Back to Journals » Vascular Health and Risk Management » Volume 15
Stability of thromboxane in blood samples
Authors Helgadóttir H , Ólafsson Í, Andersen K, Gizurarson S
Received 12 February 2019
Accepted for publication 1 May 2019
Published 4 June 2019 Volume 2019:15 Pages 143—147
DOI https://doi.org/10.2147/VHRM.S204925
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Takashi Kajiya
Helga Helgadóttir,1,2 Ísleifur Ólafsson,2 Karl Andersen,3 Sveinbjörn Gizurarson1
1Faculty of Pharmaceutical Sciences, University of Iceland, Reykjavik, Iceland; 2Department of Clinical Biochemistry, Landspitali University Hospital, Reykjavik, Iceland; 3Faculty of Medicine, University of Iceland, Reykjavik, Iceland
Introduction: Conventional venous blood collection requires a puncture with a needle through the endothelium of a vessel. The endothelial injury causes activation of circulating platelets and the release of thromboxane A2. The aim of the study was to investigate if platelets continue to form thromboxane A2 in the blood tube after sample collection, but such synthesis would give false information about the actual circulating thromboxane A2 value.
Methods: Thromboxane B2 is a biologically inactive but stable metabolite of thromboxane A2 and can be measured in blood samples by a standard enzyme immunoassay. Thromboxane B2 measurements reflect thromboxane A2 concentration. Blood samples were collected in 3.2% sodium citrate vials and EDTA vials from ten individuals and centrifuged and frozen at different time points (0, 30, and 120 minutes). Plasma aliquots were transferred to and frozen in 1.8 mL polypropylene tubes and the citrate samples were also transferred to and frozen in propylene tubes containing indomethacin.
Results: Concentrations of thromboxane B2 in plasma samples collected in citrate vials and stored in propylene tubes increased very rapidly as the samples were left for longer after sampling and allowed to stand at room temperature. After 120 minutes, the amount of thromboxane B2 was 400% higher than in the reference sample at time zero. In comparison, thromboxane B2 concentration was about 200% higher in the 120-minute samples compared to the reference in samples collected in citrate vials but stored in indomethacin tubes. In samples collected in EDTA vials, a 10% reduction in thromboxane B2 concentration in the 120-minute samples was observed.
Conclusion: Storage conditions, type of sampling vial and time from sampling until sample processing (centrifuging) has a major impact on thromboxane B2 stability.
Keywords: thromboxane A2, thromboxane B2, stability, platelet function
Introduction
Platelets or thrombocytes are disk-shaped cells circulating in the blood stream with a lifespan of about 10 days. They have no cell nucleus and are produced by megakaryocytes in the bone marrow.1 A normal platelet count ranges from 150 to 400×109/L1,2 and they are involved in the initial cellular response to endothelial damage and repairing the vessel. Platelet function that depends on platelet thromboxane production can be determined by measuring platelet thromboxane A2 (TxA2) release.3 Activated platelets convert arachidonic acid to TxA2 by the enzyme cyclooxygenase (COX-1).4 TxA2 stimulates platelet aggregation as well as smooth muscle contraction.5 Consequently, TxA2 has both prothrombic properties as well as being a potent vasoconstrictor.
Measuring thromboxane in blood samples is useful for evaluating the efficacy of acetylsalicylic acid (aspirin) since it inhibits irreversibly the platelet COX, preventing the formation of prostaglandin H2 and therefore TxA2.6
TxA2 is very unstable under physiological conditions and is rapidly degraded into an inactive metabolite called thromboxane B2 (TxB2).4 TxA2 has a half-life of about 30 seconds, where TxB2 has a half-life of 5–7 minutes whereafter it is rapidly metabolized to urinary metabolites such as 11-dehydrothromboxane B2. Due to the ultra-short half-life TxA2 cannot be analyzed in blood samples. TxB2 and 11-dehydrothromboxane B2, however, can be measured with various methods such as gas and liquid chromatography, mass spectroscopy and enzyme immunoassays. The concentrations of TxB2 or the urinary metabolite 11-dehydrothromboxane B2 are used to reflect the levels of its source, TxA2.3,7
The collection of a blood sample requires a puncture through the endothelium of a vessel with a needle, resulting in that local platelets are activated and start to produce TxA2. The platelets that are collected into the tube are, therefore, in an activated state and may continue to produce TxA2 inside the tube. This may give false information about the true TxA2 value in the circulation.
The aim of this study was to study the stability of TxB2 in blood samples by measuring possible exnuovo production of TxA2 in blood samples. Samples were collected in two different blood tubes and consequently processed and frozen at different time points. TxB2 concentration was then measured using standardized enzyme immunoassay. Optimizing a method for handling platelets is complicated, involving many different factors, including heat sensitivity, time-dependent differences and factors due to anticoagulants and plasma preparation.8,9 The method used in this study was set up based on standard procedures recommended by the Clinical Department of the Icelandic University Hospital, Landspitali.
Materials and methods
The study was approved by the Ethics Committee at Landspitali University Hospital in Iceland (No. 22/2016). All participants provided written informed consent after receiving information about the study in accordance with the Declaration of Helsinki.
Blood sample collection and preparation
Ten healthy volunteers with body mass index (BMI) under 30 kg/m2 participated in the study. All participants were free of any medication considered to affect the coagulation process, such as aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) at least one week prior to participation in the study and all participants were nonsmokers. Blood samples from each participant were collected in a total of seven blood tubes; (i) three Vacuette® blood tubes (Greiner Bio-One GmbH, Kremsmünster, Austria) containing 3.2% sodium citrate; and (ii) four tubes containing EDTA. One of the EDTA blood samples was collected to measure complete blood count using Sysmex XE-5000 hematology instrument (Sysmex XE-5000 analyzer; Sysmex, Kobe, Japan). The other six samples were centrifuged at 3,200 rpm for 14 minutes at 4°C.
After centrifugation, the plasma was aliquoted into 1.8 mL polypropylene tubes or in sampling tubes containing 10 µm indomethacin (Cayman Chemicals, Ann Arbor, MI, USA, No. 10,951). Indomethacin is a COX inhibitor that prevents ex-vivo thromboxane formation that cannot be prevented using anticoagulant alone. The samples stored in tubes containing indomethacin were stored frozen at −20°C. Samples stored in polypropylene tubes were frozen immediately in dry ice and then stored at −80°C.
The whole blood samples collected in vials containing citrate, and three of the whole samples collected in EDTA vials were centrifuged and plasma aliquoted at following times: Right after blood collection (0 minutes), 30 minutes, and 120 minutes after blood withdrawal (samples were allowed to stand at room temperature (23°C) until centrifugation).
TxB2 measurements
Concentration of TxB2 was measured using commercially available reagents from Cayman Chemicals (Ann Arbor, MI, USA), No. 501020. The measuring method is a competitive enzyme immunoassay (EIA) based in the competition between TxB2 and a TxB2-acetylcholinesterase (AChE) conjugate (TxB2 tracer) for a limited number of TxB2-specific rabbit antiserum binding sites. The concentration of the TxB2 tracer is held constant, thus the concentration of TxB2 is inversely proportional to the concentration of TxB2 on the well. The method can be used for quantification of TxB2 in urine, serum, plasma, culture media samples, and other sample matrices. Plasma (citrate and EDTA) was used in this study. The EIA displays an IC50 of approximately 60 pg/mL and has a detection limit of 5 pg/mL. Standards, buffers, washing buffer, and all other solutions supplied with the kits were used as recommended from the manufacturer.3
Statistics
To get 80% power in the study with 5% acceptance for type 1 error, number of subjects were calculated based on statistical method for qualitative outcome.10 The p1 value was defined as zero (proportion of the control expected to be more than zero), since subjects act as their own control. The p2 value was set to 50% (proportion of the study group expected to show change compared to control). Total number of subjects needed based on the calculations were eight. Since sampling, measurement and quantification of TxB2 is a very delicate procedure two more participants were added to the study, resulting in a total of ten volunteers participating in the study.
Results are expressed as percentage change from the reference (0 minutes) sample. Results are expressed as mean ±SEM of N were N is the number of participants. Student's t-test was used to analyze the difference in relative concentration of TxB2 between groups and P<0.05 was considered as significant.
Results
Total number of participants were ten, six females and four males. Table 1 summarizes the main characteristics of the participants in the study. Blood status values of all participants were within normal range. No correlation was found between platelet count and the TxB2 levels.
 | Table 1 Characteristics of participants in the study |
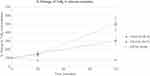
Figure 1 shows that both the type of blood vials (citrate or EDTA) and the storage conditions (with or without indomethacin) of the plasma samples are important for TxB2 measurements. The individual variation was found to be high, especially for samples collected in citrate tubes and stored in the empty polyethylene tubes.
Citrate plasma samples stored in the empty polyethylene tubes (cit-emp) showed 40% increase in TxB2 levels in samples processed after 30 minutes compared to the reference sample at time zero. In the 120-minute samples, however, the increase reached an average of 400% compared to the time zero sample.
Citrate plasma samples stored in indomethacin tubes (cit-indo) were more stable compared to the cit-emp samples. The increase was found to be similar (Figure 1) in the 30-minute cit-indo and cit-emp samples. However, in the 120-minute samples the increase in the cit-indo was about 200% compared to the reference sample. There was a statistical difference between the cit-emp and cit-indo storage tubes in the 120-minute samples (P=0.038).
EDTA plasma samples had the least variation, where there was on average no increase in the TxB2 concentration over the studied range. On the contrary, there was about 10% decrease in the concentration detected at 30 minutes and 120 minutes compared to the zero sample. The difference at 120 minutes was statistically significant when compared to cit-emp (P<0.001) and compared to cit-indo (P=0.001) samples.
Discussion and conclusion
The results indicate that the time from sampling to storage is an important factor for thromboxane B2 stability. The type of sampling tubes as well as the storage conditions were also found to have a great impact on the true TxB2 in the blood samples.
The cit-emp tubes showed up to 400% increase in TxB2 concentration, indicating that there is a significant ex-nuovo formation of TxB2 after the samples have been collected and frozen. The cit-indo tubes also showed a high increase in the TxB2 formation post sampling, although the indomethacin tubes showed less TxB2 formation compared to the cit-emp tubes.
Interestingly, there was no ex-nuovo TxB2 formation in the EDTA plasma samples even though these samples were stored in polypropylene tubes containing no indomethacin. Citrate and EDTA are both anticoagulants used in vitro to prevent clot formation in blood samples. Calcium is essential for normal platelet adherence and for a wide range of enzyme reactions of the coagulation cascade. Removing it prevents blood clotting within the blood collection tube.11 EDTA is a polyprotic acid containing four carboxylic acid groups and two amine groups with lone-pair electrons that chelate calcium and several other metal ions in 1:1 metal-EDTA complexes.12 Sodium citrate is the sodium salt of citric acid with alkalinizing activity. Citrate also acts by removing calcium from the blood sample, but unlike EDTA, it is reversible. Residual calcium ions are not expected to be present in samples in the EDTA tube since the excess amount of EDTA irreversibly forms 1:1 complex with calcium ions in the sample. When collecting blood samples in sodium citrate tubes the ratio between the blood sample (thus calcium) and sodium citrate in the tube is important. If the ratio is shifted residual calcium ions are expected to be present. This possible imbalance was minimized by filling the tube with enough whole blood, and by trying to have the amount as equal as possible between each tube.
Previous study suggested that EDTA is capable of penetrating biological membranes such as plasma membranes to chelate intracellular calcium to prevent platelet activation.13 However further studies have shown that in vitro activation does occur in EDTA-anticoagulated blood.8 Thus, the extent of this factor on the overall results of this particular study is not clear.
In conclusion, these results are interesting since both citrate and EDTA are able to bind calcium ions in the blood. The different mechanism behind the calcium removal in the blood sample might play a crucial role in the stability of TxB2 in the samples. It has also been shown that acidity has an effect on the coagulation, where lowering the pH reduces coagulation.14 The acidity of the plasma might also be of importance. These results are important for future analysis and work with TxB2.
Acknowledgments
This study was supported by a grant from the Icelandic research fund (Rannis). Cayman Chemicals kindly provided equipment for this study. The authors also thank Landspitali University Hospital in Iceland for the facilities used.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Thon JN, Italiano JE. Platelet Formation. Semin Hematol. 2010;47(3):220–226. doi:10.1053/j.seminhematol.2010.03.005
2. Schmitt A, Guichard J, Masse JM, Debili N, Cramer EM. Of mice and men: comparison of the ultrastructure of megakaryocytes and platelets. Exp Hematol. 2001;29(11):1295–1302.
3. Rozalski M, Watala C, Golanski J. Various laboratory protocols for measuring thromboxane A2 generation to detect the effectiveness of acetylsalicylic acid therapy: a comparative study. Blood Coagul Fibrin. 2014;25(1):46–51. doi:10.1097/MBC.0b013e32836551b5
4. Hamberg M, Svensson J, Samuelsson B. Thromboxanes - new group of biologically-active compounds derived from prostaglandin endoperoxides. P Natl Acad Sci USA. 1975;72(8):2994–2998. doi:10.1073/pnas.72.8.2994
5. Yabe M, Sako M, Yabe H, et al. A conditioning regimen of busulfan, fludarabine, and melphalan for allogeneic stem cell transplantation in children with juvenile myelomonocytic leukemia. Pediatr Transplant. 2008;12(8):862–867. doi:10.1111/j.1399-3046.2008.00931.x
6. Roth GJ, Stanford N, Majerus PW. Acetylation of prostaglandin synthase by aspirin. P Natl Acad Sci USA. 1975;72(8):3073–3076. doi:10.1073/pnas.72.8.3073
7. Hankey GJ, Eikelboom J. Aspirin resistance. Lancet. 2006;367(9510):606–617. doi:10.1016/S0140-6736(06)68040-9
8. Mussbacher M, Schrottmaier WC, Salzmann M, et al. Optimized plasma preparation is essential to monitor platelet-stored molecules in humans. PLoS One. 2017;12(12). doi:10.1371/journal.pone.0188921
9. Zhang JN, Wood J, Bergeron AL, et al. Effects of low temperature on shear-induced platelet aggregation and activation. J Trauma. 2004;57(2):216–223.
10. Enderlein G, Pocock SJ. Clinical Trials — a practical approach. John Wiley & Sons, Chichester — New York — Brisbane — Toronto — Singapore 1983, 265 S., £ 16.95. Biometrical Journal. 1985;27(6):634. doi:10.1002/bimj.4710270604
11. Mikaelsson ME. The Role of Calcium in Coagulation and Anticoagulation. Developments in Hematology and Immunology. Vol. 26. Boston, MA: Springer; 1991.
12. Banfi G, Salvagno GL, Lippi G. The role of ethylenedimine tetraacetic acid (EDTA) as in vitro anticoagulant for diagnostic purposes. Clin Chem Lab Med. 2007;45(5):565–576. doi:10.1515/CCLM.2007.110
13. Ogundele MO. Bimodal role for divalent cations in the mechanism of EDTA cytolysis. Brit J Biomed Sci. 2000;57(4):312–315.
14. Green FW, Kaplan MM, Curtis LE, Levine PH. Effect of acid and pepsin on blood-coagulation and platelet-aggregation - possible contributor to prolonged gastroduodenal mucosal hemorrhage. Gastroenterology. 1978;74(1):38–43.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.