Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Spatial Distribution and Factors Associated with Multiple Sexual Partnerships among Reproductive-Aged Men in Ethiopia: A Spatial and Mixed-Effect Analysis of the 2016 Ethiopian Demographic and Health Survey
Authors Teshale AB , Worku MG , Tesema GA
Received 13 March 2021
Accepted for publication 28 April 2021
Published 31 May 2021 Volume 2021:13 Pages 593—604
DOI https://doi.org/10.2147/HIV.S311020
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Achamyeleh Birhanu Teshale,1 Misganaw Gebrie Worku,2 Getayeneh Antehunegn Tesema1
1Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 2Department of Human Anatomy, University of Gondar, College of Medicine and Health Science, School of Medicine, Gondar, Ethiopia
Correspondence: Achamyeleh Birhanu Teshale Email [email protected]
Background: Though multiple sexual partnerships (MSPs) increase the risk of acquiring sexually transmitted diseases, such as HIV/AIDS, they are still common in sub-Saharan Africa, particularly in Ethiopia. Therefore, this study aimed to investigate spatial distribution and factors associated with MSPs among reproductive-age men in Ethiopia.
Methods: This study was based on Ethiopian Demographic and Health Survey 2016 data. A total weighted sample of 12,688 men aged 15– 59 years was included. Spatial analysis was conducted using Arc GIS 10.3 and SaTScan 9.6 statistical software. Mixed-effect logistic regression analysis was used to estimate the association between MSPs and independent variables. Variables with p< 0.05 on multivariable mixed-effect analysis were considered significant predictors of MSPs.
Results: MSPs had significant variations across the country (global Moran’s I=0.109, p< 0.001). The primary-cluster spatial window was located in the southwest Oromia and Somalia regions, withrelative risk of 3 and log-likelihood ratio of 24.49 (P< 0.001). Age 20– 29 years (AOR 2.79, 95% CI 1.83– 4.26), 30– 39 years (AOR 4.04, 95% CI 2.48– 6.58), and 40– 59 years (AOR 7.13, 95% CI 4.36– 11.68), never married (AOR 1.54, 95% CI 1.13– 2.08), femle-headed household (AOR 1.90, 95% CI 1.48– 2.44), Internet usage (AOR 1.62, 95% CI 1.21– 2.17), ever chewing khat (AOR 1.72, 95% CI 1.37– 2.18), ever drinking alcohol (AOR 2.31, 95% CI 1.74– 3.08), and being from regions other than Tigray, Harari, and Dire Dawa were significant factors associated with increased odds of MSPs.
Conclusion: MSPs showed significant variations across the country, with the primary-cluster spatial window located in Oromia and Somalia regions. Therefore, special attention should be paid to high-risk regions and groups, particularly those who are unmarried and substance users, to decrease MSPs and their serious consequences, such as HIV and other sexually transmitted infections.
Keywords: multiple sexual partnership, spatial distribution, mixed-effect analysis, Ethiopia
Background
Risky sexual behaviors are defined as any sexual activity (sexual initiation at an early age, having multiple sexual partners, having sex while under the influence of alcohol or drugs, and unprotected sexual behaviors) that put a person at risk of developing sexually transmitted infections (STIs), such HIV.1–3 A multiple sexual partnership (MSP) is defined as having two or more sexual partners, and is a major public-health issue in many countries, especially in sub-Saharan Africa.4–6 Practicing sex with multiple partners exposes one to an increased risk of acquiring STIs, which may in turn lead inability to conceive/infertility and miscarriage.4,7–10 In addition, increased numbers of nonmarital sexual partners can result in loss of happiness and other mental health consequences, such as higher rates of anxiety and depression and decreased quality of relationships with family, friends, and the community in general.11,12 Despite its negative health outcomes, many men nowadays have MSPs. According to a previous study in sub-Saharan Africa, the prevalence of male MSPs ranges up to 29%.13–15 In Ethiopia, the prevalence of MSPs among reproductive-aged men is 3%–54.1%.16–18 Evidence has revealed that such factors as education, occupation, age, substance abuse, religion, wealth, media exposure, age at first sexual intercourse, residence, and region are associated with MSPs.14,15,19–29
Male MSPs are the leading cause of the spread of HIV in sub-Saharan Africa.13 Even though having MSPs causes a substantial adverse effect on the health of women and men, spatial distribution and determinants of MSPs remain poorly understood in Africa, particularly in Ethiopia. We concentrate on MSPs in reproductive-aged men in Ethiopia because men have greater involvement and influence in such risky sexual behavior than women, and prevention of MSPs among men will have an appreciable effect on preventing MSPs among women.30 Therefore, we aimed to investigate spatial distribution and factors associated with MSPs among reproductive-aged men in Ethiopia. Since this study is based on nationally representative data and incorporates spatial analysis, which is important in identifying high-risk areas for MSPs, it will have great advantage in informing policy-makers and governmental and nongovernmental organizations to initiate appropriate interventions.
Methods
Study Area and Period
This study was based on data from the Ethiopian Demographic and Health Survey (EDHS) 2016, which was conducted from January 18 to June 27, 2016. Ethiopia is divided into nine regional states (Tigray, Afar, Amhara, Oromia, Somali, Benishangul-Gumuz, Southern Nations Nationalities and People Region (SNNPR), Gambela, and Harari) and two chartered cities (Addis Ababa and Dire Dawa), and is one of the most populous countries in the Horn of Africa. The regional states aand two chartered cities are further divided into 68 zones, 800 woredas, and around 15,000 kebeles (the lowest administrative unit of Ethiopia). According to Worldometer, the population of Ethiopia is >117 million, of which 49.8% are male.
Study Design and Sampling
The 2016 EDHS was a community-based cross-sectional study and stratified and selected in two stages using 84,915 enumeration areas (EAs) created for the 2007 PHC as a sampling frame. A total of 645 enumeration areas — 202 in urban areas and 443 in rural areas — were selected in the first stage and a fixed number of 28 households per each newly formed cluster were selected in the second stage of selection. All women agedf 15–49 years and all men aged 15–59 years were eligible for the interview.31 The current study comprised a weighted total sample of 12,688 men aged 15–59 years.
Measurement of Variables
Outcome Variable
An MSP was defined as having two or more sexual partners during the 12 months preceding the survey. This was coded “1” when the respondent mentioned two or more sexual partners and “0” when there was no more than one sexual partner.
Independent Variables
Independent variables were age, educationl, working status, religion, marital status, sex of household head, household wealth, age at first sex, radio and television consumption, Internet use, chawing khat (ever), use of alcohol (ever), ever tested for HIV, ever heard of HIV/AIDS, residence, and region.
Data Management and Analysis
Data extraction, further coding, and analysis were done using Stata 14. Weighting was done to make the data representative, as well as to consider the nonresponse rates and to get appropriate statistical estimates. Since the EDHS has a hierarchical structure and samples were taken using multistage sampling, intra-class correlation coefficient (ICC) was estimated to assess the clustering effect. The ICC revealed that there was a significant clustering effect, and thus we employed mixed-effect logistic regression analysis. Bivariable analysis was done first to screen variables for multivariable analysis, and those variables with P<0.2 in the bivariable analysis were considered for multivariable analysis. Model fitness was checked using deviance, and the model with the lowest deviance was considered the best-fit model. Finally, AORs with 95% CIs were calculated, and variables with P<0.05 on multivariable mixed-effect analysis were considered significant predictors of MSPs.
Spatial Analysis
Spatial analysis was conducted using Arc GIS 10.3 and SaTScan 9.6 statistical software. Global spatial autocorrelations to ascertain whether MSPs were clustered, dispersed, or random across the country, were calculated using the global Moran I statistic.32 Kriging spatial interpolation was used to predict the magnitude of MSPs in unsampled/unmeasured areas based on the values from sampled measurements. Getis-Ord Gi* statistical hots-pot analysis was used to identify significant hot spots (areas with higher rates of MSPs) and cold spots (areas with lower rates of MSPs).
Since the outcome variable was binary, we used Bernoulli-based spatial scan statistical analysis to detect statistically significant spatial clusters using SaTScan 9.6.33 To fit the model, men with MSPs were taken as cases and those without MSPs were taken as controls. A default maximum spatial cluster <50% of the population was used as the upper limit for detecting both small and large clusters. Log-likelihood ratios (LLRs) statistic were used to determine if the number of observed cases within the potential cluster was significantly higher than expected or not. Primary and secondary clusters were identified and P-values assigned and ranked using LLRs based on 999 Monte Carlo replications. Areas with the highest LLRs and significant P-values were considered high-risk areas/clusters, and the spatial window with the highest LLR was defined as the most likely (primary) cluster spatial window.
Results
Sociodemographic Characteristics of Respondents
The mean age of participants were 31±11 years. Most (46.51%) had primary education, and 92.51% had a job. A majority (44.84%) were followers of the Orthodox Christian religion, 58.88% were married, and 87.66% were from male-headed households. A majority (55.65%) had their first sexual intercourse aged ≥18 years, and only 12.38% used the Internet. Less than half (46.30%) had ever drunk alcohol, and 26.94% had a history of chawing khat. More than half (54.31%) had never been tested for HIV, and 97.70% had heard about HIV/AIDS, while 80.29% and 37.50% were from a rural area and Oromia region, respectively (Table 1).
 |
Table 1 Sociodemographic characteristics of respondents (n=12,688) |
Spatial Analysis of MSPs among Reproductive-Aged Men in Ethiopia
Spatial Distribution
The spatial distribution of MSPs had significant variations across the country (I=0.109, P<0.001). As shown in the green clusters in Figure 1, higher prevalence of MSPs among reproductive-aged men was found in the Afar, Somali, Benishangul, and Gambela regions. Areas with lower MSP prevalence were located in Amhara, Oromia, Harari, Dire Dawa, and Tigray regions, as indicated by red clusters (Figure 1).
 |
Figure 1 Spatial distribution of MSPs among reproductive-aged men in Ethiopia, 2016. |
Kriging Spatial Interpolation
Based on Kriging interpolation, southwestern Oromia, southwestern and eastern parts of Somalia, and western Afar had higher predicted MSP prevalence. Amhara, Tigray, Dire Dawa, and Harari had lower predicted MSP prevalence (Figure 2).
 |
Figure 2 Kriging interpolation of MSPs among reproductive-aged men in Ethiopia, 2016. |
Hot-Spot and Cold-Spot Analysis
Figure 3 shows regions with red clusters (central Afar, southwest Benishangul, all Gambela, southwest Oromia, and southwest and eastern Somalia) were the significant hot-spot areas. Regions with blue clusters (all Amhara, Tigray, Dire Dawa, and Harari regions) indicate significant cold-spot areas.
 |
Figure 3 Hot-spot and cold-spot analysis of MSPs in reproductive-aged men in Ethiopia, 2016. |
SaTScan Analysis
Figure 4 shows the SaTScan analysis. Of the total 622 clusters included, 115 significant clusters were identified. Of these, 27 significant clusters were primary (most likely) and the rest secondary. The primary-cluster spatial window were located in southwest Oromia and Somalia regions with 336.89 km radius and relative risk (RR) of 3, as well as LLR of 24.49 (P<0.001). This can be interpreted as men within the spatial window had three times higher likelihood of MSPs as compared to those outside the spatial window. The secondary clusters were located in Gambela and Benishangul regions.
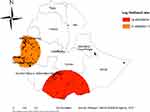 |
Figure 4 Identified significant SaTScan clusters of areas with higher proportions of men having MSPs in Ethiopia, 2016. |
Random Effect and Model Fitness
As shown in Table 2, the ICC in the null model (the model containing only the outcome variable) was 0.19, showing about 19% of total variation in MSPs was attributable to differences among clusters/communities. Regarding model fitness, the final model (the model containing both the outcome variable and all independent variables) that had the lowest deviance was the best fit(Table 2).
 |
Table 3 Bivariable and multivariable mixed-effect logistic regression analysis for factors associated with MSPs among men in Ethiopia, 2016 |
 |
Table 2 Random effect (community-level variability) and model fitness |
Factors Associated with MSPs among Reproductive-Aged Men in Ethiopia, 2016
On bivariable analysis, age, occupation, religion, marital status, wealth, sex of household head, age at first sex, listening to the radio, Internet use, ever chewing khat, smoking, ever drinking Alcohol, ever been tested for HIV, residence, and region were associated with MSPs (P<0.20), while on multivariable analysis, age, marital status, sex of household head, Internet use, ever chewing khat, ever drinking Alcohol, and region were significant factors associated with MSPs (P<0.05). The odds of having MSPs were 2.79 (95% CI 1.83–4.26), 4.04 (95% CI 2.48–6.58), and 7.13 (AOR 7.13, 95% CI 4.36–11.68) times among men aged 20–29, 30–39, and 40–59 years than men aged 15–19 years. Never-married men had 1.54 (95% CI 1.13–2.08) times higher odds of having MSPs than married men. Men from female-headed households had 1.90 (95% CI 1.48–2.44) times higher odds of having MSPs as compared to their counterparts. Internet users had 1.62 (95% CI 1.21–2.17) times higher odds of having MSPs as compared to nonusers. Regarding khat and alcohol use, the odds of having MSPs were 1.72 (95% CI 1.37–2.18) and 2.31(AOR 2.31, 95% CI 1.74,3.08) times higher among those who had ever chawed Khat and ever drunk Alcohol, respectivelly, as compared to those who had no such history. In addition, men from regions other than Tigray, Harari, and Dire Dawa had higher odds of having MSPs than those from the Amhara region (Table 3).
Discussion
In this study, we found that MSPs are not random and had spatial variation in Ethiopia. In the SaTScan analysis, the primary clusters were located in Oromia and Somalia regions with a 336.89 km radius and RR of 3 and LLR 24.49 (P<0.001). This regional difference is congruent with a worldwide study that reported huge regional variation in risky sexual behaviors, including having MSPs,34 and a study in sub-Saharan Africa.29 Furthermore, this regional variation is supported by this research by the mixed-effect logistic regression analysis, which revealed that these regions were more likely for MSPs. A potential reason is that people’s working conditions are harsh and stressful in these border regions. Therefore, these individuals tend to relax and unwind at the end of the day with alcohol and sexual activity.35 In addition, it may be due to socioeconomic and sociocultural differences among regions.
On the multivariable mixed-effect analysis, age, marital status, sex of household head, Internet, khat, and alcohol use, and region were associated with MSPs among men in Ethiopia. We found that older men had higher odds of having MSPs. This is in line with previous studies,14,16,25 but contrary to studies conducted in Lesotho and South Africa.5 This may be due to the greater desire for and familiarity of older men with sex-related activities.
Respondents who had never married had higher odds of having MSPs than those who were married. This is supported by a study conducted in the US.28 A possible explanation might be that never-married men are vulnerable to experiencing MSPs in the course of seeking an ideal partner. Married men, who are likely to have a safe and settled state of living, avoid risky sexual behaviors like MSPs.36 Sex of the household head was also an important factor associated with MSPs. The odds of having MSPs were higher for female-headed households, contrary to a study conducted in Lesotho,14 which revealed that coming from a female-headed household decreased the odds of having MSPs. This may be because the woman participates in MSPs for reasons of economic survival, and this in turn leads to men getting MSPs.
Use of the Internet was a significant factor, ie, respondents who were Internet users were more likely to have MSPs. This finding is in line with studies done in sub-Saharan Africa,29 Nigeria,21 and Virginia.23 In addition, a relationship of online dating via Internet with risky sexual behavior has been reported in studies conducted in Hong Kong and the Netherlands.37,38 This may be because the widespread accessibility of the Internet can easily promote communication of sensitive issues and sex-related information that allow a person to pursue sexual pleasure. Furthermore, adult men who frequently use the Iinternet are mostly sexually active and may be exposed to pornography, found frequently and increasingly online, and tend to engage in MSPs.39–41
Chewing khat was associated with higher odds of having MSPs, and this is supported by studies conducted in sub-Saharan Africa15 and Ethiopia.26,27,42 Moreover, drinking alcohol was another important factor associated with increased odds of having MSPs. This finding is also supported by different studies.15,22,24,27,43–46 This association of alcohol and khat consumption with having MSPs might be due to impaired ability in realizing risks (eg, probability of getting infected with HIV/AIDS and other STIs), in turn increasing risky sexual behaviors, such as having of MSPs.47
This study had both strengths and limitations. Since it was cross-sectional study it cannot show a cause-and-effect relationship between having MSPs and exposure variables. In addition, since our outcome variable (MSPs) was assessed based just on the responses of males to the question “How many sex partners including spouse in the last 12 months?”, there may have been a social desirability bias. However, this research has value, as it used spatial analysis and identified the most vulnerable areas using SaTScan analysis, as well as using representative national data to inform policy-makers and other governmental and nongovernmental organizations to take concrete action on this public-health problem.
Conclusion
This study revealed that there was a spatial clustering/variation in MSPs among reproductive men in Ethiopia. The primary clusters sptial window were located in Oromia and Somalia regions. Older age, never married, female-headed household, Internet use, khat alcohol consumption, and being from regions other than Tigray, Harari, and Dire Dawa increased the odds of having MSPs. However, being from the Amhara region decreased the odds of having MSPs. Therefore, special attention to high-risk regions and groups identified in this study could decrease MSPs in men and serious consequences, such as HIV and STIs.
Abbreviations
AIC, Akaike information criterion; EDHS, Ethiopian Demographic and Health Survey; ICC, intraclass correlation; LLR, log-likelihood ratio; RR, relative risk.
Data Sharing Statement
We included all result-based data in the manuscript, and the data set can be accessed from www.measuredhs.com/data.
Ethics Approval and Consent to Participate
We accessed the data set from the DHS website (https://dhsprogram.com) through registering or online requests. Ethics approval was not required, since we used publicly available data. This research was exempted by the Institute of Public Health College of Medicine and Health Sciences University of Gondar Institutional Review Committee.
Acknowledgments
Our sincere gratitude and appreciation go to the DHS Program for permission to use the EDHS data set for conducting this study.
Author Contributions
All authors made a significant contribution to the work reported, whether in conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval to the version to be published, agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Chawla N, Sarkar S. Defining “High-risk Sexual Behavior” in the context of substance use. J Psychosexual Health. 2019;1(1):26–31. doi:10.1177/2631831818822015
2. Glen-Spyron C. Risky Sexual Behavior in Adolescence. Namibia: Belia Vida Centre; 2015.
3. Dimbuene ZT, Emina JB, Sankoh O. UNAIDS ‘multiple sexual partners’ core indicator: promoting sexual networks to reduce potential biases. Glob Health Action. 2014;7:23103. doi:10.3402/gha.v7.23103
4. Thornton R. Sexual networks and social capital: multiple and concurrent sexual partnerships as a rational response to unstable social networks. Afr J AIDS Res. 2009;8(4):413–421.
5. Onoya D, Zuma K, Zungu N, Shisana O, Mehlomakhulu V. Determinants of multiple sexual partnerships in South Africa. J Public Health (Bangkok). 2015;37(1):97–106.
6. Mutinta G. Multiple sexual partnerships and their underlying risk influences at the University of KwaZulu-Natal. J Human Ecol. 2014;46(2):147–155.
7. Mutinta G. Multiple sexual partnerships and their underlying risk influences at the University of KwaZulu-Natal. J Human Ecol. 2018;46(2):147–155.
8. Onoya D, Zuma K, Zungu N, Shisana O, Mehlomakhulu V. Determinants of multiple sexual partnerships in South Africa. J Public Health (Oxf). 2015;37(1):97–106.
9. Apari P, de Sousa JD, Muller V, Rall GF. Why sexually transmitted infections tend to cause infertility: an evolutionary hypothesis. PLoS Pathog. 2014;10(8):e1004111. doi:10.1371/journal.ppat.1004111
10. Tanser F, Bärnighausen T, Hund L, Garnett GP, McGrath N, Newell M-L. Effect of concurrent sexual partnerships on rate of new HIV infections in a high-prevalence, rural South African population: a cohort study. Lancet. 2011;378(9787):247–255. doi:10.1016/S0140-6736(11)60779-4
11. Rector RE, Johnson KA, Noyes LR, Martin S. The Harmful Effects of Early Sexual Activity and Multiple Sexual Partners Among Women. The Heritage Foundation; 2003.
12. Berde AS, Ozcebe H. Risk factors for prelacteal feeding in sub-Saharan Africa: a multilevel analysis of population data from twenty-two countries. Public Health Nutr. 2017;20(11):1953–1962. doi:10.1017/S1368980017000659
13. Bingenheimer JB. Men’s multiple sexual partnerships in 15 Sub-Saharan African countries: sociodemographic patterns and implications. Stud Fam Plann. 2010;41(1):1–17. doi:10.1111/j.1728-4465.2010.00220.x
14. Karabo EM. Covariates of multiple sexual partnerships among sexually active men in Lesotho. Afr J Reprod Health. 2017;21(1):73–81. doi:10.29063/ajrh2017/v21i1.6
15. Shayo FK, Kalomo MH. Prevalence and correlates of sexual intercourse among sexually active in-school adolescents: an analysis of five sub-Sahara African countries for the adolescent’s sexual health policy implications. BMC Public Health. 2019;19(1):1285.
16. Gurmu E. Differentials and determinants of men’s sexual behavior in Ethiopia. Ethiop J Health Dev. 2017;31(1):36–43.
17. Central Statistical Agency. Demographic and Health Survey 2016. Rockville, Maryland, USA: The DHS Program ICF; 2016.
18. Abosetugn AE, Zergaw A, Tadesse H. Correlations between risky sexual behavior and parental communication among youth in Dilla Town, Gedeo Zone, South Ethiopia. Biol Med. 2015;07(05). doi:10.4172/0974-8369.1000253
19. Waktole ZD, Dalby AR. Sexual behaviors and associated factors among youths in Nekemte town, East Wollega, Oromia, Ethiopia: a cross-sectional study. PLoS One. 2019;14(7):e0220235. doi:10.1371/journal.pone.0220235
20. Wordofa D, Shiferaw S. Sexual risk behaviors and its associated factors among undergraduate students in Madda Walabu University, Southeast Ethiopia: a facilitybased cross sectional study. Epidemiol. 2015;5(4).
21. Adebayo D, Udegbe IB, Sunmola A. Gender, internet use, and sexual behavior orientation among young Nigerians. Cyberpsychol Behav. 2006;9(6):742–752. doi:10.1089/cpb.2006.9.742
22. Alamrew Z. Prevalence and correlates of multiple sexual partnerships among private college students in Bahir Dar City, Northwest Ethiopia. Sci J Public Health. 2013;1:9. doi:10.11648/j.sjph.20130101.12
23. Brown MJ, Pugsley R, Cohen SA. Meeting sex partners through the internet, risky sexual behavior, and HIV testing among sexually transmitted infections clinic patients. Arch Sex Behav. 2015;44(2):509–519. doi:10.1007/s10508-014-0463-3
24. Given M. An exploratory study of the relationship between alcohol use and sexual risk behaviour among students at the University of Kwazulu-Natal. J AIDS Clin Res. 2015;6(1):1.
25. Hope R. Addressing Cross-Generational Sex: A Desk Review of Research and Programs. Washington, DC: Population Reference Bureau; 2007.
26. Muche AA, Kassa GM, Berhe AK, Fekadu GA. Prevalence and determinants of risky sexual practice in Ethiopia: systematic review and meta-analysis. Reprod Health. 2017;14(1):113. doi:10.1186/s12978-017-0376-4
27. Mulu W, Yimer M, Abera B. Sexual behaviours and associated factors among students at Bahir Dar University: a cross sectional study. Reprod Health. 2014;11(1):84. doi:10.1186/1742-4755-11-84
28. Santelli JS, Brener ND, Lowry R, Bhatt A, Zabin LS. Multiple sexual partners among US adolescents and young adults. Fam Plann Perspect. 1998;30:271–275. doi:10.2307/2991502
29. Uchudi J, Magadi M, Mostazir M. A multilevel analysis of the determinants of high-risk sexual behaviour in sub-Saharan Africa. J Biosoc Sci. 2012;44(3):289–311. doi:10.1017/S0021932011000654
30. Pawlowski B, Atwa R, Dunbar RIM. Sex differences in everyday risk-taking behavior in humans. Evol Psychol. 2008;6(1):29–42. doi:10.1177/147470490800600104
31. Central Statistical Agency (CSA) [Ethiopia] and ICF. Demographic and Health Survey 2016. Central Statistical Agency Addis Ababa, Ethiopia. Rockville, Maryland, USA: The DHS Program ICF; 2016.
32. Anselin L, Getis A. Spatial statistical analysis and geographic information systems. Ann Reg Sci. 1992;26(1):19–33. doi:10.1007/BF01581478
33. Kulldorff M. A spatial scan statistic. Commun Stat. 1997;26(6):1481–1496. doi:10.1080/03610929708831995
34. Wellings K, Collumbien M, Slaymaker E, et al. Sexual behaviour in context: a global perspective. Lancet. 2006;368(9548):1706–1728. doi:10.1016/S0140-6736(06)69479-8
35. Grovogel A. Finding different ways to unwind at the end of your day; 2020. Available from: https://greenbay.momcollective.com/health-wellness/finding-different-ways-to-unwind-at-the-end-of-your-day/.
36. Osuafor GN, Ayiga N. Risky sexual behaviour among married and cohabiting women and its implication for sexually transmitted infections in Mahikeng, South Africa. Sex Cult. 2016;20(4):805–823. doi:10.1007/s12119-016-9360-3
37. Choi EP, Wong JY, Lo HH, Wong W, Chio JH, Fong DY. The impacts of using smartphone dating applications on sexual risk behaviours in college students in Hong Kong. PLoS One. 2016;11(11):e0165394. doi:10.1371/journal.pone.0165394
38. Heijman T, Stolte I, Geskus R, et al. Does online dating lead to higher sexual risk behaviour? A cross-sectional study among MSM in Amsterdam, the Netherlands. BMC Infect Dis. 2016;16(1):288. doi:10.1186/s12879-016-1637-5
39. Flood M. Exposure to pornography among youth in Australia. J Sociol. 2007;43:45–60. doi:10.1177/1440783307073934
40. Akers RL. Criminological Theories: Introduction and Evaluation. Routledge; 2013.
41. Cooper A, Scherer CR, Boies SC, Gordon BL. Sexuality on the internet: from sexual exploration to pathological expression. Prof Psychol Res Pr. 1999;30(2):154. doi:10.1037/0735-7028.30.2.154
42. Temesgen G, Markos Y. Assessment of substance use and risky sexual behaviour among public college students in Bonga town, Southwest Ethiopia. Am J Biomed Life Sci. 2015;3(5):91–97. doi:10.11648/j.ajbls.20150305.11
43. Cook RL, Comer DM, Wiesenfeld HC, et al. Alcohol and drug use and related disorders: an underrecognized health issue among adolescents and young adults attending sexually transmitted disease clinics. Sex Transm Dis. 2006;33(9):565–570. doi:10.1097/01.olq.0000206422.40319.54
44. Bazargan-Hejazi S, Gaines T, Bazargan M, Seddighzadeh B, Ahmadi A. Alcohol misuse and multiple sexual partners. West J Emerg Med. 2012;13(2):151. doi:10.5811/westjem.2011.6.6676
45. Mola R, Araújo RC, Oliveira JVB, et al. Association between the number of sexual partners and alcohol consumption among schoolchildren. Jornal De Pediatria (Versão Em Português). 2017;93(2):192–199. doi:10.1016/j.jpedp.2016.07.010
46. Mutalip MHA, Mahmud MAF, Awaluddin M, et al. Risky sexual behaviours among school-going adolescent in Malaysia-findings from national health and morbidity survey. J Environ Sci. 2019;3(2):226–235.
47. Organización Mundial de la Salud. Department of Mental Health, Substance Abuse, World Health Organization. Mental Health Evidence, Research Team, World Health Organization, World Health Organization. Department of Mental Health, Substance Abuse. Alcohol Use and Sexual Risk Behaviour: A Cross-Cultural Study in Eight Countries. World Health Organization; 2005.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
