Back to Journals » Clinical Interventions in Aging » Volume 13
Sleep onset latency is related with reduced bone mineral density in elderly people with insomnia: a retrospective study
Authors Tong Q , Wu WZ, Wu Q , Yu YB, Lv XL, Wang BZ, Wang GF
Received 8 January 2018
Accepted for publication 25 June 2018
Published 30 August 2018 Volume 2018:13 Pages 1525—1530
DOI https://doi.org/10.2147/CIA.S161922
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Qian Tong,1,2,* Wanzhen Wu,2,* Qing Wu,2 Yanbo Yu,3 Xiaoling Lv,2 Bozhong Wang,2 Guofu Wang1,2
1Zhejiang Chinese Medical University, Hangzhou 310053, Zhejiang, China; 2Department of Geriatrics, Zhejiang Hospital, Zhejiang Provincial Key Lab of Geriatrics, Hangzhou 310013, Zhejiang, China; 3Wenzhou Medical University, Wenzhou, 325035 Zhejiang, China
*These authors contributed equally to this work
Purpose: Inconsistent outcome about association between insufficient sleep and bone mineral density (BMD) has been reported. The present study aimed to determine whether BMD was associated with score of Pittsburgh Sleep Quality Index (PSQI).
Methods: A total of 410 patients (mean age 81.6±5.9 years) attending our hospital for evaluation of sleep were retrospectively studied. Dual-Energy X-ray Absorptiometry was used to measure BMD and T-score at femoral neck and lumbar spines over L2–L4 regions. Subjective sleep status was evaluated by the PSQI questionnaires. The Mann–Whitney U test and chi-square analysis were used to compare continuous variables and categorical variables, respectively. Spearman correlation test was conducted to find the relationship between BMD and other clinical factors. Multinomial logistic regressions analysis was performed to analyze independent factors predicting BMD.
Results: Majority of the participants with osteoporosis (OP) were female and had lower body mass index (BMI) and higher sleep onset latency score. Spearman correlation test showed that gender, BMI, score of total PSQI, and sleep onset latency were significantly related to BMD and T-score in femoral neck and lumbar region L2–L4. Finally, multinomial logistic regression analysis demonstrated that gender and age were independent factors for OP and osteopenia and that after adjustment for gender, age, and BMI, sleep onset latency of <15 minutes (OR: 0.38; 95% CI: 0.15–0.96; P=0.04) and 16–30 minutes (OR: 0.37; 95% CI: 0.17–0.79; P=0.01) were less likely to have reduced BMD.
Conclusion: There was a significant association between BMD and sleep onset latency, suggesting that, in elderly patients with sleep problem, BMD measurement and intervention for OP might be valuable.
Keywords: bone mineral density, insomnia, osteoporosis, osteopenia, Pittsburgh Sleep Quality Index, sleep onset latency
Introduction
China is rapidly stepping into the aging society. The elderly population is usually affected by multiple chronic conditions, for example, osteoporosis (OP) and insomnia. Epidemiological data reported that insomnia and abnormal sleep disproportionally influence older population, with 47.2%–49.9% in China and 30%–40% around the world.1–3 Similarly, the population with OP will increase sharply from 83.9 million in 1997 to 212 million by 2050.4 Moreover, it is estimated that, in the developed countries, about 30% of all postmenopausal women have OP and that more than 40% of them have one or more fragility fractures during their remaining lifetime.5
Growing evidence suggested that insufficient sleep could be prone to obesity, diabetes, and cardiovascular diseases.6–9 More interestingly, a research study demonstrated that sleep deprivation could increase cortisol concentration, which might decrease bone formation and bone mineral density (BMD).10 In addition, a large number of studies have demonstrated that short sleep or long sleep resulted in elevated pro-inflammatory cytokines, including C-reactive protein, and interleukin-6, which subsequently increased osteoclast activity and consequent bone loss.11–14 Thus, it is reasonable to speculate that insomnia is related to OP.
However, clinical investigations concerning the association between sleep disorder and OP generated mixed results. For example, in PROOF Cohort research of 500 participants aged 65.7±0.8 years, participants with OP at the femoral level had a greater self-reported sleep duration (P=0.03) and were more frequently long sleepers (P=0.004) without differences for sleep quality (P=0.34) and sleep efficiency (P=0.80).15 Similarly, Tian et al reported that self-reported habitual sleep duration of 9 hours or longer was associated with an increased prevalence of OP.16 However, the NHANES study of 5,288 adults aged ≥50 years found that a sleep duration of <6 hours per night was associated with a significantly increased risk of OP, but only in the older age group (>65 years).17 In line with NHANES study, Rodrigues and Barros demonstrated that a higher prevalence of OP was seen in older people who slept <7 hours/day or in patients with insomnia.18 Therefore, based on the above results, it is necessary to further determine the relationship between sleep status and BMD in elderly patients.
In the present study, we reported a retrospective analysis to determine whether lumbar spines and femoral neck (FN) BMD and T score were associated with Pittsburgh Sleep Quality Index (PSQI) score in elderly Chinese people with insomnia.
Methods
Inclusion and exclusion criteria
It was a retrospective study and approved by the Medical Ethics Committee of Zhejiang Hospital (2017–23 k). All patients attending our hospital from October 2012 to September 2016 for the evaluation of sleep were analyzed. The inclusion criteria were age ≥60 years, complete PSQI questionnaires, and take Dual-Energy X-ray Absorptiometry (DEXA) measurement. The exclusion criteria in the present study mainly included age <60 years, metallic prosthesis/fixation at hip or lumbar spines, renal insufficiency, malignancy, connective tissue or musculoskeletal diseases, significant liver, thyroid, parathyroid gland, adrenal gland or pituitary diseases, inability to ambulate, taking bone active drugs (eg, bisphosphonates, parathyroid hormones, denosumab), hormone replacement therapy, or glucocorticoids.
Ethics approval
This was a retrospective study which used patients’ medical records from October 2012 to September 2016 rather than directly contacting patients. The risk of this research was no more than the minimum risk. More importantly, the researchers have promised to protect the privacy of participants. Hence, according to the 39th provisions of Chinese law, The Ethical Review of Human Biomedical Research (2016), the Medical Ethics Committee of Zhejiang Hospital agreed to exempt the patients consent.
Sleep assessment
Subjective sleep status was evaluated by the PSQI questionnaires, which include seven components, namely subjective sleep quality, sleep onset latency in minutes, sleep duration in hours, percentage sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction, weighted equally on an ordinal scale of 0–3.19 This scale is applicable to evaluate the sleep quality of patients with sleep disorder and mental disorder and also to evaluate the sleep quality of ordinary people. The cutoff values for sleep duration were <5 hours, 5–6 hours, 6–7 hours, and >7 hours, respectively.
BMD measurements
DEXA (GE Lunar-iDXA, GE Medical Systems, Madison, WI, USA), which was performed by a single experienced operator according to standard protocols, was used to measure BMD at FN and lumbar spines over L2–L4 regions. The short-term coefficient of variation for our DXA machine was no more than 2%. Diagnosis of OP was defined as the WHO criteria of a T-score ≤−2.5 at any one site, osteopenia (OS), T-score >−2.5 to <−1, and normal BMD, T-score ≥−1 (referent).20 BMD data within 3 months were accepted.
Statistical analysis
We used the SPSS 19.0 software (IBM Corporation, Armonk, NY, USA) package to complete statistical analyses. Nonparametric tests (the Mann–Whitney U test/Kruskal–Wallis test) and chi-square analyses were adopted to compare continuous variables and categorical variables, respectively. Spearman correlation test was used to determine the correlation between BMD and other clinical parameters. Multinomial logistic regressions analysis was conducted to determine the independent factors predicting OP and OS. The normal group was used as the control group. The final models were adjusted for demographic and clinical data (gender, body mass index [BMI]). P<0.05 was considered statistically significant.
Results
Characteristics of the participants
A total of 606 patients aged over 60 years attended our hospital for evaluation of sleep from October 2012 to September 2016. Among them, 410 patients (67.66%), receiving BMD measurement, were included in the retrospective analysis. The remaining 196 population (32.34%) were excluded due to lack of BMD data within 3 months.
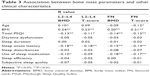
The participants were mostly men (57.1%), with a mean age of 81.6±5.9 years, a mean BMI of 23.7±3.7 kg/m2, and a mean PSQI score of 7.2±3.7. As showed in Table 1, when compared to male participants, female participants had poorer BMD and T-score at lumbar spines over L2–L4 regions and FN, and higher score of total PSQI score, sleep duration, sleep onset latency, use of sleep medication, sleep efficiency, subjective sleep quality, although they were younger.
  | Table 1 Baseline characteristics of study population |
Clinical and PSQI data of participants with different bone mass status
First, chi-square test and Kruskal–Wallis test were used to find differences in clinical and PSQI parameters among different bone mass status. As reported in Table 2, majority of participants with OP were female and had significantly lower BMI and higher sleep onset latency score, without difference for age, total PSQI score, and score of subjective sleep quality, sleep duration, percentage sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction.
BMD, clinical factors, and PSQI score (single-factor analysis)
We used Spearman correlation test to investigate whether clinical characteristics and PSQI score were related to bone mineral status. Table 3 shows that gender, BMI, score of total PSQI, and sleep onset latency were significant related with BMD and T-score in FN and lumbar region L2–L4. In addition, other factors affecting bone mass status included score of use of sleep medication (L2–L4 BMD: r=−0.10, P<0.05; FN BMD: r=−0.18, P<0.01; FN T-score: r=−0.17, P<0.01) and age (L2–L4 BMD: r=0.10, P<0.05; FN T-score: r=−0.12, P<0.05). No correlations were noted between bone mass status and other clinical and PSQI data.
Clinical and sleep determinants of bone mineral status in elderly patients with sleep problem (multivariable analyses)
Finally, to further identify independent factors predicting bone mineral status in elderly patients with sleep problem, multinomial logistic regressions analysis was performed.
In our model, gender and age were independent factors for OP and OS. After adjustment for gender, age, and BMI, elderly patients with sleep onset latency of <15 minutes (OR: 0.38; 95% CI: 0.15–0.96; P=0.04) or 16–30 minutes (OR: 0.37; 95% CI: 0.17–0.79; P=0.01) were less likely to have OS (Table 4).
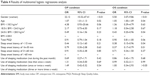  | Table 4 Results of multinomial logistic regressions analysis |
Discussion
The aim of this study was to analyze whether PSQI score was related to bone mineral status in elderly patients with sleep problem. First, single-factor analysis showed that in elderly patients with sleep disorder, gender, BMI, score of total PSQI, and sleep onset latency were significantly related to BMD and T-score in FN and lumbar region L2–L4. More interestingly, we found that gender and age were independent factors for OP and OS and that sleep onset latency was less likely to have decreased bone mass. Last, sleep duration was not related to BMD in our study. So far, previous research concerning the relationship between sleep duration and BMD obtained conflicting results, with some reporting the independent risk of short sleep for OP15,16,19–22 and others showing an independent risk in long sleepers.17,18,23–26 Our present work, to our knowledge, was the first to find that long sleep onset latency was an independent risk for reduced BMD.
The possible factors resulting in discrepancies among those studies included the large range of age (eg, from 18 to 80 years),23 different nationalities, limited evaluation of sleep duration using just a single question,20,21,23 different criteria to define OP without DEXA measurement,16,25,26 diverse cutoff value of sleep duration,19,22 and so on. In the present study, we performed DEXA, which is a gold standard for OP diagnosis, to measure BMD at different sites.
Questionnaires, including PSQI for sleep quality and the Epworth Sleepiness Scale (ESS) for daytime sleepiness, were often applied to assess sleep disturbance and its consequences.27,28 PSQI has been proven to have an excellent sensitivity and reliability in both middle-aged participants and the elderly.19,30 Study showed that a global PSQI score >5 gained a diagnostic sensitivity of 89.6% and specificity of 86.5% (kappa =0.75, P<0.001) in distinguishing good and poor sleepers.19 More importantly, Spira et al reported that internal consistency was adequate for PSQI (Cronbach’s α=0.69) and ESS (α=0.70) total scores in older men and that PSQI could distinguish participants reporting no sleep disorder from those reporting particular disorders more reliably than the ESS.28 In the present study, the cutoff values chosen for sleep duration were <5, 5–6, 6–7, and >7 hours, according to PSQI scoring method. However, previous studies adopted different cutoff values, which might be one of the reasons causing inconsistent results. For example, sleep duration cutoff values were chosen as 6, 7, and 8 hours in study by Kobayashi et al19 and 5, 6, 7, and 8 hours in research by Kim et al20.
The possible mechanisms by which long sleep onset latency could contribute to reduce BMD are unclear and need to be further studied in the future, because no related study has been reported so far. However, taking into account that insomnia makes it easy for patients to decrease BMD and that osteoporotic fracture causes high mortality rate and bad outcome,29,30 we can conclude that early screening and intervention for OP in elderly patients with insomnia might ameliorate their quality of life.
The strengths of our work included the measurement of BMD by DEXA at multiple bone sites (L2–L4 and FN) which is a gold standard for OP diagnosis, a relatively larger sample size, use of a validated PSQI sleep questionnaire, and so on. However, there are some limitations in the present study. First, it is a retrospective, observational association study, which tended to leave uncertainty. Second, it lacked clinical outcome, such as fracture, comorbidities, use of antiosteoportic drugs, and so on, which is the limitation of the retrospective study. Furthermore, the participants were heterogeneous, with diversities of medication and different morbidity, which might confound the results. Finally, the results of our study were based on Chinese elderly populations. Hence, it is necessary to further explore in other ethnicities and population of other ages.
Conclusion
Our retrospective analysis found that sleep onset latency was related to reduced BMD in elderly people with insomnia, indicating that it is meaningful to screen and intervene for OP in elderly patients with sleep problem.
Acknowledgments
We would like to thank Yefei Fang (Yuyao People’s Hospital) for her helpful advice on data acquisition. This study was funded by the National Natural Science Foundation of China (31670701).
Disclosure
The authors report no conflicts of interest in this work.
References
Roepke SK, Ancoli-Israel S. Sleep disorders in the elderly. Indian J Med Res. 2010;131:302–310. | ||
Roberts RE, Shema SJ, Kaplan GA, Strawbridge WJ. Sleep complaints and depression in an aging cohort: a prospective perspective. Am J Psychiatry. 2000;157(1):81–88. | ||
Liu Y, Dong YH, Xy L, Mao XQ, Peng GP, Liu L. Meta-analysis of the prevalence of sleep disorder among Chinese elderly aged 60 years and over. Modern Prev Med. 2014;41:1442–1445. | ||
Lin X, Xiong D, Peng YQ, et al. Epidemiology and management of osteoporosis in the People’s Republic of China: current perspectives. Clin Interv Aging. 2015;10:1017–1033. | ||
Melton LJ, Chrischilles EA, Cooper C, Lane AW, Riggs BL. Perspective. How many women have osteoporosis? J Bone Miner Res. 1992;7(9):1005. | ||
Chaput JP, Després JP, Bouchard C, Astrup A, Tremblay A. Sleep duration as a risk factor for the development of type 2 diabetes or impaired glucose tolerance: analyses of the Quebec Family Study. Sleep Med. 2009;10(8):919–924. | ||
Chien KL, Chen PC, Hsu HC, et al. Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. Sleep. 2010;33(2):177–184. | ||
Spiegel K, Leproult R, van Cauter E, van CE. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435–1439. | ||
Miller MA, Cappuccio FP. Biomarkers of cardiovascular risk in sleep-deprived people. J Hum Hypertens. 2013;27(10):583–588. | ||
Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC. Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potential mechanisms of their deleterious effects on bone. J Clin Invest. 1998;102(2):274–282. | ||
Ferrie JE, Kivimäki M, Akbaraly TN, et al. Associations between change in sleep duration and inflammation: findings on C-reactive protein and interleukin 6 in the Whitehall II Study. Am J Epidemiol. 2013;178(6):956–961. | ||
Dowd JB, Goldman N, Weinstein M. Sleep duration, sleep quality, and biomarkers of inflammation in a Taiwanese population. Ann Epidemiol. 2011;21(11):799–806. | ||
Mclean RR. Proinflammatory cytokines and osteoporosis. Curr Osteoporos Rep. 2009;7(4):134–139. | ||
Braun T, Schett G. Pathways for bone loss in inflammatory disease. Curr Osteoporos Rep. 2012;10(2):101–108. | ||
Saint Martin M, Labeix P, Garet M, et al. Does subjective sleep affect bone mineral density in older people with minimal health disorders? The PROOF cohort. J Clin Sleep Med. 2016;12(11):1461–1469. | ||
Tian Y, Shen L, Wu J, et al. Sleep duration and timing in relation to osteoporosis in an elderly Chinese population: a cross-sectional analysis in the Dongfeng-Tongji cohort study. Osteoporos Int. 2015;26(11):2641–2648. | ||
Cunningham TD, di Pace BS. Is self-reported sleep duration associated with osteoporosis? Data from a 4-year aggregated analysis from the National Health and Nutrition Examination Survey. J Am Geriatr Soc. 2015;63(7):1401–1406. | ||
Rodrigues IG, Barros MB. Osteoporosis self-reported in the elderly: a population-based survey in the city of Campinas, São Paulo, Brazil. Rev Bras Epidemiol. 2016;19(2):294. | ||
Kobayashi D, Takahashi O, Deshpande GA, Shimbo T, Fukui T. Association between osteoporosis and sleep duration in healthy middle-aged and elderly adults: a large-scale, cross-sectional study in Japan. Sleep Breath. 2012;16(2):579–583. | ||
Kim N, Choi HR, Kim SW, Kim BS, Won CW, Kim SY. Association between bone mineral density and sleep duration in the Korean elderly population. Korean J Fam Med. 2014;35(2):90–97. | ||
Niu J, Sahni S, Liao S, Tucker KL, Dawson-Hughes B, Gao X. Association between sleep duration, insomnia symptoms and bone mineral density in older Boston Puerto Rican adults. PLoS One. 2015;10(7):e0132342. | ||
Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, van den Berg JF, Verschuren WM. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN study. Sleep. 2011;34(11):1487–1492. | ||
Fu X, Zhao X, Lu H, Jiang F, Ma X, Zhu S. Association between sleep duration and bone mineral density in Chinese women. Bone. 2011;49(5):1062–1066. | ||
Specker BL, Binkley T, Vukovich M, Beare T. Volumetric bone mineral density and bone size in sleep-deprived individuals. Osteoporos Int. 2007;18(1):93–99. | ||
Chen G, Chen L, Wen J, et al. Associations between sleep duration, daytime nap duration, and osteoporosis vary by sex, menopause, and sleep quality. J Clin Endocrinol Metab. 2014;99(8):2869–2877. | ||
Wang K, Wu Y, Yang Y, et al. The associations of bedtime, nocturnal, and daytime sleep duration with bone mineral density in pre- and post-menopausal women. Endocrine. 2015;49(2):538–548. | ||
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. | ||
Spira AP, Beaudreau SA, Stone KL, et al. Reliability and validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older men. J Gerontol A Biol Sci Med Sci. 2012;67(4):433–439. | ||
Sivertsen B, Lallukka T, Salo P, et al. Insomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in Norway. J Sleep Res. 2014;23(2):124–132. | ||
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–475. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.