Back to Journals » Clinical Ophthalmology » Volume 16
Short-Term Efficacy of Combined ab Interno Canaloplasty and Trabeculotomy in Pseudophakic Eyes with Open-Angle Glaucoma
Authors Bleeker AR, Litchfield WR, Ibach MJ , Greenwood MD, Ristvedt D, Berdahl JP , Terveen DC
Received 10 April 2022
Accepted for publication 5 July 2022
Published 21 July 2022 Volume 2022:16 Pages 2295—2303
DOI https://doi.org/10.2147/OPTH.S367896
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Adam R Bleeker,1 William R Litchfield,2 Mitch J Ibach,3 Michael D Greenwood,4 Deborah Ristvedt,5 John P Berdahl,3 Daniel C Terveen3
1Dean McGee Eye Institute, Oklahoma City, OK, USA; 2University of North Dakota School of Medicine, Grand Fords, ND, USA; 3Vance Thompson Vision, Sioux Falls, SD, USA; 4Vance Thompson Vision, West Fargo, ND, USA; 5Vance Thompson Vision, Alexandria, MN, USA
Correspondence: Adam R Bleeker, Dean McGee Eye Institute – Oklahoma Health Center, 608 Stanton L Young Blvd, Oklahoma City, OK, 73104, USA, Tel +1 605-630-9023, Email [email protected]
Purpose: To evaluate short-term outcomes of combined ab interno canaloplasty and trabeculotomy in pseudophakic eyes with open-angle glaucoma.
Patients and Methods: Series included all pseudophakic eyes with open-angle glaucoma treated with up to 360° ab interno canaloplasty and up to 360° ab interno trabeculotomy using a purpose-engineered device (OMNI, Sight Sciences Inc). Data collected prior to surgery and out to 6-months postoperative. Surgical success defined as a 20% reduction in intraocular pressure (IOP) without increase in glaucoma medication, or discontinuation of at least one glaucoma medication without increase in IOP. Other primary endpoints included mean IOP and number of glaucoma medications.
Results: The study included 67 eyes of 52 patients with a mean age of 76.5 ± 8.9 years. Preoperative mean IOP was 22.1± 8.0 mmHg on 2.3± 1.4 glaucoma medications. Pressure lowering effects were sustained out to 6 months postoperative with a mean IOP of 15.2± 4.9 mmHg (p < 0.001) and mean medication reduction of 0.7± 1.4 (p < 0.001). Surgical success rate was 69.8% (30 eyes) and correlated with preoperative IOP. Two patients required a secondary surgical intervention.
Conclusion: Combined ab interno canaloplasty and trabeculotomy as a standalone procedure is an effective means of reducing IOP and medication burden in pseudophakic eyes with open-angle glaucoma.
Keywords: glaucoma, pseudophakia, MIGS, Schlemm canal
Introduction
The use of microinvasive glaucoma surgery (MIGS) is rapidly gaining acceptance as a first-line surgical intervention for glaucoma patients.1 The efficacy, safety and quick recovery of these techniques have driven this change and given surgeons the confidence to intervene earlier in the treatment paradigm in eyes that may not be good candidates for filtering surgery.
MIGS is frequently combined with cataract surgery as an adjunctive procedure; however, as the safety and efficacy of MIGS procedures continues to be demonstrated, it is now often considered as a standalone procedure.2 In patients without a concomitant cataract, the risk to benefit profile changes as the MIGS procedure must bear the full risk of entering the eye as opposed to combined surgery where that risk coexists between the cataract and the MIGS procedure. In order to justify the risk, a MIGS procedure needs to demonstrate sufficient safety and efficacy.
MIGS is increasingly being used in patients with severe glaucoma, especially when filtering or conjunctival altering procedures are a poor option. In these situations, the reduced risk of a MIGS surgery often make them the best option or, in some cases, the only option to reduce medication burden or lower IOP.3
It has been well established that the conventional outflow path is the primary location for resistance and elevated IOP in open-angle glaucoma (OAG).4–6 The trabecular meshwork, Schlemm’s canal, and collector channels all play an important role in this increased resistance. In 2014, gonioscopy-assisted transluminal trabeculotomy (GATT) was described as a novel means of addressing proximal outflow resistance by advancing a microcatheter or suture circumferentially within Schlemm’s canal followed by up to 360̊ ab interno trabeculotomy.7 Other ab interno trabeculotomy devices were designed to remove trabecular meshwork, but unlike GATT were limited to the nasal arc.8,9 In comparison, ab interno canaloplasty (ABiC) was developed as a means of reducing distal outflow resistance.10 The OMNI surgical system (Sight Sciences Inc, Menlo Park, CA) is a purpose built device capable of performing up to 360° ab interno canaloplasty and trabeculotomy through a single clear corneal incision.11 By addressing proximal and distal areas of outflow resistance, the OMNI surgical system has the potential to provide the appropriate balance of safety and efficacy, perhaps justifying the increased risk born by a standalone procedure.
Few studies have addressed the use of this device as a standalone procedure, and while preliminary studies have shown promising results they do not include patients with severe glaucoma.12–15 The purpose of this study was to retrospectively evaluate the outcomes of the OMNI surgical system as a standalone procedure in pseudophakic eyes with open angle glaucoma.
Materials and Methods
Study Design
The study was a retrospective, consecutive case series of pseudophakic eyes with open-angle glaucoma having underwent ab interno canaloplasty and trabeculotomy as a standalone procedure. Surgeries were performed by three experienced MIGS surgeons (JB, MG, and DR) at three ambulatory surgery centers in Sioux Falls, South Dakota; Fargo, North Dakota; and Alexandria, Minnesota. The study received IRB approval by the University of South Dakota. Additionally, a waiver of the process of informed consent and a full waiver of HIPAA authorization were granted due to the study’s retrospective nature. Data collection was conducted in accordance with the principles outlined by the Declaration of Helsinki.
All eyes carried a preoperative diagnosis of OAG including primary open-angle glaucoma (POAG) and pseudoexfoliative glaucoma (PXF). Other forms of secondary open-angle glaucoma (steroid-induced, uveitic, and traumatic) were excluded. The severity of disease was based on a combination of clinical judgment and the American Academy of Ophthalmology’s Preferred Practice Guidelines.1 Preoperative evaluation occurred, on average, 30.4 days prior to surgery. Baseline demographics and pertinent ocular characteristics (ie, central corneal thickness, corneal hysteresis, cup-to-disc ratio, mean standard deviation) were obtained from preoperative assessment. No protocol for preoperative glaucoma medication washout was specified. Thus, most eyes remained medically treated on the day of surgery.
Surgical Technique
The OMNI procedure performed in this study has been previously described.13,16,17 Briefly, a 1.8 mm clear corneal incision was made temporally, and the anterior chamber was filled with viscoelastic. The OMNI Surgical System was introduced into the anterior chamber and placed near the trabecular meshwork. A small otomy was performed. The microcatheter was then fed 180-degrees into Schlemm’s canal which was dilated with viscoelastic as the microcatheter was retracted. The same procedure was performed in the opposite hemisphere, completing 360-degrees of canaloplasty. The microcatheter was then fed 180-degrees into Schlemm’s canal and a 180-degree trabeculotomy was performed. Deviation from standard technique was minimal and attributable to surgeon preference; the vast majority receiving 360-degrees canaloplasty and 180-degrees trabeculotomy. Eyes that underwent OMNI in combination with cataract surgery or endoscopic cyclophotocoagulation were excluded.
Postoperative Follow-Up
A typical postoperative drop regimen, consisting of a topical steroid (prednisolone acetate 1%) for one month and antibiotic (ofloxacin 0.3% or gatifloxacin 0.5%) ± nonsteroidal anti-inflammatory (bromfenac 0.07%) for one week, was prescribed. The decision to continue preoperative glaucoma medications following surgery was based on patient’s preoperative assessment and surgeon discretion. No specific parameters were outlined for the postoperative addition or subtraction of ocular hypotensive medications. This decision was deferred to clinical judgment.
Postoperative data was collected at one day, one week, three months, and six months. The number and type of glaucoma medications used as well as the IOP were recorded at each postoperative timepoint. Combination glaucoma drops were reported in terms of their individual components. The preferred IOP measurement varied between clinical sites with the most common being Goldmann Applanation Tonometry (GAT) and corneal-compensated IOP (ccIOP) as measured by an Ocular Response Analyzer (ORA).
Outcome Measures
Primary outcome measures were mean IOP and number of glaucoma medication. Furthermore, surgical success was defined as either a 20% reduction in IOP without increase in glaucoma medication use, or discontinuation of at least one glaucoma medication without increase in IOP. This criterion was developed in accordance with prior trials13,18 and recommendations by the US FDA Guidance for Industry: Premarket Studies of Implantable MIGS Devices.
A safety index was determined using three surrogate markers – IOP spikes ≥10 mmHg above baseline, postoperative hyphema, and secondary surgical intervention. If hyphema was present at any postoperative timepoint, it was recorded regardless of clinical significance. Eyes requiring further glaucoma surgery due to uncontrolled IOP or glaucomatous progression were included in the cohort up until the point of secondary surgical intervention.
Statistical Analysis
All pseudophakic eyes having underwent a standalone OMNI procedure with postoperative data out to 6-months were included in the full data set. Missing data due to incomplete charting or a missed visit was treated as missing. To better account for absent data, a consistent cohort was established. The consistent cohort did not include eyes with secondary surgery or eyes with incomplete 6-month follow-up.
Baseline demographic and ocular characteristics were quantified using descriptive statistics. Postoperative IOP and glaucoma medication use were compared to their preoperative baseline using paired parametric t-tests. The rate of surgical success, defined above, was tabulated using consistent cohort data. To determine prognostic indicators of surgical success, preoperative ocular characteristics were compared using Pearson’s chi-square analysis and two-tailed independent t-tests. All analyses were completed using SPSS software (version 28.0, IBM Inc.) with an α level of 0.05 considered as statistically significant.
Results
Demographic and Preoperative Characteristics
This retrospective study included 67 eyes of 52 patients. Three participating clinical sites supplied patient information: Alexandria, Minnesota (30); Sioux Falls, South Dakota (24); Fargo, North Dakota (13). Relevant demographic data is summarized in Table 1. Note that the cohort was female predominant with the proportion of right and left eyes being similar.
 |
Table 1 Demographic and Preoperative Characteristics |
Most eyes had a preoperative diagnosis of POAG versus other secondary forms of open-angle glaucoma such as pseudoexfoliation (Table 1). Disease severity ranged from mild to severe with a mean visual field mean deviation of −8.7±7.8 dB and a mean cup-disc ratio of 0.7±0.2. Over half of eyes had undergone at least one prior glaucoma surgery, the most common being iStent alone (15 eyes) followed by iStent + ECP (6 eyes) then laser trabeculoplasty (10). Five eyes had a history of trabeculectomy. Despite the high incidence prior glaucoma surgery, average IOP remained (at preoperative baseline) 22.1 ± 8.0 mmHg on 2.3 ± 1.4 ocular hypotensive agents.
Efficacy
Surgical success was defined as an IOP reduction ≥20% compared to baseline without an increase in glaucoma medication burden, or discontinuation of at least one baseline glaucoma medication without concomitant increase in IOP above baseline. Out of the 43 eyes with 6-month postoperative data, 30 eyes (69.8%; 95% confidence interval, 53.9–82.8%) achieved success (Table 2). Twelve eyes experienced an IOP reduction ≥20% and medication reduction. Comparison of preoperative characteristics between surgical successes and failures found baseline IOP to be the only statistically different factor between groups (p = 0.04).
 |
Table 2 Comparison of Baseline Characteristics Between Surgical Successes and Failures |
Intraocular Pressure and Medication Reduction
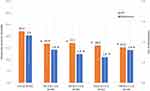
Preoperative IOP was 22.1±8.0 mmHg on 2.3±1.37 ocular hypotensive medications. At 6-months postoperative, average IOP was 15.2±4.9 mmHg (p < 0.001) demonstrating a statistically significant mean IOP reduction of 29% compared to baseline (Figure 1). IOP reduction was sustained across all postoperative time points. Eyes with a baseline IOP ≥22 mmHg experienced a 46.0% IOP reduction versus an 11.7% reduction observed in eyes with a baseline IOP <22 mmHg. Proportionally, 79% of eyes had an IOP ≤18 mmHg and 40% of eyes had an IOP ≤15 mmHg at 6-months (Figure 2).
 |
Figure 2 Proportion of eyes within complete data set achieving IOP ≤18 mmHg and ≤15 mmHg at all postoperative timepoints. |
Mean medication burden was significantly decreased at all postoperative timepoints. At 3 and 6-months, mean medication reduction was 1.0±1.3 and 0.7±1.4, respectively (p < 0.001). Significant reduction in glaucoma medication use was sustained throughout all postoperative timepoints with 19 eyes maintained on at least 1 less medication at 6-months compared to baseline. Sixteen eyes were medication free at 6-months.
Consistent cohort results were comparable with statistically significant primary outcome measures at all postoperative time points.
Subgroup Analysis
Consistent cohort data was utilized for subgroup analysis and included 16 eyes with severe glaucoma and 27 eyes with mild-moderate glaucoma (Table 3). Mean IOP was significantly higher for eyes with severe glaucoma compared to mild-moderate at both baseline and 6-months (p = 0.02; p = 0.03; Figure 3). Whereas mean ocular hypotensive use was similar between mild-moderate and severe glaucoma at baseline and 6-months (p = 0.53; p = 0.89; Figure 3). The mean percent reduction in IOP was 52% for severe versus 16% for mild-moderate (p < 0.001). Furthermore, surgical success rate was statistically different with 94% (95% confidence interval, 69.8–99.8%) of severe eyes meeting criteria compared to 56% (95% confidence interval, 35.3–74.5%) of mild-moderate (p = 0.01).
 |
Table 3 Primary Outcome Baseline Characteristics Stratified by Glaucoma Severity |
Safety Profile
No intraoperative complications were observed. Postoperative hyphema was the most frequent adverse event occurring in 26 eyes in the immediate postoperative period. IOP spikes ≥10 mmHg above baseline occurred at a rate of 5.1% 1-month after surgery. Two eyes underwent additional glaucoma surgery with a subconjunctival filtering procedure. The total number of adverse events was comparable to prior studies, suggesting an adequate safety profile.13
Discussion
This real-world, multi-center study evaluating the effectiveness of combined ab interno canaloplasty and trabeculotomy in pseudophakic eyes with open-angle glaucoma showed promising results. In this study, patients experienced a mean IOP reduction of 29% with 95% of eyes requiring the same number or fewer medications at 6-months. These findings parallel prior studies, which reported similar reductions in IOP and medication burden sustained out to 12 and 24-months.13,15 However, a key point of distinction is this study’s inclusion of pseudophakic eyes with severe glaucoma.
Subgroup analysis revealed a significantly greater reduction in mean IOP for eyes with severe glaucoma compared to mild-moderate glaucoma. Interestingly, mean glaucoma medication use remained similar at preoperative and 6-month timepoints for both mild-moderate and severe. This juxtaposition suggests that while a majority of eyes achieved similar medical control after surgery (ie, IOP <18), the greatest IOP reduction benefit was seen in eyes with higher baseline IOP mirroring other MIGS studies.19
IOP is the sole modifiable risk factor for glaucomatous progression. Strong, prospective evidence exists supporting the causal relationship between IOP and progression.18,20–23 The Early Manifest Glaucoma Trial reported that for every millimeter reduction in IOP, risk of progression was reduced by 10% in patients with mild-moderate glaucoma.20,21 Similarly, the Ocular Hypertension Treatment Study demonstrated the effectiveness of topical ocular hypotensive medications at delaying and, in some cases, preventing the conversion of ocular hypertension to glaucoma.23 Even in refractory glaucoma, IOP reduction has been shown to slow progression.18,22 However, IOP reduction in severe cases historically required classical surgical intervention (ie, trabeculotomy, tube shunt) posing a heightened level of risk.
With the advent of MIGS, glaucoma management has undergone a paradigm shift. MIGS has bridged the treatment gap, offering early and effective surgical options with lower associated risk compared to traditional drainage therapies. Initially, MIGS was marketed as an extension of medical therapy in the setting of nonrefractory glaucoma prompting the FDA to require rigorous safety testing for standalone procedures.24 To mitigate this, MIGS was approved in combined with cataract surgery where the risk of intraocular surgery was already justified.2 However, by doing so, the potential of MIGS was limited as the benefit of MIGS were not made available to pseudophakic eyes or eyes with severe glaucoma.
As evidence supporting the safety and efficacy of MIGS + cataract surgery continues to emerge, there is increased interest in the use of MIGS as a standalone option for pseudophakic eyes with poorly controlled primary open-angle glaucoma.2,25 The OMNI surgical system is the first and only MIGS procedure currently FDA cleared for standalone use. Compared to other MIGS, the OMNI surgical system addresses all three levels of aqueous outflow resistance without the use of an implant.26 The OMNI surgical system has the added benefit of combining two MIGS procedures, canaloplasty and trabeculotomy, into one. Thus, there is the potential for additional IOP and medication reduction especially in eyes that have already experienced the pressure lowering effects of cataract surgery.
In this study, 69.8% of pseudophakic eyes were considered a surgical success at 6 months (IOP reduction ≥20% compared to baseline without medication increase, or discontinuation of at least one baseline glaucoma medication without IOP increase). The ROMEO study defined success as a 20% reduction in IOP or an IOP between 6 and 18 mmHg at 12 months without a corresponding increase in glaucoma medication. Out of 48 pseudophakic eyes in that study, 72.9% met this criterion.13 The sole preoperative indicator of surgical success was baseline IOP. Interestingly, the correlation between baseline IOP and degree of IOP reduction was also highlighted in the first published results for the OMNI device.27 The proportion of surgical success was significantly different when stratified based on baseline glaucoma severity indicating that combined ab interno canaloplasty and trabeculotomy may provide some benefit in eyes with more extensive disease, especially in eyes with contraindications to traditional glaucoma surgery. The OMNI surgical system appears to provide substantial reduction in IOP and medication use for pseudophakic individuals open angle glaucoma irrespective of disease severity.
For MIGS to be considered as a standalone option, it must find an appropriate balance of efficacy and safety. In this study, few adverse events were observed. The most common was hyphema which occurred in 40% of eyes during the immediate postoperative period. While the clinical significance and severity of hyphema was not delineated, the rate reported was expected given the distortion of angle anatomy secondary to ab interno canaloplasty and trabeculotomy. Klabe et al evaluated postoperative outcomes of 38 eyes after standalone ab interno canaloplasty and trabeculotomy reporting a hyphema rate of 44.7% with none being >1 mm.15 Comparatively, only 4.2% of eyes included in the ROMEO study experienced clinically significant hyphema defined as layered and >1 mm and/or persisting >1 week and/or requiring secondary intervention.13 Only 2 eyes (3.0%) required additional surgery for IOP. This was less than the ROMEO study (10.4%) and the findings of Klabe et al (5.2%). All existing retrospective studies evaluating the OMNI surgical system and the preliminary, prospective findings of the ongoing ORION trial corroborate the safety profile demonstrated in this study.28
Interpretation of results is hindered by the retrospective nature of this study. Its multi-center design and lack of a standardized protocol leave much to clinical judgment. Additionally, without a comparable control group, findings should be interpreted with some caution. Despite these challenges, the study provides real-world evidence to suggest the safety and efficacy of combined ab interno canaloplasty and trabeculotomy in pseudophakic eyes with open angle glaucoma.
Conclusion
The MIGS revolution has shrunk the treatment gap within glaucoma management; however, opportunities for improved treatment options still exist. Specifically, there is growing evidence to suggest that pseudophakic individuals may benefit from the reduction in IOP provided by a standalone MIGS procedure. Yet, prior to widespread implementation safety and efficacy must be thoroughly evaluated. The results presented in this study corroborate the findings of other studies and suggest that combined canaloplasty and trabeculotomy might be a safe and effective means of managing pseudophakic eyes with uncontrolled open angle glaucoma.
Acknowledgments
Study was an Investigator Initiated Trial with research funding provided by Sight Sciences, Inc. (Menlo Park, CA).
Disclosure
The abstract of this paper was presented at the ASCRS 2021 Annual Meeting as a conference talk with interim findings. The abstract was published online [https://ascrs.org/clinical-education/abstracts/2021/efficacy-of-ab-interno-canaloplasty-followed-by-trabeculotomy-in-pseudophakic-eyes-with-openangle-gl]. Dr Mitch Ibach reports grants from Sight Sciences, during the conduct of the study; personal fees from Allergan, personal fees from Glaukos, personal fees from Sight Sciences, outside the submitted work. Mr Michael Greenwood reports personal fees from Sight Sciences, outside the submitted work. Dr Deborah Ristvedt reports personal fees from Allergan, personal fees from Glaukos, personal fees from Sight Sciences, personal fees from RxSight, outside the submitted work. Dr John P Berdahl reports personal fees from Equinox, personal fees from Glaukos, personal fees from New World Medical, personal fees from Sight Sciences, during the conduct of the study; personal fees from Abbvie, personal fees from Aerie, personal fees from Aerpio, personal fees from Aldeyra, personal fees from Aurea Medical, personal fees from CorneaGen, personal fees from Dakota Lions Eye Bank, personal fees, from Expert Opinion MD, personal fees from Gore, personal fees from Imprimis, personal fees from iRenix, personal fees from Iacta Pharmaceuticals, personal fees from Kala, personal fees from Kedalion, personal fees from MELT Pharmaceuticals, personal fees from MicroOptx, personal fees from Ocular Surgical Data, personal fees from Omega Ophthalmic, personal fees from Orasis, personal fees from Oyster Point, personal fees from Tarsus, personal fees from Surface INC, personal fees from Tear Clear, personal fees from Vertex Ventures, personal fees from ViaLase, personal fees from Vittamed, personal fees, from Vance Thompson Vision, personal fees from Verana Health, personal fees from Visionary Ventures, personal fees from Visus, outside the submitted work. Dr Daniel C Terveen reports grants from Sight Sciences, during the conduct of the study; grants from Sight Sciences, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Prum BE, Rosenberg LF, Gedde SJ, et al. Primary open-angle glaucoma preferred practice pattern(®) guidelines. Ophthalmology. 2016;123(1):P41–P111. doi:10.1016/j.ophtha.2015.10.053
2. Saheb H, Ahmed II. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012;23(2):96–104. doi:10.1097/ICU.0b013e32834ff1e7
3. Ahmed SF, Bhatt A, Schmutz M, Mosaed S. Trabectome outcomes across the spectrum of glaucoma disease severity. Graefes Arch Clin Exp Ophthalmol. 2018;256(9):1703–1710. doi:10.1007/s00417-018-4023-8
4. Mäepea O, Bill A. Pressures in the juxtacanalicular tissue and Schlemm’s canal in monkeys. Exp Eye Res. 1992;54(6):879–883. doi:10.1016/0014-4835(92)90151-H
5. Allingham RR, de Kater AW, Ethier CR. Schlemm’s canal and primary open angle glaucoma: correlation between Schlemm’s canal dimensions and outflow facility. Exp Eye Res. 1996;62(1):101–109. doi:10.1006/exer.1996.0012
6. Battista SA, Lu Z, Hofmann S, Freddo T, Overby DR, Gong H. Reduction of the available area for aqueous humor outflow and increase in meshwork herniations into collector channels following acute IOP elevation in bovine eyes. Invest Ophthalmol Vis Sci. 2008;49(12):5346–5352. doi:10.1167/iovs.08-1707
7. Grover DS, Godfrey DG, Smith O, Feuer WJ, Montes de Oca I, Fellman RL. Gonioscopy-assisted transluminal trabeculotomy, ab interno trabeculotomy: technique report and preliminary results. Ophthalmology. 2014;121(4):855–861. doi:10.1016/j.ophtha.2013.11.001
8. Francis BA, See RF, Rao NA, Minckler DS, Baerveldt G. Ab interno trabeculectomy: development of a novel device (Trabectome) and surgery for open-angle glaucoma. J Glaucoma. 2006;15(1):68–73. doi:10.1097/01.ijg.0000196653.77836.af
9. Seibold LK, Soohoo JR, Ammar DA, Kahook MY. Preclinical investigation of ab interno trabeculectomy using a novel dual-blade device. Am J Ophthalmol. 2013;155(3):524–529.e2. doi:10.1016/j.ajo.2012.09.023
10. Gallardo MJ, Supnet RA, Ahmed IIK. Viscodilation of Schlemm’s canal for the reduction of IOP via an ab-interno approach. Clin Ophthalmol. 2018;12:2149–2155. doi:10.2147/OPTH.S177597
11. Tracer N, Dickerson JE, Radcliffe NM. Circumferential viscodilation ab interno combined with phacoemulsification for treatment of open-angle glaucoma: 12-month outcomes. Clin Ophthalmol. 2020;14:1357–1364. doi:10.2147/OPTH.S252965
12. Grabska-Liberek I, Duda P, Rogowska M, et al. 12-month interim results of a prospective study of patients with mild to moderate open-angle glaucoma undergoing combined viscodilation of Schlemm’s canal and collector channels and 360° trabeculotomy as a standalone procedure or combined with cataract surgery. Eur J Ophthalmol. 2021:1120672121998234. doi:10.1177/1120672121998234
13. Vold SD, Williamson BK, Hirsch L, et al. Canaloplasty and trabeculotomy with the OMNI system in pseudophakic patients with open-angle glaucoma: the ROMEO Study. Ophthalmol Glaucoma. 2021;4(2):173–181. doi:10.1016/j.ogla.2020.10.001
14. Hirsch L, Cotliar J, Vold S, et al. Canaloplasty and trabeculotomy ab interno with the OMNI system combined with cataract surgery in open-angle glaucoma: 12-month outcomes from the ROMEO study. J Cataract Refract Surg. 2021;47(7):907–915. doi:10.1097/j.jcrs.0000000000000552
15. Klabe K, Kaymak H. Standalone trabeculotomy and viscodilation of Schlemm’s canal and collector channels in open-angle glaucoma using the OMNI surgical system: 24-month outcomes. Clin Ophthalmol. 2021;15:3121–3129. doi:10.2147/OPTH.S325394
16. Pyfer MF, Gallardo M, Campbell A, et al. Suppression of diurnal (9AM-4PM) IOP fluctuations with minimally invasive glaucoma surgery: an analysis of data from the prospective, multicenter, Single-Arm GEMINI Study. Clin Ophthalmol. 2021;15:3931–3938. doi:10.2147/OPTH.S335486
17. Toneatto G, Zeppieri M, Papa V, et al. 360° Ab-interno schlemm’s canal viscodilation with OMNI viscosurgical systems for open-angle glaucoma-midterm results. J Clin Med. 2022;11(1):259. doi:10.3390/jcm11010259
18. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration.The AGIS Investigators. Am J Ophthalmol. 2000;130(4):429–440. doi:10.1016/s0002-9394(00)00538-9
19. Ferguson TJ, Dockter Z, Bleeker A, et al. iStent inject trabecular microbypass stent implantation with cataract extraction in open-angle glaucoma: early clinical experience. Eye Vis. 2020;7:28. doi:10.1186/s40662-020-00194-3
20. Heijl A, Leske MC, Bengtsson B, Hyman L, Hussein M. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120(10):1268–1279. doi:10.1001/archopht.120.10.1268
21. Leske MC, Heijl A, Hyman L, Bengtsson B. Early Manifest Glaucoma Trial: design and baseline data. Ophthalmology. 1999;106(11):2144–2153. doi:10.1016/s0161-6420(99)90497-9
22. Feiner L, Piltz-Seymour JR, Study CIGT. Collaborative Initial Glaucoma Treatment Study: a summary of results to date. Curr Opin Ophthalmol. 2003;14(2):106–111. doi:10.1097/00055735-200304000-00010
23. Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):
24. Ahmed II. MIGS and the FDA: What’s in a name? Ophthalmology. 2015;122(9):1737–1739. doi:10.1016/j.ophtha.2015.06.022
25. Kerr NM, Wang J, Barton K. Minimally invasive glaucoma surgery as primary stand-alone surgery for glaucoma. Clin Exp Ophthalmol. 2017;45(4):393–400. doi:10.1111/ceo.12888
26. Dickerson JE, Brown RH. Circumferential canal surgery: a brief history. Curr Opin Ophthalmol. 2020;31(2):139–146. doi:10.1097/ICU.0000000000000639
27. Brown RH, Tsegaw S, Dhamdhere K, Lynch MG. Viscodilation of Schlemm canal and trabeculotomy combined with cataract surgery for reducing intraocular pressure in open-angle glaucoma. J Cataract Refract Surg. 2020;46(4):644–645. doi:10.1097/j.jcrs.0000000000000107
28. Gallardo M, Sarkisian SR, Singh IP, Flowers B, Vold SD, Samuelson T. Ab-interno canaloplasty and trabeculotomy in pseudophakic eyes with mild-moderate open angle glaucoma: prospective multicenter trial (ORION). ASCRS 2021; 2021.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.