Back to Journals » Clinical Ophthalmology » Volume 18
Short-Term Outcomes of 3 Monthly intravitreal Faricimab On Different Subtypes of Neovascular Age-Related Macular Degeneration
Authors Tanaka A, Hata M, Tsuchikawa M, Ueda-Arakawa NUA, Tamura H , Miyata M, Takahashi A, Kido A, Muraoka Y , Miyake M, Ooto S, Tsujikawa A
Received 6 November 2023
Accepted for publication 15 January 2024
Published 20 February 2024 Volume 2024:18 Pages 507—516
DOI https://doi.org/10.2147/OPTH.S448507
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Asako Tanaka, Masayuki Hata, Memiri Tsuchikawa, Naoko Ueda-Arakawa Ueda-Arakawa, Hiroshi Tamura, Manabu Miyata, Ayako Takahashi, Ai Kido, Yuki Muraoka, Masahiro Miyake, Sotaro Ooto, Akitaka Tsujikawa
Department of Ophthalmology and Visual Sciences, Kyoto University Graduate School of Medicine, Kyoto, Japan
Correspondence: Masayuki Hata, Department of Ophthalmology and Visual Sciences Kyoto University Graduate School of Medicine, Sakyo-ku, Kyoto, 606-8507, Japan, Tel +81-75-751-3248, Fax +81-75-752-0933, Email [email protected]
Purpose: To evaluate the efficacy and safety of faricimab injections for treatment-naïve neovascular age-related macular degeneration (nvAMD) patients, including subtypes and pachychoroid phenotypes, and identify predictive factors for visual outcomes.
Methods: nvAMD patients were prospectively recruited, receiving three monthly faricimab (6 mg) injections. Best-corrected visual acuity (BCVA) two months after the last injection (month 4) was compared between subtypes, and between pachychoroid neovasculopathy (PNV) and non-PNV eyes. Regression analysis determined factors influencing month 4 BCVA.
Results: The study involved 23 patients (12 typical AMD [tAMD], 10 polypoidal choroidal vasculopathy [PCV], 1 retinal angiomatous proliferation [RAP]). Eleven exhibited PNV phenotype. Significant BCVA (P = 4.9 × 10− 4) and central retinal thickness (CRT) (P = 1.3 × 10− 5) improvements were observed post-faricimab treatment. The therapy demonstrated favourable results for both tAMD and PCV eyes, and non-PNV and PNV eyes. Faricimab achieved dry macula in 77.3% of eyes, with subretinal fluid resolution in most cases, although intraretinal fluid (IRF) often persisted. Multivariable analysis identified external limiting membrane (ELM) presence and IRF as BCVA contributors at month 4.
Conclusion: Faricimab demonstrated significant effectiveness and safety in treatment-naïve nvAMD patients, particularly for PCV and PNV eyes. ELM presence and IRF is predictive of visual outcomes.
Keywords: anti-VEGF, anti-vascular endothelial growth factor, CRT, central retinal thickness, ELM, external limiting membrane, faricimab, IRF, intraretinal fluid, MNV, macular neovascularization, nvAMD, neovascular age-related macular degeneration, PCV, polypoidal choroidal vasculopathy, PNV, pachychoroid neovasculopathy, RAP, retinal angiomatous proliferation
Introduction
Age-related macular degeneration (AMD) is a leading cause of blindness worldwide, affecting individuals in North America, Europe, Australia, and Asia.1 Late AMD is classified into two types: geographic atrophy and neovascular AMD (nvAMD). Pathological neovascularization of the choroidal blood vessels underneath the macula or intraretinal neovascularization (macular neovascularization, MNV) is observed in patients with nvAMD, which rapidly compromises their central visual field. Over the past decade, standards of care for nvAMD have primarily focused on targeting vascular endothelial growth factor-A (VEGF-A). Intravitreal injection of anti-VEGF drugs, such as ranibizumab and aflibercept, is considered the first-line therapy for nvAMD.2,3 However, over 10% of patients show a suboptimal response to anti–VEGF therapy.4,5 Additionally, frequent injections of anti–VEGF therapy are required to maintain the vision gain achieved during the loading phase, resulting in treatment burden and possibly macular atrophy.6–8 Brolucizumab, which was recently approved as an anti-VEGF agent based on the HAWK and HARRIER, has demonstrated better fluid control and longer dosing intervals.9 However, there are significant concerns regarding intraocular inflammation, including retinal occlusive vasculitis, following intravitreal brolucizumab treatment, which can result in permanent vision loss.10 Therefore, new therapeutic approaches, including novel agents that target other pathways involved in nvAMD that exhibit acceptable safety profiles while potentially being more effective, must be explored.
Faricimab, an innovative bispecific monoclonal antibody, has been specifically designed for intraocular use through intravitreal injection, to target two distinct pathways by binding and neutralizing both VEGF-A and angiopoietin-2 (Ang-2) simultaneously.11,12 Anti–Ang-2 stabilizes vessels, reduces vascular leakage, and alleviates inflammation, whereas anti–VEGF-A inhibits neovascularization in addition to reducing vascular leakage.11 The efficacy of faricimab in nvAMD has been demonstrated in the pivotal Phase 3 TENAYA and LUCERNE trials.13,14 Data from the phase 3 global trials indicate that dosing of faricimab up to every 16 weeks (Q16W) was non-inferior to aflibercept Q8W in terms of changes in best-corrected visual acuity (BCVA) from baseline. Additionally, rates of ocular adverse events were comparable between faricimab Q16W and aflibercept Q8W.13 These results suggest that faricimab may overcome some of the limitations of existing anti-VEGF drugs in treating nvAMD. Therefore, real-world evidence on the use of faricimab is highly desirable. In addition, although the efficacy of anti-VEGF therapy differs among the subtypes of nvAMD15 and eyes with pachychoroid phenotypes,16 the current literature lacks data on the efficacy of faricimab in these populations.
In this study, we investigated the effectiveness and safety of three monthly intravitreal injections of faricimab in treatment-naïve patients with nvAMD. We also evaluated the differences in treatment effects by subtypes and with and without pachychoroid phenotypes.
Methods
Study Design
This prospective, non-randomised, observational study was conducted in an institutional setting. The study design was approved by the Institutional Review Board (IRB) of Kyoto University Graduate School of Medicine (R0532). All study conduct adhered to the tenets of the Declaration of Helsinki. Prior to enrolment, each patient provided written informed consent to participate in this study.
Study Population
Participants were recruited at Kyoto University Hospital between June 2022 and October 2022. The inclusion criteria were age >50 years, axial length <26.5 mm, presence of nvAMD, and willingness to participate in the study. Only one eye from each patient was included in the study and the other eye was not considered if it developed AMD. The exclusion criteria comprised previous treatment for MNV, and the presence of other retinal diseases, such as retinal vein or artery occlusion, diabetic retinopathy, angioid streaks, and vitelliform macular dystrophy. Patients with a chronic course of AMD, as indicated by disease history and/or massive fibrotic lesions, were also excluded. Those who dropped out of the study were not included in the analysis.
Intervention and Observation Procedure
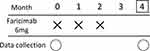
All participants received 3 monthly faricimab injections (6.0 mg). We collected clinical data at baseline and 2 months after the third faricimab injection (month 4; Figure 1). If patients did not show subretinal fluid (SRF) or intraretinal fluid (IRF) at month 4, their clinical data were collected at month 5.
The patients underwent comprehensive examinations, including BCVA measurement with Landolt C charts (Takagi Seiko, Nakano, Japan),17 fundus photography, measurement of axial length (IOL Master, Carl Zeiss Meditec, Dublin, California, USA), fluorescein angiography (FA), indocyanine green angiography (IGA), fundus autofluorescence imaging (HRA2; Heidelberg Engineering), and spectral-domain optical coherence tomography (SD-OCT; Spectralis; Heidelberg Engineering, Heidelberg, Germany) at baseline. We performed fundus photography, angiography, fundus autofluorescence imaging, and SD-OCT under pupillary dilation. Visual acuity measurements and SD-OCT were also performed in month 4, and the results at baseline and month 4 were analysed. The SD-OCT images were obtained using Spectralis and Heidelberg Eye Explorer (version 1.8.6.0; Heidelberg Engineering). Thirty-degree horizontal and vertical scans through the fovea were recorded using normal and enhanced depth imaging modes, with an average of 100 scans.18
The measurements of central retinal thickness (CRT), defined as the distance between the vitreoretinal surface and the inner surface of the retinal pigment epithelium (RPE), and subfoveal choroidal thickness (SFCT), defined as the length between the outer border of the Bruch’s membrane and the chorioscleral interface, were done in horizontal and vertical scans and subsequently averaged. SFCT was measured using enhanced depth imaging scans. Height of pigment epithelium detachment (PED) was defined as the distance between the outer border of the retinal pigment epithelium and the inner border of the Bruch’s membrane. The subretinal hyperreflective material (SHRM) was identified in the subretinal space19 and the SHRM height was defined as the distance between the inner surface of the hyperreflective material and the inner surface of the RPE. Graders reviewed all the B scans to determine and measure the maximum PED and SHRM heights in the raster scans. Furthermore, the presence of the foveal external limiting membrane (ELM) and ellipsoid zone (EZ) were evaluated using vertical and horizontal scans. The presence of vitreoretinal adhesions was assessed using raster scanning. The presence of fluid accumulation was determined using SD-OCT at month 4. A dry macula was defined as the complete resolution of intraretinal (IRF) and/or subretinal fluid (SRF) detected on SD-OCT raster scans. The persistence of only PED was considered indicative of a dry macula.
We evaluated the presence of polypoidal lesions using indocyanine green angiography at baseline. Polypoidal choroidal vasculopathy (PCV) was diagnosed based on the finding of characteristic polypoidal lesions at the border of the branching choroidal vascular networks. Patients with signs of retinochoroidal anastomosis were diagnosed with retinal angiomatous proliferation (RAP), whereas others were diagnosed with typical AMD (tAMD).
Definition of Pachychoroid Neovasculopathy
In this study, pachychoroid neovasculopathy (PNV) was diagnosed according to the following criteria20,21: (1) MNV in either eye and (2) clinical features of the pachychoroid phenotype22 such as reduced fundus tessellation in fundus photographs, choroidal vascular hyperpermeability (CVH) in IA images, and dilated choroidal vessels in SD-OCT and IA images. Dilated choroidal vessels were defined as dilated outer choroidal vessels with attenuation and thinning of the choriocapillaris on OCT.22 In IA, dilated choroidal vessels extended from one or more vortex veins;23 (3) there was none or only non-extensive hard drusen in both eyes (Age-Related Eye Disease Study [AREDS] level 1, no AMD24). Diagnoses were made by two ophthalmologists, and in case of discrepancy, a senior retinal specialist determined the final diagnosis.
Outcome Measures
Main outcome measure was a change in visual acuity. Secondary outcome measures included subgroup comparisons between patients with and without PNV and those with AMD subtypes. Additionally, we performed a multivariable regression analysis to identify baseline characteristics predicting visual outcomes.
Statistical Analysis
Statistical analysis was performed using SPSS version 21 (IBM Japan, Tokyo, Japan) with a significant P-value set at <0.05. Visual acuity measured with Landolt C charts was converted to the logarithm of the minimal angle of resolution (logMAR) for statistical analysis. To compare baseline characteristics, visual acuity, CRT, SFCT, PED height, and SHRM height between PNV and non-PNV, PCV and tAMD, and eyes with and without fluid at month 4, unpaired t-test or Fisher’s exact test was applied. A paired t-test was used to compare baseline and month 4 values. Bivariate relationships were examined using the Pearson correlation coefficient for continuous variables and the Spearman correlation coefficient test for binary variables. Stepwise multivariable regression analysis was performed with age, presence of polypoidal lesions, presence of IRF and/or SRH, CRT, maximum SHRM, and presence of ELM as independent factors, and visual acuity at month 4 as a dependent factor.
Results
This study included 24 patients who met the eligibility criteria with one patient dropping out after the second injection for unknown reasons. Thus, the final study sample size was 23 patients, consisting of 12 patients with tAMD, 10 with PCV, and 1 with RAP. One patient developed a retinal pigment epithelium tear as an adverse event but no other ocular complications, such as intraocular inflammation or systemic extraocular complications, were observed.
The baseline characteristics of the study participants are presented in Table 1. The mean age of patients was 75.4 ± 7.6 years and baseline BCVA was 0.29 ± 0.30 logMAR (20/39). BCVA significantly improved to 0.18 ± 0.32 logMAR (20/30) two months after the third injection (month 4) (P = 4.9 × 10−4, Figure 2A). Regardless of the subtype (PCV or tAMD), BCVA significantly improved (Figure 2B). In addition, significant improvements were observed in OCT parameters, where CRT and maximum SHRM height significantly decreased from 324.5 ± 193.2 µm to 164.3 ± 90.1 µm (P = 1.3 × 10−5, Figure 2C), and 159.3 ± 127.0 to 44.6 ± 132.3 (P = 5.0 × 10−6, Figure 2D) respectively. For the effects of treatments on the structures under the RPE, SFCT, and PED height significantly reduced from 287.8 ± 103.1 to 259.7 ± 103.2 µm (P = 1.1 × 10−2, Figure 2E), and 244.1 ± 182.9 to 145.8 ± 89.6 µm (P = 7.2 × 10−3, Figure 2F) respectively.
 |
Table 1 Baseline Demographic and Clinical Characteristics of Patients with Neovascular Age-Related Macular Degeneration |
Among the 23 eyes, 11 showed pachychoroid phenotypes (PNV) and 12 did not (non-PNV). Comparing baseline characteristics between eyes with PNV and non-PNV, PNV eyes had a higher frequency of CVH (81.2% vs 8.3%, P = 6.0 × 10−4) and significantly greater SFCT as expected (333.1 ± 100.8 vs 246.3 ± 86.3 µm, P = 4.6 × 10−2) (Table 2). After 3 monthly faricimab injections, BCVA showed favourable results in both non-PNV eyes and PNV eyes at month 4 (P = 4.1 × 10−2 and 1.1 × 10−3, respectively, Figure 3A). Faricimab significantly decreased SFCT in PNV (12.5% reduction in SFCT, P = 5.0 × 10−3; Figure 3B) and decreased CRT, PED height, and SHRM height in both non-PNV (P = 3.0 × 10−3, 4.1 × 10−2, and 3.0 × 10−3, respectively), and PNV eyes (P = 2.0 × 10−3, 1.8 × 10−2, and 1.0 × 10−3, respectively) (Figure 3C–E).
 |
Table 2 Comparison of Baseline Characteristics Between Neovascular AMD Patients with and without Pachychoroid Phenotypse |
We explored predictive factors for visual outcomes. The univariate analysis showed that age, CRT, maximum SHRM height, and presence of foveal ELM, IRF, and SRH were associated with visual acuity at month 4 (Table 3). A multiple regression model analysis was performed, yielding significant overall regression (R2 = 0.788, P < 1.0 × 10−3), indicating that 78.8% of the visual outcomes could be explained by the selected factors. Among the possible predictive factors, the presence of ELM and the absence of IRF were identified as contributing factors to better visual acuity at month 4 (Table 4).
 |
Table 3 Predictive Factors of Visual Acuity at Month 4 in Patients with Faricimab |
 |
Table 4 Results of Multiple Linear Regression After Step-Wise Selection in Patients Treated with Faricimab |
Dry macula was achieved in 77.3% of eyes at month 4 (P < 0.0001); although faricimab completely resolved SRF in most cases (from 100% to 9.1%, P < 1.0 × 10−4), IRF often persisted (from 21.7% to 13.6%, P = 7.0 × 10−1) (Figure 4A). Among eyes with dry macula at month 4, 58.8% remained dry one month later (month 5). Upon comparing eyes with and without fluid at month 4, although CRT significantly decreased in both groups (Figure 4B), VA improved in eyes without fluid (P = 5.5 × 10−4) only and not in eyes with fluid (P = 6.6 × 10−1) (Figure 4C).
Discussion
In the present study, we demonstrated the effectiveness and safety of three monthly intravitreal injections of faricimab in treatment-naïve patients with nvAMD, including those with and without pachychoroid phenotypes. Our results indicated that faricimab injections improved anatomical outcomes both above and below the RPE (CRT and SHRM, SFCT and PED, respectively). Notably, faricimab was effective not only in patients with tAMD but also in PCV as well as PNV. Dry macula was achieved in 77.3% of the eyes two months after the third injection, with 58.8% of these eyes remaining dry one month later, suggesting a prolonged treatment effect after the last dose in approximately half of the eyes. Furthermore, multivariable analysis identified the presence of ELM and IRF as factors contributing to visual outcomes.
Our findings are consistent with the results of the pivotal phase 3 TENAYA and LUCERNE trials, which demonstrated the non-inferiority of faricimab dosed up to Q16W compared to aflibercept Q8W, with similar ocular adverse event rates, and those of the retrospective clinical studies.13,14,25,26 Our study extends these previous findings by examining the efficacy of faricimab in different subtypes of nvAMD, including tAMD and PCV, and PNV and non-PNV eyes. Although several studies have reported that nvAMD subtypes can affect disease management15,27 we found that faricimab treatment resulted in significant improvements in BCVA in both the PCV and tAMD subtypes, suggesting that faricimab may be effective in managing a range of nvAMD presentations. However, further studies with longer follow-up periods are necessary to confirm the long-term safety and efficacy of faricimab. Overall, our study provides promising evidence for the real-world application of faricimab in patients with nvAMD.
PNV is a novel clinical entity of MNV driven by pachychoroid phenotypes, which indicate choroidal manifestations, including thickened choroid and dilated outer choroidal vessels.16,28 The significant decrease in SFCT observed in our study, especially in PNV eyes, suggests that faricimab may effectively target the underlying choroidal abnormalities associated with pachychoroid phenotypes. This finding is essential as previous reports have shown the suboptimal efficacy of anti-VEGF agents (ranibizumab, aflibercept, and bevacizumab) for PNV treatment.29 We and others have previously revealed that the molecular mechanisms involved in angiogenesis differ between PNV and non-PNV eyes.21 Notably, the upregulation of Ang-2 was found in the aqueous humour of treatment-naïve patients with PNV.30 The bispecific action of faricimab, which targets both VEGF-A and Ang-2, may therefore be crucial in addressing the complex pathophysiology of PNV. Further, though targeting both VEGF and Ang-2 by Faricimab may offer enhanced efficacy for PNV compared to other anti-VEGF agents, it is important to note that our current study did not include a direct comparison between Faricimab and other anti-VEGF treatments. Because our study’s scope was limited to its efficacy within the context of PNV without comparative analysis to other treatments, future studies specifically designed to compare Faricimab with other anti-VEGF agents would be invaluable to substantiate this hypothesis and provide more definitive conclusions.
Our multivariable analysis identified the presence of ELM and IRF at baseline emerged as factors contributing to visual acuity at month 4. These findings align with those of previous studies that have reported the presence of ELM as a predictor of better visual outcomes following anti-VEGF therapy.31 The association between IRF presence before treatments and poorer visual outcomes underscores the importance of addressing fluid accumulation in the management of patients with nvAMD. The reasons for the potential negative impact of IRF on BCVA are not well understood, and it has been suggested that IRF may be indicative of a more aggressive lesion type or a late sign of the chronic stage of MNV.32 Despite a significant reduction in SRF following faricimab treatment as demonstrated in our study, IRF often persisted, highlighting the need for further investigation into the management of intraretinal fluid in patients with nvAMD.
A key strength of our study lies in its evaluation of faricimab treatment in a real-world setting, which complements the findings from the TENAYA and LUCERNE trials. Additionally, the inclusion of nvAMD subtypes and investigation of treatment effects in eyes with and without PNV provide valuable insights into the potential benefits of faricimab across different patient populations. However, our study has several limitations, including a small sample size and a relatively short follow-up period. We understand that the small sample size may impact the generalizability of our findings, but our results can be a valuable preliminary indicator and a basis for future studies. We believe that our findings contribute to the field, offering initial insights that can be further explored in subsequent research. Future studies with larger sample sizes and longer follow-up periods are needed to provide further evidence of the long-term efficacy and safety of faricimab in patients with nvAMD.
In conclusion, our findings provide compelling evidence supporting the effectiveness and safety of faricimab in treatment-naïve patients with nvAMD. The favourable outcomes observed in both PNV and non-PNV eyes suggest their potential as promising therapeutic options for a wide range of patients with nvAMD. Half of the treated eyes retained dry macula 3 months after the last dose, indicating the possibility of extending the dosing interval compared to conventional anti-VEGF agents, such as ranibizumab and aflibercept. However, further comparative studies are needed to confirm the long-term benefits of faricimab and optimise treatment regimens tailored to individual patients.
Funding
This work was supported in part by a Grant-in-Aid for Scientific Research (No. 21H03092) from the Japan Society for the Promotion of Science (Tokyo, Japan).
Disclosure
M Hata: Novartis Pharma, Senju Pharmaceutical, Alcon Research Institute, and Kyoto Drug Discovery and Development; A. N Ueda-Arakawa: Santen Pharmaceutical, Novartis Pharma, and Chugai Pharmaceutical; H. Tamura: Findex, Bayer Yakuhin, Novartis Pharma, Santen Pharmaceutical, SUNTORY, and Otsuka Pharmaceutical; M Miyata: Alcon Japan, Novartis Pharma, Santen Pharmaceutical, HOYA, Bayer Yakuhin, Senju Pharmaceutical, and Kowa Pharmaceutical; A. Takahashi: Bayer Yakuhin, Novartis Pharma, Santen Pharmaceutical, and MSD; Y. Muraoka: Rohto Pharmaceutical, Bayer Yakuhin, Novartis Pharma, Alcon Japan, Canon, Santen Pharmaceutical, Senju Pharmaceutical, AMO Japan, HOYA, Johnson & Johnson K.K.; M Miyake: Novartis Pharma, Bayer Yakuhin, Kowa Pharmaceutical, Alcon Japan, AMO Japan, Santen Pharmaceutical, Senju Pharmaceutical, Johnson and Johnson K. K., and Chugai Pharmaceutical; S. Ooto: Bayer Yakuhin, Kowa Pharmaceutical, Janssen Pharmaceutical, Novartis Pharma, AMO Japan, Santen Pharmaceutical, Alcon Japan, and Senju Pharmaceutical; A. Tsujikawa: Canon, Findex, Santen Pharmaceutical, Kowa Pharmaceutical, Pfizer, Sumitomo Pharma, Rhoto Pharmaceutical, Nippon Boehringer Ingelheim, Nidek, Johnson & Johnson, Nikon Solutions, AMO Japan, Senju Pharmaceutical, Wakamoto Pharmaceutical, Alcon Japan, Alcon Pharma, Otsuka Pharmaceutical, Tomey Corporation, Taiho Pharma, Hoya, Bayer Yakuhin, Novartis Pharma, Chugai Pharmaceutical, Astellas, Eisai, Daiich-Sankyo, Janssen Pharmaceutical, Kyoto Drug Discovery and Development, Allergan Japan, MSD, Ellex, HOYA, Sanwa Kagaku Kenkyusho, Nitten Pharmaceutical, and AbbVie GK. The authors report no other conflicts of interest in this work.
References
1. Wong W. Managed care opportunities and approaches to select treatment for sight preservation. Am J Manag Care. 2020;26:S112–S117. doi:10.37765/ajmc.2020.43436
2. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–1431. doi:10.1056/NEJMoa054481
3. Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119(12):2537–2548. doi:10.1016/j.ophtha.2012.09.006
4. Krebs I, Glittenberg C, Ansari-Shahrezaei S, et al. Non-responders to treatment with antagonists of vascular endothelial growth factor in age-related macular degeneration. Br J Ophthalmol. 2013;97(11):1443–1446. doi:10.1136/bjophthalmol-2013-303513
5. Nagai N, Suzuki M, Uchida A, et al. Non-responsiveness to intravitreal aflibercept treatment in neovascular age-related macular degeneration: implications of serous pigment epithelial detachment. Sci Rep. 2016;6(6):29619. doi:10.1038/srep29619
6. Maguire MG, Martin DF, Ying GS, et al. Five-year outcomes with anti-vascular endothelial growth factor treatment of neovascular age-related macular degeneration: the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2016;123(8):1751–1761. doi:10.1016/j.ophtha.2016.03.045
7. Holz FG, Tadayoni R, Beatty S, et al. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br J Ophthalmol. 2015;99(2):220–226. doi:10.1136/bjophthalmol-2014-305327
8. Ohji M, Takahashi K, Okada AA, et al. Efficacy and safety of intravitreal aflibercept treat-and-extend regimens in exudative age-related macular degeneration: 52- and 96-week findings from ALTAIR: a randomized controlled trial. Adv Ther. 2020;37(3):1173–1187. doi:10.1007/s12325-020-01236-x
9. Dugel PU, Singh RP, Koh A, et al. HAWK and HARRIER: ninety-six-week outcomes from the phase 3 trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology. 2021;128(1):89–99. doi:10.1016/j.ophtha.2020.06.028
10. Mones J, Srivastava SK, Jaffe GJ, et al. Risk of inflammation, retinal vasculitis, and retinal occlusion-related events with brolucizumab: post hoc review of HAWK and HARRIER. Ophthalmology. 2021;128(7):1050–1059. doi:10.1016/j.ophtha.2020.11.011
11. Regula JT, Lundh von Leithner P, Foxton R, et al. Targeting key angiogenic pathways with a bispecific crossmab optimized for neovascular eye diseases. EMBO Mol Med. 2016;8(11):1265–1288. doi:10.15252/emmm.201505889
12. Sharma N, Kumar N, Kuppermann BD, et al. Faricimab: expanding horizon beyond VEGF. Eye. 2020;34(5):802–804. doi:10.1038/s41433-019-0670-1
13. Heier JS, Khanani AM, Quezada Ruiz C, et al. Efficacy, durability, and safety of intravitreal faricimab up to every 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): two randomised, double-masked, phase 3, non-inferiority trials. Lancet. 2022;399(10326):729–740. doi:10.1016/S0140-6736(22)00010-1
14. Mori R, Honda S, Gomi F, et al. Efficacy, durability, and safety of faricimab up to every 16 weeks in patients with neovascular age-related macular degeneration: 1-year results from the Japan subgroup of the phase 3 TENAYA trial. Jpn J Ophthalmol. 2023;67(3):301–310. doi:10.1007/s10384-023-00985-w
15. Hata M, Tsujikawa A, Miyake M, et al. Two-year visual outcome of ranibizumab in typical neovascular age-related macular degeneration and polypoidal choroidal vasculopathy. Graefes Arch Clin Exp Ophthalmol. 2015;253(2):221–227. doi:10.1007/s00417-014-2688-1
16. Miyake M, Ooto S, Yamashiro K, et al. Pachychoroid neovasculopathy and age-related macular degeneration. Sci Rep. 2015;5(1):16204. doi:10.1038/srep16204
17. Kuo HK, Kuo MT, Tiong IS, et al. Visual acuity as measured with landolt c chart and early treatment of diabetic retinopathy study chart. Graefes Arch Clin Exp Ophthalmol. 2011;249(4):601–605. doi:10.1007/s00417-010-1461-3
18. Spaide RF, Koizumi H, Pozzoni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol. 2008;146(4):496–500. doi:10.1016/j.ajo.2008.05.032
19. Kawashima Y, Hata M, Oishi A, et al. Association of vascular versus avascular subretinal hyperreflective material with aflibercept response in age-related macular degeneration. Am J Ophthalmol. 2017;181:61–70. doi:10.1016/j.ajo.2017.06.015
20. Tagawa M, Ooto S, Yamashiro K, et al. Characteristics of pachychoroid neovasculopathy. Sci Rep. 2020;10(1):16248. doi:10.1038/s41598-020-73303-w
21. Hata M, Yamashiro K, Ooto S, et al. Intraocular vascular endothelial growth factor levels in pachychoroid neovasculopathy and neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci. 2017;58(1):292–298. doi:10.1167/iovs.16-20967
22. Dansingani KK, Balaratnasingam C, Naysan J, et al. En face imaging of pachychoroid spectrum disorders with swept-source optical coherence tomography. Retina. 2016;36(3):499–516. doi:10.1097/IAE.0000000000000742
23. Pang CE, Shah VP, Sarraf D, et al. Ultra-widefield imaging with autofluorescence and indocyanine green angiography in central serous chorioretinopathy. Am J Ophthalmol. 2014;158(2):362–371.e2. doi:10.1016/j.ajo.2014.04.021
24. Age-Related Eye Disease Study Research Group. The age-related eye disease study system for classifying age-related macular degeneration from stereoscopic color fundus photographs: the age-related eye disease study report number 6. Am J Ophthalmol. 2001;132(5):668–681. doi:10.1016/S0002-9394(01)01218-1
25. Matsumoto H, Hoshino J, Nakamura K, et al. Short-term outcomes of intravitreal faricimab for treatment-naïve neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2023;261(10):2945–2952. doi:10.1007/s00417-023-06116-y
26. Mukai R, Kataoka K, Tanaka K, et al. Three-month outcomes of faricimab loading therapy for wet age-related macular degeneration in Japan. Sci Rep. 2023;13(1):8747. doi:10.1038/s41598-023-35759-4
27. Maruko M, Ogasawara M, Yamamoto A, et al. Two-year outcomes of treat-and-extend intravitreal aflibercept for exudative age-related macular degeneration: a prospective study. Ophthalmol Retina. 2020;4(8):767–776. doi:10.1016/j.oret.2020.03.010
28. Pang CE, Freund KB. Pachychoroid neovasculopathy. Retina. 2015;35(1):1–9. doi:10.1097/IAE.0000000000000331
29. Chang YC, Cheng CK. Difference between pachychoroid and nonpachychoroid polypoidal choroidal vasculopathy and their response to anti-vascular endothelial growth factor therapy. Retina. 2020;40(7):1403–1411. doi:10.1097/IAE.0000000000002583
30. Inoda S, Takahashi H, Inoue Y, et al. Cytokine profiles of macular neovascularization in the elderly based on a classification from a pachychoroid/drusen perspective. Graefes Arch Clin Exp Ophthalmol. 2022;260(3):747–758. doi:10.1007/s00417-021-05445-0
31. Oishi A, Tsujikawa A, Yamashiro K, et al. One-year result of aflibercept treatment on age-related macular degeneration and predictive factors for visual outcome. Am J Ophthalmol. 2015;159(5):853–860.e1. doi:10.1016/j.ajo.2015.01.018
32. Schmidt-Erfurth U, Waldstein SM. A paradigm shift in imaging biomarkers in neovascular age-related macular degeneration. Prog Retin Eye Res. 2016;50:1–24. doi:10.1016/j.preteyeres.2015.07.007
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.