0%) of the participants were females. Slightly above half of the participants (208; 52.7%) had elementary to primary education. About two-thirds (257; 69.4%) of patients had health insurance coverage. As per BMI (177; 44.8%) were overweight. About half the participants (192; 48.6%) had high blood pressure of ≥140/90 mmHg. The mean (±SD) duration of diabetes was 10.2 (±7.6) years with half of them having ≥ 10 years of the disease.
In the cohort of 395 participants, 307 (77.7%) participants had hypertension, 8 (2%) had CAD, 12 (3%) had PAD and 27 (6.8%) had CVEs. Documented cardiovascular complications, namely neuropathy, retinopathy and nephropathy were found in 309 (78.3%), 234 (59.2%), 121 (30.6%) of study participants, respectively.
For participants who had their LDL recorded, 59 (42.7%) had normal LDL while 82 (20.8%) had high values. Also for patients whose HbAIc was recorded, 44 (27.3%) reached the control target of <6.5%. Proteinuria was found in 104 (26.3%) and decline in kidney function as expressed by estimated glomerular filtration rate was found in 81 (32.5%). As per atherosclerotic risk stratification, the majority of participants (348; 88.1%) had high risk followed by moderate risk (47; 11.9%). The sociodemographic and clinical characteristics of the participants are described in Table 1.
 |
Table 1 Sociodemographic and Clinical Characteristics of type 2 Diabetes Participants (n = 395) |
The most frequently prescribed type of statin was atorvastatin (95%) at the dosage of 20 mg, followed by rosuvastatin (5%) at the dosage of 10 mg (Figure 2).
 |
Figure 2 Prescribed statins among study participants. |
Statin Prescription Patterns in Relation to CVD Risk Stratification
In this study, 395 (98.8%) participants were eligible for statins prescription however only 187 (47.3%) were prescribed with statins. About 47 (11.9%) had moderate risk, and among them 21 (44.7%) received moderate intensity statin. The majority of the study participants had high risk (348; 88.1%) among which 166 (47.7%) received moderate intensity statins and the remaining 182 (52.3%) did not receive statins. Moderate intensity statin was the only pattern found in this study with none of the participants being on either low intensity or high intensity statin prescriptions (Figure 3).
 |
Figure 3 Prescription of statins in relation to risk stratification among type 2 diabetes participants. |
Participants in the “very high risk” cardiovascular category accounted for 133/395 (33.7%). Of these participants, 82/133 (61.7%) were on moderate intensity statins prescription (Table not shown).
Factors Associated with Statin Prescription Patterns
Bivariate analysis revealed that participants aged ≥40 years were significantly more often prescribed with moderate intensity statin than those of <40 years (49.9% versus 8.3%, p< 0.001).
Moderate intensity statin prescription pattern was seen more in participants with health insurance than those without (175; 63.6% versus 10.0%, p< 0.001).
Participants with diabetes duration of ≥10 years were significantly more often prescribed moderate intensity statin than those with less than <10 years diabetes duration (54.7% versus 39.7%, p = 0.003).
Individuals with history of hypertension were significantly more often prescribed with moderate intensity statins than non-hypertensive individuals (52.2% versus 30.0%, p<0.001).
Participants who had coronary arterial disease were significantly more often prescribed with moderate intensity statins therapy compared with those without coronary artery disease (87.5% versus 46.5%, p = 0.023).
Participants with high levels of LDL were not significantly prescribed with moderate intensity statins compared with those with normal LDL levels (68.3% versus 64.4%, p = 0.763). Participants with positive protein in urine were not significantly prescribed moderate intensity statins than those with negative protein in urine (57.0% versus 60.7%, p = 0.634).
Moreover, cardiovascular complications among participants such as neuropathy, retinopathy and nephropathy were seen in 78.3%, 59.2%, and 30.6%, respectively, and moderate intensity statins were prescribed more in nephropathy (62%), followed by retinopathy (50.9%) and neuropathy (48.5%).
Of the cardiovascular complications, cerebral vascular event was the most frequent documented complication (6.8%), followed by peripheral arterial disease (3.0%) and coronary arterial disease (2.0%). Among the participants with documented complications, moderate intensity statins were prescribed in at least half (50%) for each of the individual complications; with the only exception being among participants with neuropathy whom only 48.5% were on moderate intensity statin prescription (Table 2). However, gender, education level, prescriber’s title, history of cigarette smoking, reduced eGFR <60 mL/min/1.73 m2 and HbAIc ≥ 6.5% were not associated with moderate intensity statin prescription (Table 2).
 |
Table 2 Factors Associated with Statin Prescription Patterns Among Type 2 Diabetes Participants (N = 395) |
The multivariate logistic regression examined associations between statins prescription patterns and various factors. Age was not associated with statins prescription patterns (OR: 0.203; 95% CI: 0.02–1.87). Having medical insurance increased the likelihood of being on statins prescriptions compared with not being insured by 94.4% insurance coverage (OR: 0.056; 95% CI: 0.03–0.12). Furthermore, being hypertensive increased the likelihood of being on statins prescription by 74.1% (OR: 0.259; 95% CI: 0.12–0.54). Diabetes duration, body mass index, education level and proteinuria were not associated with moderate intensity statin prescription after adjustment for the other variables in the model (Table 3).
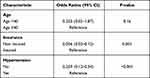 |
Table 3 Multivariate Logistic Regression on Factors Associated with Statin Prescription Patterns |
Discussion
The current study sought to provide data on statin prescription patterns for the prevention of CVD among participants with type 2 diabetes mellitus. Prescription patterns were evaluated in relation to risk stratification in patients with T2DM. It was found that statins were prescribed in about half of the participants with T2DM who were eligible for prescription. Findings of this study were similar to those found by Mwita et al.,32 Demoz et al.33 and Gupta et al.23 and in which statin prescriptions were 45.5% and 55.7%, respectively. The explanation for such a low prescription rate could be due to the following reasons: firstly, lack of local guidelines, secondly, inadequate adherence to already recommended international guidelines,33,34 and thirdly, limited access to medications and lipid tests due to poor socioeconomic status.
Of those patients who received statins (n = 187), moderate intensity statins prescription was the only pattern found in 47.3%, similarly to 46.1% in the study done by Dermoz et al.32 Likewise, almost half of patients (166; 47.7%) in a high risk group (n = 348) were prescribed with moderate-dose statins, contrary to the recommendations12,35 while more than half in this group did not receive statins despite being at high risk.
In this study, atorvastatin was found to be the most commonly prescribed type of statin, followed by rosuvastatin. Similarly, in a study done by Gupta et al.,23 atorvastatin was the most commonly prescribed type of statin (74.1%), followed by rosuvastatin (29.2%). In contrast to this, Demoz et al.33 found that simvastatin (37.2%) was the most commonly prescribed statin, followed by atorvastatin (32.8%) and rosuvastatin (15.6%). Reasons for discrepancies could be availability, cost, and physician preference.36,37
With regards to cholesterol levels it was found that having high levels of low density lipoprotein was not associated with statins prescription pattern. Our findings are in contrast to the observation from previous studies that revealed clinicians tend to prescribe statins based on the baseline LDL-C levels rather than to the patients’ overall CVD risk profile as described in clinical guidelines.38,39 Although there is a lack of local guidelines, MNH diabetes clinic has adopted ADA guidelines which recommend statins along with lifestyle changes regardless of cholesterol levels for all patients with diabetes aged >40 years with or without CVD.12 These findings may suggest a need for deliberate efforts for improving the understanding and implementation of the adopted guidelines.
Concerning insurance coverage, those who had medical insurance had very high odds of being prescribed with statins, as observed in other studies.40–42 This can be explained by the easy access of these drugs in insurance packages, hence facilitating prescription. On the other hand, even among those who are medically insured and eligible, some were not on statin prescription. This might as well have been caused by an absence of guidelines in the hospital to guide statin prescription.
Likewise, participants who had history of hypertension as a comorbid condition were significantly more often prescribed with statins compared with those without hypertension. This association has also been reported by various other studies.43,44 Therefore having a comorbid condition such as hypertension along with diabetes should be regarded as a high risk for developing cardiovascular diseases, hence this should trigger intervention by clinicians in order to provide the best care to these patients before they succumb to cardiovascular complications.
In our study, proteinuria was not associated with statins prescription pattern. This finding is in contrast to that of Berthold et al. who reported that patients with proteinuria had increased odds of statin prescription in Germany.34 Since proteinuria is a marker of renal disease, it is disturbing to see participants with proteinuria in this study received lesser statin prescriptions. We highly encourage clinicians to recognize proteinuria as a predictor of CVD and to increase statins prescription in this group of participants.
Interestingly, the present study found that of those participants who received statin therapy, only 38/94 (40.4%) (Table 2) were found to have normal range LDL-cholesterol level. Certainly, only one third (35.7%) of patients in this study had a detailed lipid profile. This indicates noncompliance with the standard guidelines about monitoring of lipid profile, i.e., that all patients with type 2 diabetes should be tested at least annually.35 This might also be the reason for the low percentage of patients with normal range cholesterol levels. Therefore, there is a need to emphasize periodic monitoring of patients’ lipid levels in optimizing the utilization of statins in response to the CVD risks factors. Such an initiative will ensure that statin prescription decisions are, at least in part, based on the risk assessment and lipid profile.
Multivariate regression analysis revealed that there was no significant association between diabetes duration and statin prescription. In contrast some studies and clinical guidelines have reported association of longer diabetes duration and tendency to statin prescription.31,45 The difference here may be because almost half of the patients (49%) had less than 10 years diabetes duration from the time of diagnosis.
Smoking was also not found to be associated with statin prescription in this study. This lack of association was also found in other studies.31 Our finding is in contrast to other studies which showed that patients with history of smoking had increased odds of being prescribed with statins.46 The overall low smoking and alcohol consumption habits in the Tanzania population could contribute to this effect.26 Also, one of the lifestyle modifications in diabetes mellitus is to limit cigarette smoking.
Increase in age and BMI were also not associated with statin prescription in this study; this was contrary to other studies46,47 where the odds of being prescribed statins were seen in more elderly and in overweight/obese patients. This could be attributed to differences in population representation or the fact that prescribers fear to increase the burden of pills to these high-risk groups to avoid adverse effects as the majority have also been prescribed with other medications.
The findings of this study should be interpreted against the background of several limitations. These include lack of standard risk stratification tool and lack of systematic collected data on microvascular complications (especially renal disease). There is also a possibility of recall bias in participants to some of the disease presentations that could have resulted in inaccurate estimation of their comorbid conditions. Moreover, a qualitative analysis to determine causes of low statin prescriptions by clinicians was not performed. On the other hand, cardiovascular risk categories are derived from international societies and not from Tanzania or regional-specific guidelines. Therefore, one of the limitations is that these CV risk scores and categories might be different in patients in Tanzania (more research is needed to define population-specific risk scores/charts). Categorization of participants into very high risk was based on documented complications, this is likely to be an underestimate as we did not actively assess the participants to obtain any undocumented complications. The use of convenience sampling hinders external generalization of the findings of this study to the general population of diabetes patients in Tanzania. This is the first hospital-based cross-sectional study of its kind in a tertiary hospital in Tanzania that assessed statin prescription patterns and its associated factors. The study has helped to identify the gaps in statin prescribing practice among clinicians and raise awareness for development of local guidelines in order to guide treatment.
Conclusion
This study showed suboptimal statin prescription among type 2 diabetes participants attending a diabetes clinic at Muhimbili National Hospital. Moderate intensity statins prescription was the only pattern found among diabetes participants. Strategies to optimize prescriptions at the clinic should focus on exploring reasons for low statin prescription, clinicians’ awareness of recommended guidelines, continuing medical education as well as time to time prescription audits and dissemination of results to improve quality of preventive care among patients with type 2 diabetes mellitus.
Data Sharing Statement
The data set generated and/or analyzed during this study is available from the corresponding author on reasonable request.
Consent to Publish
All authors read and approved the submitted manuscript.
Acknowledgments
We would like to thank the study participants for voluntarily participating in this study, staff of Muhimbili National Hospital Diabetic clinic in Dar es Salaam, Tanzania for cooperation throughout the study.
Funding
The study did not receive any funding.
Disclosure
Both authors declare no conflicts of interest for this work.
References
1. King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21(9):1414–1431. doi:10.2337/diacare.21.9.1414
2. Martín-Timón I, Sevillano-Collantes C, Segura-Galindo A, Del Cañizo-Gómez FJ. Type 2 diabetes and cardiovascular disease: have all risk factors the same strength? World J Diabetes. 2014;5(4):444. doi:10.4239/wjd.v5.i4.444
3. Morrish N, Wang S-L, Stevens L, Fuller J, Keen H, Group WMS. Mortality and causes of death in the WHO multinational study of vascular disease in diabetes. Diabetologia. 2001;44(2):S14. doi:10.1007/PL00002934
4. Mihaylova B, Emberson J, Blackwell L, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–590. doi:10.1016/S0140-6736(12)60367-5
5. Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–1278. doi:10.1016/S0140-6736(05)67394-1
6. Pyörälä K, Pedersen TR, Kjekshus J, Faergeman O, Olsson AG, Thorgeirsson G. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease: a subgroup analysis of the Scandinavian Simvastatin Survival Study (4S). Diabetes Care. 1997;20:614–620. doi:10.2337/diacare.20.4.614
7. Armitage J, Collins R. Need for large scale randomised evidence about lowering LDL cholesterol in people with diabetes mellitus: MRC/BHF heart protection study and other major trials. Heart. 2000;84(4):357–360. doi:10.1136/heart.84.4.357
8. Shepherd J, Barter P, Carmena R, et al. Effect of lowering LDL cholesterol substantially below currently recommended levels in patients with coronary heart disease and diabetes: the Treating To New Targets (TNT) study. Diabetes Care. 2006;29:1220–1226. doi:10.2337/dc05-2465
9. Sever P, Poulter N, Chang C-L, et al. The Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT): testing C-Reactive protein at baseline and on-treatment as an independent predictor of cardiovascular outcomes. Am Coll Cardiol. 2013;8(62):8–20. doi:10.1016/j.jacc.2013.02.098
10. Knopp RH, D’Emden M, Smilde JG, Pocock SJ. Efficacy and safety of atorvastatin in the prevention of cardiovascular end points in subjects with type 2 diabetes: the Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in Non-Insulin-Dependent Diabetes Mellitus (ASPEN). Diabetes Care. 2006;29:1478–1485. doi:10.2337/dc05-2415
11. Colhoun HM, Betteridge DJ, Durrington PN, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364:685–696. doi:10.1016/S0140-6736(04)16895-5
12. Cefalu WT, Berg EG, Saraco M, et al. American Diabetes Association: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(Suppl.1):S15–S33. doi:10.2337/dc21-S002
13. Weng TC, Yang YHK, Lin SJ, Tai SH. A systematic review and meta-analysis on the therapeutic equivalence of statins. J Clin Pharm Ther. 2010;35(2):139–151. doi:10.1111/j.1365-2710.2009.01085.x
14. Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–1681. doi:10.1016/S0140-6736(10)61350-5
15. Wilson PWF, Polonsky TS, Miedema MD, Khera A, Kosinski AS, Kuvin JT. Correction to: systematic Review for the 2018AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1144–e1161. doi:10.1161/CIR.0000000000000700
16. Morieri ML, Perrone V, Veronesi C, et al. Improving statin treatment strategies to reduce LDL-cholesterol: factors associated with targets’ attainment in subjects with and without type 2 diabetes. Cardiovasc Diabetol. 2021;20:144. doi:10.1186/s12933-021-01338-y
17. Ray KK, Molemans B, Schoonen WM, et al. EU-wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: the DAVINCI study. Eur J Prev Cardiol. 2021;28:1279–1289. doi:10.1093/eurjpc/zwaa047
18. Morieri ML, Avogaro A, Fadini GP; the DARWIN-T2D Network of the Italian Diabetes Society. Cholesterol lowering therapies and achievement of targets for primary and secondary cardiovascular prevention in type 2 diabetes: unmet needs in a large population of outpatients at specialist clinics. Cardiovasc Diabetol. 2020;19:190. doi:10.1186/s12933-020-01164-8
19. Roman WP, Martin HD, Sauli E. Cardiovascular diseases in Tanzania: the burden of modifiable and intermediate risk factors. J Xiangya Med. 2019;1–13. doi:10.21037/jxym.2019.07.03
20. Mboera L, Kishamawe C, Rumisha SF, Chiduo MG, Kimario E. Patterns and trends of hospital mortality due to noncommunicable diseases and injuries in Tanzania: a 10- year retrospective analysis. Available from: https://orcid.org/0000-0001-5746-3776.
21. Nelson RH. Hyperlipidemia as a risk factor for cardiovascular disease. Prim Care. 2013;40(1):195–211. doi:10.1016/j.pop.2012.11.003
22. Arya R, Antonisamy B, Kumar S. Sample size estimation in prevalence studies. Indian J Pediatr. 2012;79(11):1482–1488. doi:10.1007/s12098-012-0763-3
23. Gupta R, Lodha S, Sharma KK, et al. Evaluation of statin prescriptions in type 2 diabetes: india Heart Watch-2. BMJ Open Diabetes Res Care. 2016;4(1):e000275. doi:10.1136/bmjdrc-2016-000275
24. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227–239. doi:10.1161/01.CIR.0000133317.49796.0E
25. Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25Pt B):2889–2934. doi:10.1016/j.jacc.2013.11.002
26. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1–87. doi:10.4158/EP171764.APPGL
27. Tanzania Ministry of Health. Tanzania Demorgraphic and Health Survey Indicator Survey (TDHS-MIS) 2015–2016. Dar Es Salaam, Tanzania, Rockville, Maryland, USA MoHCDGEC, MoH, NBS, OCGS, ICF. Available from: https://dhsprogram.com/pubs/pdf/fr321/fr321.pdf.
28. Williams JS, Brown SM, Conlin PR. Videos in clinical medicine. blood-pressure measurement. N Engl J Med. 2009;360(5):e6. doi:10.1056/NEJMvcm0800157
29. James PA, Oparil S, Carter BL, et al. Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520. doi:10.1001/jama.2013.284427
30. American Diabetes Association. Glycemic targets: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Supplement 1):s61–s70. doi:10.2337/dc19-S006
31. Akaike information criterion. Available from: https://www.sciencedirect.com/topics/social-sciences/akaike-information-criterion.
32. Mwita JC, Godman B, Esterhuizen TM. Statin prescription among patients with type 2 diabetes in Botswana: findings and implications. BMC Endocr Disord. 2020;20(1):36. doi:10.1186/s12902-020-0516-7
33. Demoz GT, Wahdey S, Kasahun GG, et al. Prescribing pattern of statins for primary prevention of cardiovascular diseases in patients with type 2 diabetes: insights from Ethiopia. BMC Res Notes. 2019;12(1):386. doi:10.1186/s13104-019-4423-9
34. Berthold HK, Gouni-Berthold I, Böhm M, Krone W, Bestehorn KP. Patterns and predictors of statin prescription in patients with type 2 diabetes. Cardiovasc Diabetol. 2009;8(25):1–12. doi:10.1186/1475-2840-8-25
35. IDF Diabetes Atlas 2019. International diabetes federation; 2019. Available from: http://www.idf.org/about-diabetes/facts-figures.
36. Sarfo FS, Ovbiagele B. Prevalence and predictors of statin utilization among patient populations at high vascular risk in Ghana. J Neurol Sci. 2020;414:116838. doi:10.1016/j.jns.2020.116838
37. Yeh JS, Franklin JM, Avorn J, Landon J, Kesselheim AS. Association of industry payments to physicians with the prescribing of brand-name statins in Massachusetts. JAMA Intern Med. 2016;176(6):763–768. doi:10.1001/jamainternmed.2016.1709
38. Athyros VG, Katsiki N, Karagiannis A, Mikhailidis DP. Statins can improve proteinuria and glomerular filtration rate loss in chronic kidney disease patients, further reducing cardiovascular risk. Fact or fiction? Expert Opin Pharmacother. 2015;16(10):1449–1461. doi:10.1517/14656566.2015.1053464
39. Singh BM, Lamichhane HK, Srivatsa SS, et al. Role of statins in the primary prevention of atherosclerotic cardiovascular disease and mortality in the population with mean cholesterol in the near-optimal to borderline high range: a systematic review and meta-analysis. Adv Prev Med. 2020;2020:6617905. doi:10.1155/2020/6617905
40. Wu J, Zhu S, Yao GL, Mohammed MA, Marshall T. Patient factors influencing the prescribing of lipid lowering drugs for primary prevention of cardiovascular disease in UK general practice: a National Retrospective Cohort Study. PLoS One. 2013;8(7):e67611. doi:10.1371/journal.pone.0067611
41. Norris P, Horsburgh S, Becket G, et al. Equity in statin use in New Zealand. J Prim Health Care. 2014;6(1):17–22. doi:10.1071/HC14017
42. Kitzmiller JP, Foraker RE, Rose KM. Lipid-lowering pharmacotherapy and socioeconomic status: atherosclerosis risk in communities (ARIC) surveillance study. BMC Public Health. 2013;13:488. doi:10.1186/1471-2458-13-488
43. King DE, Mainous AG, Egan BM, Player M, Geesey ME. Use of statins and blood pressure. Am J Hypertens. 2007;20(9):937–941. doi:10.1016/j.amjhyper.2007.03.018
44. D’Agostino RB, Kannel WB, Stepanians MN, D’Agostino LC. Efficacy and tolerability of lovastatin in hypercholesterolemia in patients with systemic hypertension. Am J Cardiol. 1993;71(1):82–87. doi:10.1016/0002-9149(93)90715-o
45. Lielith V. Type 2 diabetes mellitus in a dutch region: epidemiology and shared care. Available from: https://pure.rug.nl/ws/portalfiles/portal/66113685/L.Ubink_Veltmaat.pdf.
46. Neutel CI, Morrison H, Campbell NRC, de Groh M. Statin use in Canadians: trends, determinants and persistence. Can J Public Heal. 2007;98(5):412–416. doi:10.1007/BF03405430
47. Savoie I, Kazanjian A. Utilization of lipid-lowering drugs in men and women. a reflection of the research evidence? J Clin Epidemiol. 2002;55(1):95–101. doi:10.1016/s0895-4356(01)00436-x
48. chulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials Br Med J. 2010;340:c332. doi:10.1136/bmj.c332. Creative Commons.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
