Back to Journals » International Journal of General Medicine » Volume 14
Standing 8-Electrode Bioelectrical Impedance Analysis as an Alternative Method to Estimate Visceral Fat Area and Body Fat Mass in Athletes
Authors Lee LC , Hsu PS, Hsieh KC , Chen YY, Chu LP , Lu HK , Chiu YC , Li L, Lai CL
Received 14 September 2020
Accepted for publication 14 December 2020
Published 24 February 2021 Volume 2021:14 Pages 539—548
DOI https://doi.org/10.2147/IJGM.S281418
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ling-Chun Lee,1,* Pi-Shan Hsu,2,3,* Kuen-Chang Hsieh,4– 6 Yu-Yawn Chen,7 Lee-Ping Chu,8 Hsueh-Kuan Lu,9 Yen-Chen Chiu,10 Lin Li,11 Chung-Liang Lai12,13
1Department of Physical Education, Chinese Culture University, Taipei, Taiwan; 2Department of Family Medicine, Taichung Veterans General Hospital, Taichung, Taiwan; 3Graduate Institute of Microbiology and Public Health, National Chung-Hsing University, Taichung, Taiwan; 4Fundamental Education Center, National Chin-Yi University of Technology, Taichung, Taiwan; 5Big Data Center, National Chung-Hsing University, Taichung, Taiwan; 6Office of Physical Education, Fu Jen Catholic University, New Taipei, Taiwan; 7Division of Food Nutrition, National Taitung Junior College, Taitung, Taiwan; 8Department of Orthopedics, China Medical University Hospital, Taichung, Taiwan; 9General Education Center, National Taiwan University of Sport, Taichung, Taiwan; 10Department of Exercise Health Science, National Taiwan University of Sport, Taichung, Taiwan; 11Department of Physical Medicine and Rehabilitation, Taichung Hospital, Ministry of Health and Welfare, Taichung, Taiwan; 12Department of Physical Medicine and Rehabilitation, Puzi Hospital, Ministry of Health and Welfare, Chiayi, Taiwan; 13Department of Occupational Therapy, Asia University, Taichung, Taiwan
*These authors contributed equally to this work
Correspondence: Chung-Liang Lai
Department of Physical Medicine and Rehabilitation, Puzi Hospital, Ministry of Health and Welfare, No. 42– 50, YungHo Vil., Puzi City, Chiayi County, 61347, Taiwan
Tel +886-5-379-0600
Email [email protected]
Purpose: To investigate the potential of standing 8-electrode bioelectrical impedance analysis (BIA) for assessing visceral fat area (VFA) and body fat mass (BFM) in athletes.
Materials and Methods: A total of 95 subjects (50 males and 45 females) were recruited. VFA and BFM measurements were obtained using three standing 8-electrode BIA devices, InBody230, InBody770, and IOI353. These acquired VFA and BFM were expressed as VFAIOI353, VFAInBody230, VFAInBody770 V, BFMIOI353, BFMInBody230, and BFMInBody770, respectively. As reference measurement, the VFA acquired from computer tomography (CT) was expressed as VFACT, and the BFM measured by dual-energy X-ray absorptiometry (DXA) was denoted as BFMDXA.
Results: The coefficient of determination (r2) in regression analysis between the measurements by VFAIOI353, VFAInBody230, VFAInBody770 and VFACT were 0.425, 0.492, and 0.473, respectively. Also, the limits of agreement (LOA) obtained from Bland–Altman analysis were − 25.18 to 56.62, − 29.74 to 62.44, and − 32.96 to 71.93 cm2. For BFM, r2 in regression analysis between the measurements by BFMIOI353, BFMInBody230, BFMInBody770 and BMFDXA were 0.894, 0.950, and 0.955, respectively; LOA were − 7.21 to 5.75, − 4.70 to 4.05, and − 5.48 to 3.05 kg, respectively.
Conclusion: The results showed when assessing BFM, these instruments delivered comparable measurements, and the degree of agreement ranged from excellent to moderate compared with the reference method. However, when assessing VFA, the agreements were weak. Therefore, the application of standing 8-electrode BIA devices for assessing athletes’ VFA still needs improvement.
Keywords: bioelectrical impedance analysis, body fat mass, visceral fat area
Introduction
Excess visceral adiposity is a risk factor for metabolic syndrome and is related to type 2 diabetes and cardiovascular diseases.1,2 Hence, valid and reliable methods for visceral fat would be of great value in identifying patients at risk of metabolic syndrome. Reference methods for measuring visceral fat are MRI (magnetic resonance imaging)3 and CT (computed tomography).4 These methods can quantify visceral fat directly but have the disadvantages of high cost, time-consuming, and labor-intensive. Other surrogate markers of visceral adiposity include body mass index (BMI), waist-to-hip ratio,5,6 and fat estimates by DXA (dual-energy X-ray absorptiometry),7 is less expensive and more convenient, but has the disadvantage of indirect measurement for visceral fat. BMI is a commonly used measurement among the current methods of categorizing body fatness because of its convenience and simplicity. However, research has shown limited accuracy for categorizing body fatness by using BMI.8,9
BIA (bioelectrical impedance analysis) is a simple, safe, fast, and noninvasive body composition tool in clinical and epidemiological studies.10 It provides body composition estimates, such as body fat mass, lean body mass, and body fat percentage, using equations derived from the impedance of the total body or body segments.11 The accuracy of BIA assessment can be validated by DXA, CT, MRI and deuterium dilution method. The commercially available BIAs use single or multiple frequency currents for measurements, and the derived impedance can be used to estimate body composition parameters by established empirical equations. Apart from that, the bioimpedance spectroscopy system can assess body composition without using empirical equations.12–14
In addition to the body composition estimates mentioned above, most modern BIA models also provide a simple method for the measure of VFA (visceral fat area). Therefore, it may also be a potential tool for body adiposity study.
Many studies have been conducted to examine body composition in athletes of different ethnic origins;15 however, research on the measurement of BIA in athletes’ abdominal visceral fat are limited. Existing research reports that abdominal visceral fat and body fat weight are highly correlated in the general population, as well as obese populations.16
BFM (body fat mass) and distribution are directly correlated to the performance and health of athletes and, therefore, tracing BFM and VFA may hold value for coaches and trainers for monitoring training adaptations and metabolic risk in athletes, and possibly for monitoring athletes after retirement. The accuracy of BIA measure for BFM has been widely discussed in general population13 and athletes15 in different ethnic groups. Unlike to the well-established role of fat estimates by BIA, there is limited literature to support the use of VFA by BIA. Controversial results about the potential role of VFA by BIA have been reported with low to high positive correlations between VFA measured by CT and BIA in general,17–21 aging,22 and obese23 populations. For the athlete, most studies have focused on measuring fat-free mass, BFM or percentage of body fat rather than the assessment of VFA and BFM and research that focuses on validating VFA by BIA is limited.
The purpose of this study was to validate the assessment of BFM and VFA by standing 8-electrode BIA devices in athletes. In this study, BFM by BIA was validated against BFM by DXA and VFA by BIA was validated against VFA by single-sliced CT. The relationship between VFA and BFM was also explored.
Materials and Methods
Ninety-five athletes (50 males, 45 females; age range: 20.5–30.0 years) were recruited as participants. All participants were informed of the purpose and the details of the study, and upon a full understanding of their rights, they were asked to sign a consent form. Participants were asked to empty their bladder of urine 20 min before measurements were taken, and they changed into cotton gowns (weight about 450 g). Each participant then completed anthropometry, BIA, DXA, and CT assessments (in that sequence). All procedures were completed within 90 min. Female test subjects refrained from testing during the menstruation. This study was approved by the Institutional Review Board of Tasotun Psychiatric Center, which is the same hospital alliance group as our institution (Nan-Tou, Taiwan). (IRB No. 107,031, Chinese Clinical Trial Registry: ChiCTR 1,900,024,743). All procedures were conducted according to the Declaration of Helsinki.
Participants were weighed to the nearest 0.1 kg using a Weight-Tronix digital scale (Scale Electronics Development, New York, USA). Participant’s height was measured without shoes to the nearest 0.5 cm using a Stadiometer (Holtain, Crosswell, Wales, UK). BMI was calculated as weight divided by height squared (kg/m2).
When standing 8-electrode BIA assessments were performed, participants only wore a cotton gown. We used three different standing 8-electrode BIA devices for assessing body composition: (1) IOI353 (Jawon Medical, Gyeongsan, Korea) is a multi-frequency BIA device which measures at 5 kHz, 50 kHz, and 250 kHz (250 mA), respectively; (2) InBody230 (Biospace, Seoul, Korea) is a two- frequency BIA device which measures at 20 kHz and 100 kHz (330 mA), respectively; and (3) InBody770 (Biospace, Seoul, Korea) is a multifrequency BIA device which measures at 1 kHz, 5 kHz, 50 kHz, 250 kHz, 500 kHz, and 1000 kHz (80 mA), respectively. All three standing 8-electrode BIA instruments had eight stainless steel electrodes mounted on a hand-grip and footplate with a built-in weight sensor embedded in the base of the instrument. When conducting the measurement, the participant stood on the base contact plate with bare feet and placed both hands on the hand-grips with their arms slightly open, apart from the trunk. Participants’ feet were placed on the base contact plate. Subjects stood for 30 min before the BIA measurement was taken, as the water in the body was distributed at a stable state, then the participants were measured by three different BIA instruments randomly. BFM and VFA were measured using IOI353, InBody230, and InBody770 and were expressed as BFMIOI353, BFMInBody230, BFMInBody770, as well as VFAIOI353, VFAInBody230, VFAInBody770, respectively.
Each participant was tested using the Lunar Prodigy DXA system (GE, USA) for measuring body fat mass. Participants were asked to wear a cotton gown and lay in a supine position on the DXA measuring table with both arms extended at their sides, while placing both feet together with their toes pointing upward. The subject stayed in this supine position on the DXA table for five minutes before the DXA measurement was made. The total body scan was made using enCore 2003 Version 7.0 software. Measurements derived by DXA were denoted as BFMDXA. On the day of measurement, prior to DXA scan, a standard calibration procedure was recommended by the manufacturer and implemented here.
For CT measurement, participants wore a cotton gown and lay in a supine position on the CT scanner with their arms extended overhead. The abdominal (L4-L5) CT scan was conducted using a Somatorn Sensation 64 CT system (Siemens Corp., Germany) equipped with software version Syngo CT2005A. Scanning was performed at 120 kV; 120 mAs; exposure and scanning times were 0.5 seconds. Slice thickness was 5 mm, and collimation was set at 1.5 mm. The acquired images were processed using a 3D-Doctor Ver 3.5 (Able Software Corp., MA, USA), following procedures suggested by Yoshizumi et al,4 to color visceral and abdominal fat in the calculated area, where CT threshold for fat tissue was set at −190±3 to −30±3 HU.
Statistical Analysis
The SPSS Ver. 18 (SPSS Inc., Chicago, IL, USA) and MedCalc Ver 19.6 (MedCalc Software Ltd, Mariakerke, Belgium) were used for statistical analyses. The data are presented as mean ±standard deviation. Repeated-measures ANOVA followed by Dunnett's post hoc pairwise comparison was used to test the mean differences between different measurement methods used for estimating VFA and BFM. Lin’s concordance correlation coefficient (ρc) was used to examine agreement between the BIA and reference method derived measures for VFA and BFM, respectively; ρc ranges from −1 to 1, with the perfect agreement at 1.24 The ordinary least products regression models of the predictive values of VFA and BFM estimates using different BIA devices and the values derived from the reference methods were also conducted, and the coefficient of determination (r2) and standard error of the estimates (SEE) were used to assess the model, as well as to differentiate fixed bias and proportional bias.25 We retrospectively calculated that a sample of 84 subjects provided 95% power at a significance level of 0.05, considering effect size of 0.4 (G*Power 3.1.9.2). Moreover, the Bland–Altman analyses were used to assess the degree of agreement between methods.26 The LOA is bias – .96 SD to bias +1.96 SD, and LOA (%) is the percentage ratio of 2⨰1.96 SD to the mean values of referential measurements. In addition, intraclass correlation coefficient (ICC) and coefficient of variation (CV%) were used to ensure the reliability of the impedance measures in BIA devices. The APE (absolute percentage error) was used for the comparison of multiple methods. Statistical significance was set at p<0.05.
Results
A total of 95 highly-ranked or national-level Taiwanese athletes were recruited. Participants were specialized in wrestling (24%), judo (25%), dancing (14%), track and field (17%) and soccer (20%). The mean (±SD) age of the subjects was 23.5 (±2.7) years (Table 1). Male participants were significantly taller and heavier than female participants but BMI was not significantly different between both sexes (Table 1).
 |
Table 1 Subjects Characteristics and Body Composition Estimates |
DXA was used as the reference method for BFM measure. The BFM measured by three different BIA models and DXA are showed in Table 1 and the correlations between BIA and DXA in BFM are summarized in Table 2. Regardless of which tool this measurement was taken, females had a greater amount of BFM than males. In men, BFM estimates using IOI353 (BFMIOI353) and InBody230 (BFMInBody230) were significantly higher compared to that of DXA (BFMDXA). In women, BFM estimates using all three BIA models were significantly lower than BFMDXA. There was a very strong linear correlation (r2=0.894 to 0.955 [r=0.946 to 0.977]) and a strong agreement (ICC=0.917 to 0.967) in BFM between BIA models and DXA. The scatter plots and regression analysis between BIA and DXA in BFM measures are shown in Figure 1. The SEE in BFM between IOI353, Inbody230 and Inbody770 were 2.956 kg, 2.028 kg, and 1.999 kg, respectively. Bland–Altman analysis showed that the LOA (%) of BFMInBody230, BFMInBody770, and BFMIOI35 was 89.3% and 60.3%, and 58.8%, respectively. The ordinary least products regression analysis indicated a fixed and proportional bias existed in BFMIOI353, BFMInBody230, and BFMInBody770 when compared with BFMDXA (Figure 2).
 |
Table 2 BIA Devises Estimation Results in Lin’s Concordance Correlation Coefficient ( |
CT was used as the reference method for VFA measure. The VFA measured by three different BIA models and DXA are showed in Table 1. In both sexes, all three BIA models overestimated VFA. The correlations between BIA and DXA in VFA are summarized in Table 2 and the scatter plots and regression analysis are shown in Figure 3. Sex differences were found for VFA between two InBody scanner (InBody230 and InBody770) and DXA but not for VFA between IOI350 and DXA. There was a very strong linear correlation (r2=0.706 to 0.728 [r=0.840 to 0.853]) and a moderate agreement (ICC=0.781 to 0.797) between two InBody scanners and DXA in VFA in men whereas in female, there was a low to fair linear correlation (r2=0.242 to 0.277 [r=0.492 to 0.526]) and a moderate agreement (ICC=0.781 to 0.797). The LOA (%) of VFA was also greater between InBody scanners and DXA in female than that of male. The ordinary least products regression analysis indicated a fixed and proportional bias existed in VFAInBody230, and VFAInBody770 when compared with VFADXA (Figure 4).
In contrast, there was no sex difference between IOI353 and DXA in the estimation of VFA. There was a moderate linear correlation (r2=0.442 to 0.455 [r=0.665 to 0.675]) and moderate agreement (ICC=0.659 to 0.674) between IOI353 and DXA in VFA for both men and female. The LOA (%) of VFA was also compatible between box sexes using IOI353 and DXA. A fixed bias between IOI353 and DXA in VFA is shown in Figure 4 in both sexes.
In this study, regression equations for predicting VFACT using BFMDXA were developed, showing a very strong correlation in male (r2=0.776 [r=0.881]) but fair correlation in female (r2=0.245 [r=0.494]).
In males, the equation was as below:
In females, the equation was as below:
The LOA of the above equation for VFA in male athletes was −75.53 to 63.82 cm2, ICC: 0.875 (95%CI: 0.789 to 0.927). The LOA of the equation for VFA in female athletes shown above was −108.93 to 81.85 cm2, ICC: 0.384 (95%CI: 0.104 to 0.607).
Discussion
In this study, statistical methods were applied to analyze the BFM and VFA estimates by three models standing 8-electrode BIA against established techniques in athletes. A very high correlation and strong agreement were demonstrated between BFM readings by the three BIA models and DXA in both sexes, indicating these devices have the potential to provide BFM measurement in athletes. Compared with the promising results of BFM measure by BIA, the VFA measure by BIA was less convincing. Furthermore, there was a gender difference for the relationships between BIA and CT in VFA measure. In male athletes a moderate to high correlation and moderate agreement were noted for the VFA values by BIA models compared to that of CT, whereas in female athletes there was only a low to moderate correlation and weak to moderate agreement between methods.
BIA has been utilized to assess body composition widely, and in all the components of body composition, the degree of abdominal visceral fat accumulation seems to be the most health-related one, because it is associated with metabolic abnormalities. Previous studies utilizing BIA in the assessment of VFA were primarily focused on the general population or the obese population, rarely on athletes. This study examined the agreement of different standing 8-electrode BIA instruments for estimating BFM and VFA compared with reference methods in athletes.
BIA has been used to assess body composition for its convenient, noninvasive, and rapid assessment. Moreover, it has been used widely in clinical, experimental, and epidemiological studies. The predictive models used to estimate fat mass have been considered as confidential information by manufacturers. However, whether BIA can deliver accurate and precise estimates in athletes remains to be determined. The current study aimed to examine the association between BIA and reference methods for the assessment of BFM and VFA in Taiwanese athletes. Although bias of BIA for assessing VFA compared with the reference method is generally higher than the bias of assessing BFM. Moreover, research has revealed that assessment of VFA in different populations when comparing the estimates with VFACT, BIA can still deliver satisfactory results. However, the results of our study show that it is not able to deliver acceptable results when assessing athletes.
In the current study, we used three different BIA instruments, two of which, BFMInBody230 and BFMInBody770, were manufactured by the same company (Biospace Co. Ltd) These two instruments generated slightly different results when assessing the same participant under the same controlled environment. However, when compared to the estimates that were acquired by reference methods (CT and DXA), results were similar. The results coincided with the findings by Anderson et al.27 BFMInBody230 and BFMInBody770 were highly correlated with BFMDXA. The results of SEE for BFMInBody230, BFMInBody770, and BFMIOI35 were 2.956, 2.028, and 1.999 kg, respectively.
Furthermore, Lin’s concordance correlation coefficient (CCC) between BFMInBody230 vs BFMDXA and BFMInBody770 vs BFMDXA were 0.964 and 0.957, respectively, suggesting agreement when comparing to BFMIOI353 vs BFMDXA (0.903). As for the estimation of VFA, the results of Lin’s concordance correlation coefficient and SEE indicated that agreements between VFA assessed using BIA devices and that done by CT were poor. The VFA estimated using BIA devices were not desirable.
Some studies have focused on examining the degree of agreement between different BIA instruments and reference methods by reporting LOA (relative difference in unit from standard; 95% CI) or LOA %.28,29 However, LOA (95%CI) can only reveal the difference in the range between the results of different BIA instruments compared with reference methods. When we tried to examine the agreement of BIA instruments with the results for reference methods, it was determined that reporting the difference as a percentage may be easier for us to understand. Therefore, we reported the degree of agreement by calculating LOA%. Considering that the participants were athletes, their BFM and VFA were generally lower than the general population or obese population. Therefore, LOA% tended to be higher due to the relatively lower means. Therefore, VFA measurements obtained using BIA devices had wider LOA% than that of BFM. Moreover, other statistical indicators such as Lin’s concordance correlation coefficient and the determined coefficients and standard errors of the estimate when using linear regression analysis also show VFA estimates obtained by BIA had substantial bias compared to that of BFM.
Taken together, the accuracy of the three different BIA instruments used for assessing VFA may still need improvements before they can be used for the assessment of athletes. Previously, studies have been more focused on assessing athletes’ lean body mass or skeletal muscle mass rather than fat mass. The current study aimed to examine agreements between standing 8-electrode BIAs and reference methods for assessing VFA and BFM, as well as to investigate the relationship between VFA and BFM. Smith et al,16 reported the relationship between VFA and BFM: the equations were VFA=3.65 BFM −18.0 (r2=0.641, female) and VFA=5.13 BFM –11.65 (r2=0.769, male). In the current study, we demonstrated the relationship between VFA and BFM: VFA=1.738 BFM +3.958 (r2=0.245, female) and VFA=2.549 BFM +3.153 (r2=0.776, male). Compared to the results of Smith et al,16 when assessing male subjects, we yielded a similar result for the determined coefficient; however, that study subjects were obese and were not athletes. However, when assessing female subjects, the devices in this study showed different results at the determined coefficient, intercept, and slope in the equation. Taken together, when assessing female athletes, using BFM alone to estimate VFA (r2=0.245) may not support consistent results.29
In this study, we also applied the BFM for establishing the equation of VFA in both male and female athletes, which had been rarely studied in current research for the relationship between BFM and VFA concerning male and female athletes. From the established VFA predictive equation or the validated outcomes in our study, the results showed that the correlation between VFA and BFM was stronger in the male athletes than that of the female athletes. Furthermore, regarding the application of BIA device on the estimation of VFA, some devices such as InBody230 and InBody770 also showed better predictive results for male athletes. Even though we do not have detailed information about the built-in equations of VFA in the BIA devices; the median APE results show no significant difference in the three BIA devices for estimating BFM. In this study, whether BFM and VFA showed wide ranges of LOA or other statistical analytical outcomes indicated that the BIA devices discussed in the study were not suitable for clinical application in athletes. The InBody230 and InBody770 had greater range of error for the estimated results in female athletes. Therefore, the application of initial screening for VFA has to proceed with caution.
As for the BIA devices investigated in this study, the predictive VFA of female athletes has more bias than the estimated results of male athletes. Similar results have been reported in other BIA and VFA studies.21,23 However, studies with different results have also been reported.22,28 When assessing an obese population, BIA tends to underestimate VFA.30 If VFA is estimated indirectly using BFM, studies from Smith et al,16 showed that the correlation between VFA and BFM in obese women is lower than in obese men. Hence, the accuracy of applying BIA to measure VFA in women may be lower than for men. When BIA was used to measure VFA, the variables such as height, weight, gender, impedance of different limbs, and frequency at different limbs, have different degrees of correlation with VFA. These related issues still require additional research and study for verification.
VFA has been shown to have a positive relationship with BFM and fat mass of the trunk.16,28 The results of the current study demonstrate that using BIA devices to assess BFM yields less biased results than VFA. All VFA measurements obtained by BIA devices differed from VFACT. The existing methods used in standing BIA devices for estimating fat mass can be calculated in two ways: by a predictive method using variables such as weight, height, age, and sex, or by a predictive method using direct measurements of the impedance in different body segments. Regardless of the predictive model used to estimate, when assessing VFA, the degree of correlation between VFA and predictive variables remain a concern. Furthermore, the placement of eight electrodes in standing BIA instruments are located at hands and feet that did not directly measure the resistance of the abdominal area; therefore, most BIA devices using indirect predictive methods from other variables such as body fat, percentage body fat, or other parameters to obtain estimates of VFA instead of using impedance measured at the abdominal area to derived VFA.12,19 A study has reported that only a moderate correlation exists between VFA obtained by standing BIA and with a reference method; r=0.605 (p<0.001, n=1006).21 Therefore, if increasing the accuracy of BIA in assessing VFA is the goal, a direct impedance measurement from the abdominal area similar to the DUALSCAN HDS-2000 (Omron Healthcare Co., Kyoto, Japan) may need to be applied. Park et al,31 reported that the correlation of VFA measurements obtained by DUALSCAN HDS-2000 and InBody720 with referenced CT were r=0.89 and r=0.64, respectively. The accuracy can also be improved by adding parameters regarding the abdominal area to the predictive model, such as those used by Yoneda et al,32 . In their study, the equation Dual 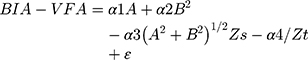 was used to determine VFA; where A, abdominal transverse diameter; B, abdominal anteroposterior diameter; Zs, surface impedance; Zt, truncal impedance; ε, residual constant; αi (i=1–4); αi is the parameter that estimated by the regression model. By including more variables that are related to the abdominal area, or the single-frequency electrical abdominal impedance applied by Scharfetter et al,33 the accuracy of standing BIA instruments when assessing VFA may be improved.
was used to determine VFA; where A, abdominal transverse diameter; B, abdominal anteroposterior diameter; Zs, surface impedance; Zt, truncal impedance; ε, residual constant; αi (i=1–4); αi is the parameter that estimated by the regression model. By including more variables that are related to the abdominal area, or the single-frequency electrical abdominal impedance applied by Scharfetter et al,33 the accuracy of standing BIA instruments when assessing VFA may be improved.
The areas measured for electrical impedance in this study included the entire body and individual extremities but not directly over the abdominal region. It is uncertain that if the electrical impedance obtained from extremities can be applied to estimate the fat area of the abdomen. Although the current research showed that the whole body BFM can be used to estimate VFA, whether the approach is applicable for athletes is still to be clarified.
Our study only recruited the elite active athletes in Taiwan as the research participants, so the results cannot be generalized to other ethnicities or athletes at different ages, such as adolescence and middle adulthood. Moreover, the sample size and sport specialization are the limitations of the study.
Conclusion
Our study tested the agreement of three different standing 8-electrode BIA devices for assessing body composition against reference methods in athletes. When assessing BFM, these instruments can deliver comparable measurements, and the degree of agreement ranged from excellent to moderate compared with the reference method. However, when assessing VFA, the agreements were weak. Therefore, the accuracy of standing 8-electrode BIA devices for assessing VFA still needs improvement before they can be applied to assess athletes.
Acknowledgments
This research was supported by the foundation of the Ministry of Health and Welfare, Taiwan.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Grundy SM. Metabolic syndrome: connecting and reconciling cardiovascular and diabetes worlds. J Am Coll Cardiol. 2006;47(6):1093–1100. doi:10.1016/j.jacc.2005.11.046
2. Alberti KG, Zimmet P, Shaw J. The metabolic syndrome- a new worldwide definition. Lancet. 2005;366(9491):1059–1062. doi:10.1016/S0140-6736(05)67402-8
3. Nakai R, Azuma T, Kishimoto T, et al. Development of a high-precision image-processing automatic measurement system for MRI visceral fat images acquired using a binomial RF-excitation pulse. Magn Reson Imagin. 2010;28(4):520–526. doi:10.1016/j.mri.2009.12.019
4. Yoshizumi T, Nakamura T, Yamane M, et al. Abdominal fat: standardized technique for measurement at CT. Radiology. 1999;211(1):283–286. doi:10.1148/radiology.211.1.r99ap15283
5. Berker D, Kopoaral S, Isik S, et al. Compatibility of different methods for the measurement of visceral fat in different body mass index strata. Diagn Inter v Radiol. 2010;16(2):99–105. doi:10.4261/1305-3825.DIR.2749-09.1
6. Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am J Clin Nutr. 2002;75(4):683–688. doi:10.1093/ajcn/75.4.683
7. Lane JT, Mack-Shipman LR, Anderson JC, et al. Comparison of CT and dual-energy DEXA using a modified trunk compartment in the measurement of abdominal fat. Endocrine. 2005;27(3):295–299. doi:10.1385/ENDO:27:3:295
8. Romero-Corral A, Somers VK, Sierra-Johnson J, et al. accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes. 2008;32:959–966. doi:10.1038/ijo.2008.11
9. Kanellakis S, Skoufa E, Khudokonenko V, et al. Development and validation of two equation based on anthropometry, estimating body fat for the Greek adult population. Obesity. 2017;25:408–416. doi:10.1002/oby.21736
10. Dehghan M, Merchant AT. Is bioelectrical impedance accurate for use in large epidemiological studies? Nutr J. 2008;7:26. doi:10.1186/1475-2891-7-26
11. Ryo M, Maeda K, Onda T, et al. A New simple method for the measurement of visceral fat accumulation by bioelectrical impedance. Diabetes Care. 2005;28(2):451–453. doi:10.2337/diacare.28.2.451
12. Yamada M, Moriguch Y, Mitani T, Aoyama T, Arai H. Age-dependent changes in skeletal muscle mass and visceral fat area in Japanese adults from 40 to 79 years-of-age. Geriatr Gerontol Int. 2014;14(Suppl. 1):8–14. doi:10.1111/ggi.12209
13. Ward LC, Heitmann BL, Craig P, et al. Association between Ethnicity, body mass index, and bioelectrical impedance: implications for the population specificity of prediction equations. Ann NY Acad Sci. 2000;904:199–202. doi:10.1111/j.1749-6632.2000.tb06449.x
14. Jaffrin MY, Morel H. Body fluid volumes measurements by impedance: A review of bioimpedance spectroscopy (BIS) and bioimpedance analysis (BIA) methods. Med. Eng Phys. 2008;30(10):1257–1269. doi:10.1016/j.medengphy.2008.06.009
15. Zemski AJ, Slater GJ, Broad EM. Body composition characteristics of elite Australian rugby union athletes according to playing position and ethnicity. J Sports Sci. 2015;33:970–978. doi:10.1080/02640414.2014.977937
16. Smith SR, Lovejo JC, Greenway F, et al. Contributions of total body fat, abdominal subcutaneous adipose tissue compartments, and visceral adipose tissue to the metabolic complications of obesity. Metabolism. 2001;50(4):425–435. doi:10.1053/meta.2001.21693
17. Nye NS, Camahan D, Jackson JC, et al. Abdominal circumference is superior to body mass index in estimating musculoskeletal injury risk. Med Sci Sports Exerc. 2014;46(10):195–199. doi:10.1249/MSS.0000000000000329
18. Nagai M, Komjya H, Mori Y, Ohta T, Kasahara Y, Ikeda Y. Development of a new method for estimating visceral fat area with multi-frequency bioelectrical impedance. Tohoku J Exp Med. 2008;214(2):105–112. doi:10.1620/tjem.214.105
19. Shimomura M, Kodama M, Sato H Method and system for estimating visceral fat area. United States patent US 6,920,352 B2. 2005 Jul 15.
20. Lu HK, Chen YY, Yeh C, et al. Discrepancies between leg-to-leg bioelectrical impedance analysis and computerized tomography in abdominal visceral fat measurement. Sci Rep. 2017;7(1):9102. doi:10.1038/s41598-017-08991-y
21. Lee DH, Park KS, Ahn S, et al. Comparison of abdominal adipose tissue area measured by computed tomography with that estimated by bioelectrical impedance analysis method in Korean subjects. Nutrients. 2015;7(12):10513–10524. doi:10.3390/nu7125548
22. Lia CC, Lu HK, Chiang LM, Chiang J, Hsieh KC, Lai CL. Evaluation of a leg-to-leg bioimpedance device in the estimation of abdominal visceral fat for the elderly-comparison with CT. Int J Geron. 2017;11(3):144–148. doi:10.1016/j.ijge.2016.03.013
23. Browning LM, Mugridge O, Chatfield MD, et al. Validity of a new abdominal bioelectrical impedance device to measure abdominal and visceral fat: comparison with MRI. Obesity. 2010;18(12):2385–2391. doi:10.1038/oby.2010.71
24. Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45(1):255–268. doi:10.2307/2532051
25. Ludbrook J. Statistical techniques for comparing measures and methods of measurement: a critical review. Clin Exp Phamacol Physiol. 2002;29:527–536. doi:10.1046/j.1440-1681.2002.03686.x
26. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. doi:10.1016/S0140-6736(86)90837-8
27. Anderson LJ, Erceg DN, Schroeder ET. Utility of multi-frequency bioelectrical impedance compared with dual-energy x-ray absorptiometry for assessment of total and regional body composition varies between men and women. Nutr Res. 2012;32(7):479–485. doi:10.1016/j.nutres.2012.05.009
28. Wang JG, Zhang Y, Chen HE, et al. Comparison of two bioelectrical impedance analysis devices with dual energy X-ray absorptiometry and magnetic resonance imaging in the estimation of body composition. J Strength Cond Res. 2013;27(1):236–243. doi:10.1519/JSC.0b013e31824f2040
29. Bosy-Westphal A, Jensen B, Braun W, Pourhassan M, Gallagher D, Müller MJ. Quantification of whole-body and segmental skeletal muscle mass using phase-sensitive 8-electrode medical bioelectrical impedance devices. Eur J Clin Nutr. 2017;71(9):1061–1067. doi:10.1038/ejcn.2017.27
30. Neovius M, Hemmingsson E, Freyschuss B, Uddén J. Bioelectrical impedance underestimates total and truncal fatness in abdominally obese women. Obesity. 2006;14(10):1731–1738. doi:10.1038/oby.2006.199
31. Park KS, Lee DH, Lee JE, et al. Comparison between two method methods bioelectrical impedance analyses for accuracy in measuring abdominal visceral fat area. J Diabetes Complications. 2016;30(2):343–349. doi:10.1016/j.jdiacomp.2015.10.014
32. Yoneda M, Tasaki H, Tsuchiya N, et al. A study of bioelectrical impedance analysis methods for practical visceral fat estimation. In:
33. Scharfetter H, Schlager T, Stollberger R, Felsberger R, Hutten H, Hinghofer-Szalkay H. Assessing abdominal fatness with local bioimpedance analysis: basics and experimental findings. Int J Obes Relat Metab Disord. 2001;25(4):502–511. doi:10.1038/sj.ijo.0801556
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.







