Back to Journals » Clinical Ophthalmology » Volume 17
Silicone Oil Utilized in Pars Plana Vitrectomy for Patients with Advanced Proliferative Diabetic Retinopathy: Physico-Chemical and Optical Properties
Authors Al-Dwairi R , Ahmad AA, Aleshawi A, Bani-Salameh AA, Aljarrah IA, Al-Bataineh QM, Al Beiruti S, Alshami AO, Rusen E, Toader G
Received 28 October 2023
Accepted for publication 26 November 2023
Published 6 December 2023 Volume 2023:17 Pages 3719—3728
DOI https://doi.org/10.2147/OPTH.S447099
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Rami Al-Dwairi,1 Ahmad A Ahmad,2 Abdelwahab Aleshawi,1 Areen A Bani-Salameh,2 Ihsan A Aljarrah,2 Qais M Al-Bataineh,2,3 Seren Al Beiruti,1 Ali Omar Alshami,1 Edina Rusen,4 Gabriela Toader5
1Department of Special Surgery, Division of Ophthalmology, Faculty of Medicine, Jordan University of Science & Technology, Irbid, 22110, Jordan; 2Department of Physics, Thin Films and Nanotechnology Laboratory, Faculty of Science and Art, Jordan University of Science & Technology, Irbid, 22110, Jordan; 3Leibniz Institut für Analytische Wissenschaften‐ISAS‐e.V., Dortmund, 44139, Germany; 4Faculty of Chemical Engineering and Biotechnologies, University POLITEHNICA of Bucharest, Bucharest, 011061, Romania; 5Military Technical Academy “Ferdinand I”, Bucharest, 050141, Romania
Correspondence: Rami Al-Dwairi, Department of Special Surgery, Division of Ophthalmology, Faculty of Medicine, Jordan University of Science & Technology, P. O. Box: 3030, Irbid, 22110, Jordan, Tel +962799273019, Fax +962 2 7201064, Email [email protected]
Objective: Silicone oils have the role in maintaining the attachment of the retina in conditions where the risk of retinal re-detachment is high. However, silicone oils have the tendency to emulsify with subsequent complications. In this work, analyses have been performed to understand changes that occurred to the optical, and physical characteristics of the oil after removal from the vitreous cavity of patients underwent pars plana vitrectomy (PPV) for fibrovascular membranes/tractional retinal detachment (FVM/TRD).
Methods: Four samples of silicone oil were allocated from patients who underwent PPV for FVM/TRD. The Fourier-transform infrared (FTIR) spectroscopy, micro-viscometry, and ultraviolet-visible spectrometer analyses were utilized to determine the changes in its chemical bondings, viscosity, absorbance, transmittance, buoyance, and specific gravity.
Results: The mean age of the patients was 49.0 years. The mean duration of silicone oil implantation was 18.9 months. FTIR analysis showed significant breaking in the chemical bonding that was related to the lens status during the primary PPV, the presence of significant retinal hemorrhages, the duration of silicone oil implantation, and the degree of silicone oil filling. Similarly, viscosity and contact angle analyses revealed a reduction in the viscosity with similar factors to the FTIR analysis. Moreover, absorbance and transmittance were largely affected by the aggressiveness of FVM/TRD.
Conclusion: This study revealed that certain factors such as the age of the patient, duration of silicone oil implantation, lens status, and the presence of retinal hemorrhages, the degree of silicone oil filling and aggressiveness of FVM/TRD may contribute to the emulsification process.
Keywords: silicone oil, tractional retinal detachment, emulsification, viscosity
Introduction
Standard ophthalmic silicon oils are synthetic polymers based on polydimethylsiloxane (PDMS) chains that have different lengths.1 Silicone is an inorganic polymer composed of an alternating silicon-oxygen backbone connected to two organic groups linked to each silicon atom. Silicone has many forms, such as oil, rubber, resin, and grease.2,3 Silicone oil has high chemical and thermal stability, high oxidation resistivity, high shear stress resistivity, moderate water-repellent, moderate corrosion stability, and low toxicity.4,5 The main variations between ophthalmologic silicone oils depend on the molecular weight (MW), linear chain length, chemical composition of radical side groups (eg, methyl, phenyl, vinyl, and trifluoropropyl groups), radical end termination of polymer chains, and chain size distribution.6 As a result, every type of silicone oil has unique chemical and physical properties. Silicone oils have the capacity to be either lighter or heavier than water, and this attribute results from the radical side groups, allowing them to provide a tamponade action on either the superior or inferior retina.6
In 1962, Cibis et al7 were the first ones to introduce silicone oil in ophthalmic surgery. After that, silicone oil was approved for use as an intraocular tamponade in 1996. Many ocular indications were shown to have benefits from silicone oil implantation such as complicated retinal detachment, tractional retinal detachment (TRD) secondary to severe proliferative diabetic retinopathy, traumatic insults, viral retinitis with following retinal detachment, posterior pole detachment due to a macular hole in highly myopic eyes, persistent macular hole, colobomatous retinal detachment, and hypotony due to ciliary shutdown.8
TRD is a major and possible permanent leading factor of vision loss in patients with advanced proliferative diabetic retinopathy (PDR).9–12 Fibrovascular membranes (FVM) proliferation is the principal cause of TRD.13–15 The most common cause is advanced PDR. Other causes include vascular occlusions, sickle cell retinopathy, retinopathy of prematurity, and familiar exudative vitreoretinopathy.16,17 The most important driving factor is vascular endothelial growth factor (VEGF)-mediated neovascularization secreted in response to retinal ischemia.16 FVM tends to develop at the junction of the ischemic and non-ischemic retina or near the optic nerve.18 In about 5–10% of cases of TRD, anatomical and visual prognoses are affected by the presence of proliferative vitreoretinopathy (PVR).9,11,19,20 Surgical management of diabetic TRD is challenging.
Lucke et al reported in their study a total of 106 patients with advanced PDR in which the PPV was accompanied by silicone oil injection, and the reattachment rate was 73%.21 In a study by Yeo et al the success rate of retinal reattachment with silicone oil was 70% for 23 eyes with advanced PDR, and the final vision was 5/200 or better in 22% of the eyes.22 Brourman et al studies the effect of silicone oil on 37 eyes with refractory severe neovascular glaucoma and/or recurrent TRD as a result of severe PDR. Reattachment was obtained in 70%, and regression of anterior segment neovascularisation occurred in 36%.23 A more recent prospective study by Azen et al concluded that 359 eyes with severe PDR for which PPV and silicone oil injection were performed achieved complete retinal reattachment in 57%, and posterior pole reattachment in 74%.24
On the other hand, silicone oil is not without complications. It should be removed when the tamponade effect is satisfied. The duration for which silicone oil can remain in the eyes ranges between two to thirteen months.25 Although it is often recommended to remove silicone within 3–6 months25 after surgery to minimize potential side effects, this time frame remains a topic of debate. In patients with implants, free silicone has been discovered in the surrounding tissues and local lymph nodes.26 Lately, it has been demonstrated that some silicones are not stable in vivo but undergo chemical changes to a variety of hydrolyzed species.26,27 Silicone oil has a crucial effect on both anterior and posterior segments. Mechanisms include optic nerve damage or/and thinning in the inner retinal layers because of horizontal bipolar cell damage.28,29 Another major problem for silicone oil is the tendency to emulsify. Emulsification represents the process of formation of tiny droplets at the interfaces between the bubbles and intraocular fluids. Emulsification can aggravate proliferative vitreoretinopathy (PVR), increase the risk of inflammation, and decrease the success of retinal reattachment. In addition, it may contribute to band keratopathy, secondary glaucoma, and visual disturbance, even after silicone oil removal.30 The tendency to emulsify is determined by several factors, including interfacial surface tension, viscosity, chemical structure, the content of low molecular weight (MW) siloxane compounds or other impurities, and absorption of several biological substances from intraocular fluids and tissues (known as emulsifiers).6 Blood, proteins, lipids, and ionized solutions (eg, biological fluids) are all elements that might diminish surface tension and so cause emulsification when silicone oil is injected into the vitreous cavity.6 It is thought that certain mechanical factors can also cause emulsification, such as shear force during aqueous and oil movement along with rapid eye movements.31 Therefore, reducing the surface and interfacial tension leads to increasing emulsification due to the presence of surfactant in the eye.32
In addition, the other two important physical properties that influence emulsification are viscosity and molecular weight, ie, less viscous silicone oils (less molecular weight) emulsify earlier than higher viscous oils.33,34 Moreover, the duration of implantation of silicone oil has the most significant correlation with the occurrence of emulsification; the longer the duration, the higher the rate of emulsification.35 Other factors include the use of perfluorocarbon liquid in a direct exchange with silicone oil, impurities in silicone oil, and higher mechanical forces from intraocular instruments.32
This study aims to present a detailed investigation of the physicochemical and optical properties of silicone oil extracted from the vitreous of patients who underwent PPV for TRD/FVM, which was compared to the fresh unused silicone oil. This is a continuation and extension of our previous work on silicone oil samples extracted from patients with RRD.30 This study presents a unique approach by evaluating the various physicochemical parameters of ex-situ silicon oils extracted from the vitreous cavity. The study focuses on the key parameters related to viscosity, hydrophilicity, and optical properties. A comprehensive analysis of these parameters provides a better understanding of the properties of ophthalmologic silicon oils.
Methods
Patients and Data
This study was approved by the Institutional Review Board (IRB) at Jordan University of Science and Technology (number: 20/142/2021). The study included 4 eyes of 4 patients who underwent silicone oil removal for whom the first operation (the pars plana vitrectomy (PPV)) was performed due to traction retinal detachment (TRD) from severe fibrovascular membrane (FVM) proliferation. The study was conducted at the Ophthalmology services of a tertiary center, King Abdullah University Hospital, and in the Department of Physics and Nanotechnology laboratory at Jordan University of Science and Technology. Written informed consent was obtained from all patients. The study was conducted following the Declaration of Helsinki and its later amendments. Demographic information and medical history were obtained. Additionally, operative details (the indication and details for the first operation “pars plana vitrectomy”, duration of silicone oil within the vitrectomized eye, and the accompanying procedures with silicone oil removal) were collected. Moreover, postoperative courses were obtained, including visual outcomes, the need for antiglaucoma medications, and the retina status after silicone oil removal.
The included patients were scheduled for silicone oil removal with the primary operation PPV performed due to severe TRD/FVM. The FVM was developed due to either advanced diabetic retinopathy or advanced central retinal venous occlusion. A control sample of the same unused pure silicone oil (Huile Silicone Purifie Csi, FCI, France) was also analyzed and compared with the extracted samples.
Perioperative Setting and Samples Collection
The first PPV and the silicone oil removal were performed by a single consultant vitreoretinal surgeon, with the same following surgical guidelines. As described in our previous experiment,30 a 23-gauge vitrectomy system (Combined Wide-Field Elite Pack, Bausch, and Lomb) was utilized with a biplanar single-step technique. Under local and sterile condition, three sclerotomies were created 4 mm from the limbus, and 23-gauge trocars were inserted. The infratemporal trocar was connected to an infusion tube, and the infusion pressure was set at 30 mmHg. Using a machine-driven vacuum, up to 2 mL of silicone oil was extracted with a vacuum pressure set at 60 mm Hg. The retina was carefully monitored. The extracted 2 mL of silicone oil was pure and was not mixed with water. After extraction from the vitreous cavity, the silicone was kept in a sterile plastic syringe and put immediately in a dark container, which was then transferred to the physics lab where it was preserved in a temperature-controlled room at normal room temperature with low humidity. In two patients, phacoemulsification and intraocular lens implantation were performed at the beginning.
For all patients, the same standard, three 23 G PPVs, was used during the primary PPV. After core vitrectomy, peripheral vitreous and tractions between the anterior and posterior vitreous were removed with or without triamcinolone acetonide. The procedures involved the removal of fibrovascular tissues through segmentation and delamination, as well as the removal of old or fresh blood. Hemostasis was obtained by raising the infusion bottle or endo diathermy. Supplementary photocoagulation was then performed for the treatment of neovascularization or to barricade retinal breaks. Air–fluid exchange was always carried out at the end of each surgery, and silicone oil was injected with proper filling. The decision to tamponade with silicone was based on intraoperative findings to prevent the re-detachment of the retina in the postoperative period.
Physics and Optical Characterization
New silicone oil samples (Huile Silicone Purifie Csi, FCI, France, Viscosity = 5000 cSt) and silicone oil samples restored from the vitreous cavities of four patients were analyzed using different spectroscopic and physical measurements. The chemical structure of the silicone oil samples was investigated using Fourier-transform infrared spectroscopy (ALPHA, FTIR spectrometer, Bruker, USA) in the wavenumber range of 400 to 4000 cm.−1 Fourier-transform infrared (FTIR) spectroscopy was utilized to identify the functional groups of silicone oil and their vibrational bonding modes of the intermolecular atomic bands. Pure KBr was used as a background. FTIR spectra were recorded in transmittance mode from 400 to 4000 cm−1 at a resolution of 2 cm−1. The kinematic viscosity was measured using a micro-viscometer (HVROC-S, RheoSense).
A KSV CAM 200 apparatus was used for static contact angle measurements performed on dried films. Different liquid droplets were used with a drop volume of 20 μL. The measurement of each contact angle was made within 10s after each drop to ensure that the droplet did not soak into the film. The apparent contact angle measurements were obtained for pure silicone oil, and patient samples droplet injected from an automated 3mm syringe dispenser for all samples under the same pressure. Stereomicroscopes SZO-8 (Optika, Ponteranica (BG), Italy) was used to take droplet images and videos connected to a Stereo zoom microscope cooperate with a digital camera. The resultant videos were processed using ImageJ free source software (V 1.8.0_172) and divided into proper images. The contact angles reported were the mean of 10 determinations.
Finally, silicone oil samples’ optical transmittance and absorbance spectra were measured using ultraviolet-Visible (UV–Vis) spectral scanning at wavelengths ranged from 200 to 800 nm with a resolution of 1 nm at room temperature using an “EMC-61PC-UV” spectrophotometer (Oxford Instrument, UK).
Statistical Analysis
The extracted data were presented as frequency (percentage) for nominal data and mean ± standard deviation of the mean (SD) for normally distributed continuous variables. Limited statistical tests were applied due to the small sample size.
Results and Discussion
Clinical, Demographic, and Operative Characteristics
Unused silicone oil (control sample) and four silicone oil samples from 4 patient eyes were studied. The mean age of the patients was 49.0 (±13.0 SD) years. Three patients were females. The general demographic characteristics are presented in Table 1.
 |
Table 1 General Demographics and Characteristics |
All patients underwent pars plana vitrectomy due to FVM/TRD complex. The FVM was developed in all patients due to advanced proliferative diabetic retinopathy (PDR) except in patient 4 (the FVM resulted from ischemic central retinal venous occlusion). The primary operation comprised pars plana vitrectomy (PPV), FVM removal, TRD repair, and silicone oil injection for all patients.
In the case of patients 3 and 4, the pars plana vitrectomy (PPV) was combined with phacoemulsification. In patient 3, internal limiting membrane dye was injected due to the presence of extensive PVR over the macula due to chronic detachment. The operation for this patient ended with a large retinectomy, and a hemorrhage was noted during silicone oil injection. In patient 2, intravitreal anti-vascular endothelial growth after the primary operation was injected (while the silicone was within the eye). Notably, the silicone oil filling in this patient (patient 2) was around 90% (underfilled). The mean time silicone oil remaining within the vitrectomized eyes was 18.9 months (±0.94 standard deviation). All patients did not undergo laser after silicone oil injection in the outpatient clinic. Table 2 summarizes the operative details for all patients.
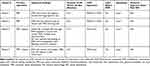 |
Table 2 Operative and Technical Details |
Clinical Outcome
Table 3 summarizes the clinical outcomes for all patients. All patients achieved flat retina 3 and 6 months after the removal. The visual outcome showed improvement in all patients except patient 3 where the preoperative status was advanced with chronic complex RD.
 |
Table 3 Clinical Outcomes |
FTIR Spectroscopy
The change in the chemical structure of silicone oils between the new silicon oil (control sample) and the samples extracted from four patients was investigated by analyzing the vibrational bands in FTIR spectra (Figure 1).
 |
Figure 1 (a) The chemical structure of the polydimethylsiloxane. (b) FTIR absorbance spectra for the control sample (pure silicon oil) and those for the four patients (Samples 1 to 4). |
The molecular structure of silicone oil (polydimethylsiloxane) contains a long chain of linked monomers, containing a silicon atom sharing two oxygen atoms at the main chain and CH3 molecules at other free axes (Figure 1a). The FTIR spectra for the control sample show many vibrational bands, ie, Si – O (686 cm−1), Si – (CH3)2 (805 cm−1), Si – O – Si (1050 cm−1), Si – CH3 (1268 cm−1), CHx (2977 cm−1), and C – H (3160 cm−1) (Figure 1b). Si – O – Si, Si – (CH3)2, and Si – CH3 bonds are the primary bonds in the silicone oil with higher intensities in the FTIR spectrum. Silicon and oxygen have a chance to connect with H when the primary bonds are broken. Decreasing the intensities of the Si – O, and Si – O – Si vibrational bands at samples extracted from patients’ eyes indicate the broken bonds and consequently the existence of emulsification, which may be due to the presence of retinal hemorrhages. This leads to decreasing silicon oil’s molecular weight and reducing viscosity, surface tension, and transparency.
Many factors may explain these findings; the combination of phacoemulsification with the primary PPV (in patients 3 and 4) may contribute to the emulsification of silicone oil by disrupting the natural crystalline lens diaphragm. In addition, the presence of significant hemorrhage and subretinal fluids in patient number three may play a role in the emulsification process. In patient 2, reducing silicone oil filling with the resultant fluid in the vitreous cavity may contribute to emulsification. Moreover, the long duration of silicone oil tamponade for all samples (especially 1 and 3) may contribute to the change in the properties of silicone oil.
Viscosity and Contact Angle Measurements
The kinematic viscosity of a fluid is the degree of inherently resisting flow under no external force other than gravity (weight). The kinetic viscosity of the samples decreased according to the patient’s medical conditions and treatment (Figure 2a). The kinetic viscosity of the control sample is 5000 cSt. The viscosity of samples 1 and 3 decreased to 4863 and 4881 cSt, respectively. Samples 1 and 3 have the highest viscosity of the patient samples, which can be attributed to the longer duration of silicone oil within the vitreous cavity and extensive hemorrhage after silicone oil injection. However, sample 2 has the least viscosity value (4675 cSt), which can be attributed to the underfilling of silicone oil. In addition, Sample 4 has a low viscosity value (4806 cSt), which can be attributed to the patient’s age. Water contact angle (WCA) measurements behave similarly to viscosity measurements (Figure 2b), following similar trends. It was observed that samples 1–4 possess a higher hydrophilicity, probably due to the pronounced emulsification process, which occurred more easily at lower viscosities.6
 |
Figure 2 (a) The kinematic viscosity and (b) water contact angle (WCA) of the silicone oil for the control sample (pure silicon oil) and those for the four patients (Samples 1 to 4). |
UV-Vis Spectroscopy
The transmittance spectra of the control sample (pure silicon oil) and the samples extracted from the patient’s eye are illustrated in Figure 3a. The transmittance spectrum of the control sample has values higher than 75% in the range of 350–700 nm (Visible region), indicating that the silicone oil is suitable for use in the patient’s eye. The transmittance spectrum for sample 1 has values higher than the control sample in the spectral range of 415–700 nm. However, in the range of 350–415 nm (violet region), the transmittance spectra decreased rapidly, indicating the limiting vision in this spectral range. In addition, the transmittance spectra for the other three samples decreased significantly in the visible region. This observation was consistent with the emulsification process that produces free radicals and broken bonds, producing dangling bonds that were free to interact with the incident light and absorb its energy. The patients’ medical conditions and the perioperative factors affect the pattern of each absorbance spectrum (Figure 3b). Destructing the bonds inside the silicone polymer decreases the viscosity of silicone oil, which reveals the formation of emulsified aggregates in the extracted samples. Accordingly, the borders and margins of these emulsified aggregates increase light absorption. The increase of absorption values in the region below the absorption edge (less than 300 nm) was due to the emulsification of silicone oil after use as tamponade, which is inconsistent with the transmittance analysis. Notably, the transmittance and absorbance of samples 3 and 2 are mostly affected, which may be explained by the presence of hemorrhage or fluid mixed with the silicone oil and the aggressiveness of FVM/TRD.
Figure 4 shows the well-known peaks of silicone oil for the control sample and samples 1 and 4 which fitted to two Gaussian crests.
 |
Figure 4 Gaussian fits (a-c) for different absorption peak observed for the silicon oil – Control Sample and the two patients observed in Figure 3 after manipulating them with baselines and normalization. Samples 2 and 3 showed no peak features that were not fitted. |
The main absorbance peak of the control silicone oil had two absorption sub-peaks (two frequency bands). High and low-frequency bands represent the Si-O-Si and Si-CH3 transition bands.30 The amplitude of the main peak and the high and low-frequency bands decreased in relevance to the patient’s age. This means the patient’s tamponade had high breaking bonds in the main chain structure. This was also an indication of different mechanisms of emulsification that occurred in this sample.
This study is not without limitations. First, the relatively small size of the extracted silicone oil minimizes our ability to perform more tests such as mass spectrometry. Second, the relatively small sample size is an important limiting point. Third, silicone oil is used as a tamponade for many indications other than TRD cases. Fourth, the large number of factors that may affect the physical properties make the results relatively heterogeneous.
Conclusions
This study is a pilot investigation of the optical and physical properties of silicone oil samples obtained from the vitrectomized eyes of patients who underwent PPV and silicone injection for FVM/TRD. A lower contact angle may imply higher hydrophilicity, which in turn, promotes emulsification processes. Moreover, transmittance, absorbance, and viscosity analyses were all conducted. Lower viscosities might indicate lower molecular weights caused by the modification of the chemical composition of the silicon oil, which predisposes to emulsification and its complications. Age-related changes of the vitreous, the presence of hemorrhages, underfilling of the silicone oil, lens status, the use of special dyes (as internal limiting membrane dye), the aggressiveness of the TRD/FVM, the duration of silicone oil tamponade, and many other factors may affect the rate of emulsification. All these results are hypotheses. Accordingly, we are working on further investigations, and practical research will be conducted on the pure silicone in an ex-situ condition to confirm this valuable conclusion.
Availability Data and Materials
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Institutional Board Review of Jordan University of Science and Technology (number: 20210430).
Consent for Publication
Written informed consent was obtained from all patients.
Acknowledgments
Our thanks are extended to Prof. Mohammad-Ali H. Al-Akhras for using his biomedical laboratory and Prof. Borhan Elbiss for using his superconductivity and nanotechnology laboratory.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors would like to acknowledge Jordan University of Science and Technology (JUST) in Jordan, the Deanship of Scientific Research, for their particular support with research grant No. 430/2021.
Disclosure
The authors declare no conflict of interest.
References
1. Chen Y, Kearns VR, Zhou L, et al. Silicone oil in vitreoretinal surgery: indications, complications, new developments and alternative long-term tamponade agents. Acta Ophthalmologica. 2021;99(3):240–250. doi:10.1111/aos.14604
2. Maghsoudi K, Momen G, Jafari R, Farzaneh M. Direct replication of micro-nanostructures in the fabrication of superhydrophobic silicone rubber surfaces by compression molding. Appl Surf Sci. 2018;458:619–628. doi:10.1016/j.apsusc.2018.07.099
3. Chang C, Lin Y. Competition of aminolysis and alcoholysis in nucleophilic cleavage of a model compound for polysiloxane networks. Polym Degrad Stabil. 2005;87(1):207–211. doi:10.1016/j.polymdegradstab.2004.07.022
4. Moretto H, Schulze M, Wagner G. Silicones, Ullmann’s Encyclopedia of Industrial Chemistry. Weinheim: Wiley-VCH Verlag GmbH & Co. KGaA; 2000.
5. Somasundaran P, Mehta SC, Purohit P. Silicone emulsions. Adv Colloid Interface Sci. 2006;128:103–109. doi:10.1016/j.cis.2006.11.023
6. Barca F, Caporossi T, Rizzo S. Silicone oil: different physical properties and clinical applications. Biomed Res Int. 2014;2014:1–7. doi:10.1155/2014/502143
7. Cibis PA, Becker B, Okun E, Canaan S. The use of liquid silicone in retinal detachment surgery. Archiv Ophthalmol. 1962;68(5):590–599. doi:10.1001/archopht.1962.00960030594005
8. Schwartz SG, Flynn HW, Lee WH, Wang X. Tamponade in surgery for retinal detachment associated with proliferative vitreoretinopathy. Cochrane Database Syst Rev. 2014;2(2):Cd006126. doi:10.1002/14651858.CD006126.pub3
9. Dikopf MS, Patel KH, Setlur VJ, Lim JI. Surgical outcomes of 25-gauge pars plana vitrectomy for diabetic tractional retinal detachment. Eye. 2015;29(9):1213–1219. doi:10.1038/eye.2015.126
10. Fong DS, Ferris FL, Davis MD, Chew EY. Causes of severe visual loss in the early treatment diabetic retinopathy study: ETDRS report no. 24. Am J Ophthalmol. 1999;127(2):137–141. doi:10.1016/S0002-9394(98)00309-2
11. Regler R, Sachs HG, Hillenkamp J, Helbig H, Framme C. Long-term evaluation of anatomic and functional results after complicated retinal detachment treated with pars plana vitrectomy and heavy silicone oil tamponade. Klinische Monatsblatter fur Augenheilkunde. 2009;226(9):707–712. doi:10.1055/s-0028-1109685
12. Berker N, Batman C, Ozdamar Y, Eranil S, Aslan O, Zilelioglu O. Long-term outcomes of heavy silicone oil tamponade for complicated retinal detachment. Eur J Ophthalmol. 2007;17(5):797–803. doi:10.1177/112067210701700518
13. Chang PY, Yang CM, Yang CH, Chen MS, Wang JY. Pars plana vitrectomy for diabetic fibrovascular proliferation with and without internal limiting membrane peeling. Eye. 2009;23(4):960–965. doi:10.1038/eye.2008.334
14. Meier P, Wiedemann P. Vitrectomy for traction macular detachment in diabetic retinopathy. Graefe’s Archive Clin Exper Ophthalmol. 1997;235(9):569–574. doi:10.1007/BF00947086
15. Smiddy WE, Flynn HW. Vitrectomy in the management of diabetic retinopathy. Survey Ophthalmol. 1999;43(6):491–507. doi:10.1016/S0039-6257(99)00036-3
16. Snead DR, James S, Snead MP. Pathological changes in the vitreoretinal junction 1: epiretinal membrane formation. Eye. 2008;22(10):1310–1317. doi:10.1038/eye.2008.36
17. Tamaki K, Usui-Ouchi A, Murakami A, Ebihara N. Fibrocytes and fibrovascular membrane formation in proliferative diabetic retinopathy. Invest Ophthalmol Vis Sci. 2016;57(11):4999–5005. doi:10.1167/iovs.16-19798
18. The Diabetic Retinopathy Vitrectomy Study Research Group. Early vitrectomy for severe proliferative diabetic retinopathy in eyes with useful vision. Results of a randomized trial--Diabetic Retinopathy Vitrectomy Study Report 3. Ophthalmology. 1988;95(10):1307–1320. doi:10.1016/S0161-6420(88)33015-0
19. Castellarin A, Grigorian R, Bhagat N, Del Priore L, Zarbin MA. Vitrectomy with silicone oil infusion in severe diabetic retinopathy. Br J Ophthalmol. 2003;87(3):318–321. doi:10.1136/bjo.87.3.318
20. Morse LS, McCuen BW. The use of silicone oil in uveitis and hypotony. Retina. 1991;11(4):399–404. doi:10.1097/00006982-199111040-00006
21. Lucke KH, Foerster MH, Laqua H. Long-term results of vitrectomy and silicone oil in 500 cases of complicated retinal detachments. Am J Ophthalmol. 1987;104(6):624–633. doi:10.1016/0002-9394(87)90176-0
22. Yeo JH, Glaser BM, Michels RG. Silicone oil in the treatment of complicated retinal detachments. Ophthalmology. 1987;94(9):1109–1113. doi:10.1016/S0161-6420(87)33328-7
23. Brourman ND, Blumenkranz MS, Cox MS, Trese MT. Silicone oil for the treatment of severe proliferative diabetic retinopathy. Ophthalmology. 1989;96(6):759–764. doi:10.1016/S0161-6420(89)32828-4
24. Azen SP, Scott IU, Flynn HW, et al. Silicone oil in the repair of complex retinal detachments. A prospective observational multicenter study. Ophthalmology. 1998;105(9):1587–1597. doi:10.1016/S0161-6420(98)99023-6
25. Er D, Öner H, Kaya M, Dönmez O. Evaluation of the effects of silicone oil on the macula with optical coherence tomography in patients with rhegmatogenous retinal detachment. Turk J Ophthalmol. 2021;51(4):218–224. doi:10.4274/tjo.galenos.2020.48376
26. Lakits A, Nennadal T, Scholda C, Knaus S, Gruber H. Chemical stability of silicone oil in the human eye after prolonged clinical use. Ophthalmology. 1999;106(6):1091–1100. doi:10.1016/S0161-6420(99)90261-0
27. McCurdy HH, Solomons ET. Forensic examination of toxicological specimens for dimethylpolysiloxane (silicone oil). J Anal Toxicol. 1977;1(5):221–223. doi:10.1093/jat/1.5.221
28. Coman Cernat CC, Munteanu M, Patoni Popescu SI, Mușat O. Silicone oil complications in vitreoretinal surgery. Rom J Ophthalmol. 2022;66(4):299–303. doi:10.22336/rjo.2022.55
29. Rabina G, Azem N, Barequet D, Barak A, Loewenstein A, Schwartz S. Silicone oil tamponade effect on macular layer thickness and visual acuity. Retina. 2020;40(5):998–1004. doi:10.1097/IAE.0000000000002464
30. Al-Dwairi R, Ahmad AA, Aleshawi A, et al. Optical and physical properties of silicone oil extracted from the vitreous of patients who underwent vitrectomy for retinal detachment. J Ocular Pharmacol Therap. 2022;38(10):717–727. doi:10.1089/jop.2022.0081
31. Yilmaz T, Güler M. The Role of Nystagmus in Silicone Oil Emulsification After Pars Plana Vitrectomy and Silicone Oil Injection for Complex Retinal Detachment. London, England: SAGE Publications Sage UK; 2008.
32. Caramoy A, Hagedorn N, Fauser S, Kugler W, Groß T, Kirchhof B. Development of emulsification-resistant silicone oils: can we go beyond 2000 mPas silicone oil? Investigat Ophthalmol Visual Sci. 2011;52(8):5432–5436. doi:10.1167/iovs.11-7250
33. Caramoy A, Schröder S, Fauser S, Kirchhof B. In vitro emulsification assessment of new silicone oils. Br J Ophthalmol. 2010;94(4):509–512. doi:10.1136/bjo.2009.170852
34. Stappler T, Morphis G, Irigoyen C, Heimann H. Is there a role for long-term silicone oil tamponade for more than twelve months in vitreoretinal surgery? Ophthalmologica. 2011;226(Suppl. 1):36–41. doi:10.1159/000328208
35. Toklu Y, Cakmak HB, Ergun ŞB, Yorgun MA, Simsek Ş. Time course of silicone oil emulsification. Retina. 2012;32(10):2039–2044. doi:10.1097/IAE.0b013e3182561f98
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

