Back to Journals » Clinical Ophthalmology » Volume 12
Simultaneous intratunnel cross-linking with intrastromal corneal ring segment implantation versus simultaneous epithelium-off cross-linking with intrastromal corneal ring segment implantation for keratoconus management
Authors Hosny M , Nour M, Azzam S , Salem M, El-Mayah E
Received 10 September 2017
Accepted for publication 17 November 2017
Published 17 January 2018 Volume 2018:12 Pages 147—152
DOI https://doi.org/10.2147/OPTH.S151313
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mohamed Hosny, Moustafa Nour, Sarah Azzam, Mohsen Salem, Esraa El-Mayah
Department of Ophthalmology, Cairo University, Giza, Egypt
Purpose: The purpose of this study is to compare the efficacy of intratunnel cross-linking combined with intrastromal corneal ring segment (ICRS) implantation versus combined epithelium-off (epi-off) cross-linking and ICRS implantation for the management of keratoconus.
Methods: Our study included 20 eyes of 12 patients with moderate-to-severe keratoconus. Group A included 10 eyes that underwent simultaneous ICRS implantation with intratunnel cross-linking. Group B included 10 eyes that underwent simultaneous ICRS implantation with epi-off cross-linking. Uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest sphere and cylinder, mean and maximum keratometric readings, corneal thickness at pachy apex and thinnest location, as well as corneal hysteresis (CH) and corneal resistance factor (CRF) were compared preoperatively and at 6 months postoperatively.
Results: The mean UDVA and CDVA improved significantly in both groups with a statistically nonsignificant difference between the groups (P=0.798 and 0.126, respectively). The manifest cylinder decreased significantly in both groups, while the manifest sphere decreased significantly in Group A but nonsignificantly in Group B with a statistically nonsignificant difference between the groups (P=0.773 and 0.111, respectively). Both techniques led to significant flattening of the cornea and a significant decrease of Km and Kmax with a statistically nonsignificant difference between the groups (P=0.312 and 0.857, respectively). There was a statistically significant decrease in CH in both groups postoperatively; however, there was a statistically nonsignificant increase in CRF after both techniques with a statistically nonsignificant difference between the groups in the mean change of CH and CRF (P=0.633 and 0.313, respectively). No intraoperative or postoperative complications were observed in both groups.
Conclusion: Both techniques improved the visual and refractive outcomes in cases of moderate and severe keratoconus with no statistically significant difference between the groups; however, simultaneous intratunnel cross-linking and ICRS implantation showed early visual rehabilitation due to the absence of epithelial defect.
Keywords: keratoconus, cross-linking, intratunnel, epi-off, ICRS
Introduction
Keratoconus is the most common primary corneal ectasia.1 It is a bilateral and asymmetric corneal degeneration characterized by localized corneal thinning which leads to protrusion of the thinned cornea.2–5 Intrastromal corneal ring segment (ICRS) can be used in the treatment of keratoconus as it acts by an arc-shortening effect, flattens the center of the cornea, and provides a biomechanical support for the thin ectatic cornea.6 It aims to defer the need for corneal transplantation and restore contact lens tolerance (by making their astigmatism more regular).6
The corneal collagen cross-linking (CXL) by the photosensitizer riboflavin and ultraviolet A (UVA) light is the main treatment that changes the intrinsic biomechanical properties of corneal collagen and was first introduced by Wollensak.7 It creates additional chemical bonds inside the corneal stroma by means of a photo-polymerization in the anterior stroma.7 The placement of riboflavin in the stroma can be done by different methods with or without epithelial removal, or using the tunnel created by a femtosecond laser for ICRS placement.8–10
ICRS implantation can be combined with CXL in progressive cases of keratoconus, and their effect is potentially synergistic. The ideal sequence and timing of the two procedures are still controversial.11–13 In our study, we compared the effect of simultaneous ICRS implantation and CXL versus combined ICRS implantation and CXL.
Patients and methods
This was a prospective, randomized, interventional comparative clinical cohort study that included 20 eyes of 12 patients with moderate-to-severe keratoconus. Diagnosis was based on slit-lamp examination and corneal topography. Keratoconus cases were classified according to the Amsler–Krumeich grading system.
Our study was approved by the ethical committee of ophthalmology department, Cairo University, and it followed the principles of the Declaration of Helsinki. In adherence with our institutional guidelines, all patients provided a written informed consent.
All eyes included in the study had keratoconus grades II–III with contact lens intolerance and corneal thickness at the thinnest point of at least 400 μm with clear cornea. We excluded pregnant or breast-feeding patients and those with the following diagnoses: grade IV keratoconus; hydrops; corneal opacity; severe atopy; collagen, vascular, autoimmune, or other ocular or systemic disease.
The patients were randomly divided into two groups (based on a selection card chosen by the patient). Group A underwent simultaneous ICRS implantation with intratunnel cross-linking. Group B underwent simultaneous ICRS implantation with epithelium-off (epi-off) cross-linking. In all cases, the following examinations were performed before surgery and at 6 months postoperatively: uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest refraction, slit-lamp biomicroscopy, indirect ophthalmoscopy, intraocular pressure (IOP) by tonometry, Scheimpflug imaging with a Pentacam device (Oculus Optikgeräte, GmbH), and corneal hysteresis (CH) by Ocular Response Analyzer (Reichert Ophthalmic Instruments, Depew, NY, USA).
Surgical technique
The procedure was done under topical anesthesia using benoxinate hydrochloride 0.4% eye drops (Benox; Eipico Inc., Cairo, Egypt). This was followed by application of topical moxifloxacin hydrochloride 0.5% (Vigamox; Alcon Surgical, Fort Worth, TX, USA) eye drops as a prophylaxis against infection.
Tunnel formation
The creation of the intrastromal pocket for Kera ring implantation was performed by means of the 200 kHz femtosecond technology FS200 (Alcon Surgical) in all cases. A vacuum ring was fixated to the eye after a tunnel is created under high IOP.
Kera ring implantation
According to specific nomogram, the Kera ring (Mediphacos, Belo Horizonte, Brazil) was selected, with 5 mm diameter (4.4 mm internal diameter and 5.6 mm external diameter), variable thickness (150–300 μm), and four arc segments (90°, 120°, 160°, and 210°). It was inserted into this corneal tunnel. In the intratunnel CXL group, injection of the isoosmolar riboflavin 0.1% solution in 20% dextran (VibeX; Avedro Inc., Waltham, MS, USA) in the pocket was done before insertion of the ring, and then the cornea was exposed to UVA radiation of 370 nm, at 18 mW/cm2 for 5 min. In the epi-off CXL group, the epithelium in the central 8–9 mm was removed by a blade, and then isoosmolar riboflavin 0.1% solution in 20% dextran (VibeX, Avedro Inc.) was applied for 5 min and exposed to UVA radiation of 370 nm, at 18 mW/cm2 for 5 min. Then, a soft bandage contact lens was applied that was removed on the first day in Group A and after epithelial continuity in Group B between 5 and 7 days.
Postoperatively, topical antibiotics and nonsteroidal anti-inflammatory drugs were prescribed. Topical steroids were initiated after complete healing of the epithelium in Group B and from the start in Group A.
Postoperative assessment
Postoperative visits were scheduled for the first postoperative day, the first week, first month, and 6 months after surgery. On the first postoperative day, slit-lamp examination was performed to ensure the Kera ring position, corneal haze, and integrity. The patients with epi-off cross-linking were followed up until complete epithelization. Six months after the surgery, full ophthalmological examination, corneal topography, and ORA were performed.
Statistical analysis
Statistical analyses were done using Microsoft Excel 2010 and SPSS software version 20.0 for Windows. Data were presented in terms of parametric and nonparametric data using Kolmogrov–Smirnov test. All data showed normal distribution, and paired t-test was used for statistical analysis to compare data before and after each treatment. Independent t-test was used to compare data of two groups. All values are given as mean ± SD. All tests were two-tailed and considered significant at P<0.05 and highly significant at P<0.01.
Results
Study population
A total of 20 eyes of 12 patients were classified into two groups. Group A underwent simultaneous ICRS implantation with intratunnel cross-linking and included 10 eyes of six patients (two males and four females) with a mean age of 24.4 (±4.85 years), while Group B underwent ICRS implantation with epi-off cross-linking and included 10 eyes of six patients (four males and two females) with a mean age of 23 (±5.5) years.
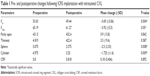
Group A
Table 1 shows the comparison between preoperative and postoperative results. As shown, there was a statistically significant improvement in the logMAR UDVA (mean change was 0.38) and logMAR CDVA (mean change was 0.1) (P<0.05). There was also a statistically significant decrease in the manifest sphere and cylinder (mean change was −2.5 D and −1.72 D, respectively) (P<0.05). We also found a decrease in the mean K and Kmax readings (mean change was 3.69 D and −3.92 D, respectively). There was no statistically significant increase in the corneal thickness at the pachy apex and the thinnest location. There was a statistically significant decrease in the CH (mean change was −0.44 mmhg) (P<0.05), but the change in the corneal resistance factor (CRF) was found to be statistically nonsignificant (0.18 mmhg, P=0.892). Figure 1A and B shows an example of Pentacam of one of the patients of this group.
  | Figure 1 Pentacam (A) before and (B) after treatment (patient in Group A). |
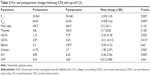
Group B
Table 2 shows a comparison of pre- and postoperative results in Group B. There was an improvement in the UDVA (0.26 logMAR) and best-corrected visual acuity (BCVA) (0.21 logMAR) (P<0.05). There was also a statistically significant decrease in the manifest cylinder (−1.85 D) (P<0.05), but the change in the manifest sphere was not significant (−0.45 D, P=0.66). There was a statistically significant decrease in the mean K and Kmax readings (−2.53 and −4.038 D). There was no statistically significant increase in the corneal thickness at the pachy apex and the thinnest location. There was a decrease in the CH by ORA at 6 months postoperatively (0.46 mmhg) (P<0.05) and an increase in CRF that was statistically nonsignificant (0.22 mmhg, P=0.401). Figure 2A and B shows the Pentacam of patients in Group B before and after treatment.
  | Figure 2 Pentacam (A) before and (B) after treatment (patient in Group B). |
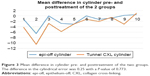
On comparing both groups, we found a statistically nonsignificant difference between them in all parameters tested (Figures 3 and 4). Table 3 shows the mean difference between the groups in all variables tested with corresponding level of significance. As shown, there was no statistically significant difference between the groups in all tested variables.
  | Figure 4 Mean difference in Km pre- and posttreatment of the two groups. The difference in Km was 1.39 with a P-value of 0.312. |
Discussion
The combination of ICRS implantation and CXL has a synergistic effect in improving the visual acuity and slowing the progression of keratoconus. The ideal sequence and timing of these procedures are still controversial.11–13 Some surgeons prefer rings inserted first so that the segments can reshape the cornea without restriction.12 Others perform CXL first to further flatten the cornea and to enhance corneal biomechanics and prevent progression.14
Our study described the combination of Kera ring implantation with CXL as a safe and effective treatment option in patients with keratoconus and contact lens intolerance.
In our study, the mean UDVA improved significantly at 6 months postoperatively. Compared with the studies published on Kera ICRS, mean UDVA in our patients increased with more Snellen lines after combined treatment than after implantation of Kera ring segments alone.15,16 Our results are in line with the study by Coskunseven et al that used combined ICRS implantation with CXL starting with either the CXL or the rings.16 However, in their study, the improvement was more in ICRS implantation group followed by CXL group after 7 months than the reverse sequence. Liu et al in their study showed that combined ICRS implantation and immediate CXL will improve the UDVA, BCVA, and spherical and cylindrical error but with no statistical difference in comparison to ICRS only or CXL followed by ICRS implantation.17
In comparison with Kilic et al’s study on 131 eyes with a mean follow-up of about 7 months, the mean improvement in logMAR UDVA was 0.26±0.16 (in our study, it was 0.38±0.25) and logMAR BCVA was 0.24±0.16 (in our study, it was 0.1±0.15), and the mean manifest cylinder improved from −3.89 (±1.97) to −2.27 (±2.18) D. In our study, the cylinder decreased from −4.975 (±1.64) to −3.25 (±1.3) D.10
El-Raggal in his prospective study divided the patients into two groups. Group 1 included nine eyes that underwent Kera rings insertion followed by CXL 6 months later, and Group 2 included seven eyes that underwent both the procedures simultaneously. The study showed that there was a statistically significant improvement in the final UDVA and BCVA, and decrease in spherical, cylindrical, and the mean keratometric reading from the preoperative values in the two groups. However, there was a statistically significant difference between the groups regarding the mean keratometric reduction with a greater reduction in Group 2 than in Group 1 (P=0.046).11
Alió et al in their study divided 27 patients into a classic group who were subjected to CXL with epithelial debridement with ICRS implantation (16 eyes) and a second group where patients were subjected to CXL with an intrastromal pocket with ICRS implantation (11 eyes).12 There was no significant difference between the patients of the two groups in terms of visual acuity, refraction, aberrometry, and pachymetry, which is in line with our results.
CH and CRF reflect the biomechanical properties of the eye, and they are lower in keratoconic eyes than normal.18 There was a decrease in the CH after treatment in both groups which is in line with the results of Pinero et al, although in their study only ICRS implantation was used as treatment.19 However, Barbara et al detected no significant difference after combined treatment with Intacs SK and CXL.20 Dauwe et al detected that there was no significant change in the viscoelastic properties after ICRS implantation.21 In our study, we found a statistically significant decrease in CH and a statistically nonsignificant increase in CRF.
Conclusion
The improvement in the UDVA, CDVA, manifest refraction, and keratometric values in our study may suggest that a simultaneous treatment might give better results than a sequential treatment, but larger sample sizes and longer follow-up are needed to validate these results. The nonsignificant difference between the groups widens the horizon of use of intratunnel CXL as a substitute of epi-off CXL when rapid visual recovery is needed or fear of epithelial defect is present. When we combined ICRS implantation with an intratunnel riboflavin injection, we obtained direct riboflavin penetration into the stroma without removing the epithelium. To our mind, this is the first randomized study to compare both techniques; however, a larger sample size and longer follow-up are recommended.
Disclosure
The authors report no conflicts of interest in this work.
References
Chopra I, Jain AK. Between eye asymmetry in keratoconus in an Indian population. Clin Exp Optom. 2005;88:146–152. | ||
Kymes SM, Walline JJ, Zadnik K, et al. Collaborative longitudinal evaluation of Keratoconus (CLEK) Study Group. Quality of life in keratoconus. Am J Ophthalmol. 2004;138:527-535. | ||
Zadnik K, Barr JT, Gordon MO, et al. Biomicroscopic signs and disease severity in keratoconus. Cornea. 1996;15:139–146. | ||
Zadnik K, Steger-May K, Fink BA, et al. Between-eye asymmetry in keratoconus. Cornea. 2002;21:671–679. | ||
Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol. 1986;101:267–273. | ||
Burris TE. Intrastromal corneal ring technology: results and indications. Curr Opin Ophthalmol. 1998;9:9–14. | ||
Wollensak G. Crosslinking treatment of progressive keratoconus: new hope. Curr Opin Ophthalmol. 2006;17:356–360. | ||
Baiocchi S, Mazzotta C, Cerretani D, et al. Corneal crosslinking: riboflavin concentration in corneal stroma exposed with and without epithelium. J Cataract Refract Surg. 2009;35:893–899. | ||
Wollensak G, Iomdina E. Biomechanical and histological changes after corneal crosslinking with and without epithelial debridement. J Cataract Refract Surg. 2009;35:540–546. | ||
Kilic A, Kamburoglu G, Akinci A. Riboflavin injection into the corneal channel for combined collagen crosslinking and intrastromal corneal ring segment implantation. J Cataract Refract Surg. 2012;38:878–883. | ||
El-Raggal TM. Sequential versus concurrent Kerarings insertion and corneal collagen cross-linking for keratoconus. Br J Ophthalmol. 2011;95(1):37–41. | ||
Alió JL, Toffaha BT, Piñero DP, et al. Cross-linking in progressive keratoconus using an epithelial debridement or intrastromal pocket technique after previous corneal ring segment implantation. J Refract Surg. 2011;27(10):737–743. | ||
Saib N, Bonnel S, Fenolland JR, et al. Intrastromal corneal rings and corneal collagen crosslinking for progressive keratoconus: comparison of two sequences. Eye (Lond). 2015;29(2):294–295. | ||
Henriquez MA, Lzquierdo L Jr, Bernilla C, et al. Corneal collagen cross-linking before Ferrara intrastromal corneal ring implantation on for treatment of progressive keratoconus. Cornea. 2012;31(7):740–745. | ||
Sansanayudh W, Bahar I, Nikhil L, et al. Intrastromal corneal ring segment SK implantation for moderate to severe keratoconus. J Cataract Refract Surg. 2010;36:110–113. | ||
Coskunseven E, Jankov MR, Hafezi F, et al. Effect of treatment sequence in combined intrastromal corneal rings and corneal collagen crosslinking for keratoconus. J Cataract Refract Surg. 2009;35(12):2084–2091. | ||
Liu XL, Li PH, Fournie P, et al. Investigation of the efficiency of intrastromal ring segments with cross-linking using different sequence and timing for keratoconus. Int J Ophthalmol. 2015;8(4):703–708. | ||
Spoerl E, Terai N, Scholz F, et al. Detection of biomechanical changes after corneal cross-linking using Ocular Response Analyzer software. J Refract Surg. 2011;27:452–457. | ||
Pinero DP, Alio JL, Barraquer RI, et al. Corneal biomechanical changes after intracorneal ring segment implantation in keratoconus. Cornea. 2012;31:491–499. | ||
Barbara R, Garzozi H, Barbara A. Combined Intacs SK and corneal collagen cross linking in the treatment of keratoconus. Int J Keratoconus Ectatic Dis. 2012;1(2):109–116. | ||
Dauwe C, Touboul D, Roberts CJ, et al. Biomechanical and morphological corneal response to placement of intrastromal corneal ring segments for keratoconus. J Cataract Refract Surg. 2009;35(10):1761–1767. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.